Recurrent respiratory papillomatosis (RPP) is a rare benign neoplasm caused by human papillomavirus (HPV). RPP is characterized by recurrent proliferation of the papillomata in the respiratory tract.
Objectives and methodsRetrospective analysis of all adult patients with diagnosis of recurrent respiratory papillomatosis admitted to our endoscopic unit between 2000 and 2013 with histological proved papillomatosis.
ResultsFour patients were included (3 women) with an average age of 53±19 years (27–72). Before endoscopy unit admission, all the patients have been previously submitted to surgical removal of the papillomas with a median number of surgeries per patient of 6.5. These patients were submitted to therapeutic endoscopy and the most frequent endoscopic treatments were Laser YAG and local injection of cidofovir. All the patients treated with cidofovir presented complete remission of the disease. The median follow-up was 6 years: 2 presented malignant transformation to epidermoid carcinoma and 1 had severe dysplasia on the histological examination. We describe the four cases due to different forms of presentation.
ConclusionPapillomatosis of the airway is a rare condition predisposing to malignant transformation. RRP tends to recur and repeated surgeries are needed to remove papillomatas. Endoscopic treatment is important for the removal of the papillomas that are not accessible via laryngoscopy (YAG Laser, cryotherapy, etc.) and for resistant moderate/severe cases of RPP because it allows intralesional administration of adjuvant therapy like cidofovir.
Recurrent respiratory papillomatosis (RPP) is a rare benign neoplasm caused by human papillomavirus (HPV) with no known cure. RPP is characterized by recurrent proliferation of the papillomata in the respiratory tract and can occur in both children and adults. The juvenile form is more frequent and more aggressive requiring repeated surgeries.1
In this article we review the experience of our endoscopic unit by a retrospective analysis of the patients with a confirmed diagnosis of recurrent respiratory papillomatosis followed by the discussion of all the clinical cases, due to different forms of presentation and outcome.
Material and methodsAdult patients with recurrent respiratory papillomatosis admitted to our endoscopic unit between 2000 and 2013 were reviewed retrospectively.
The following variables were analyzed: sex, age, presenting symptoms, number and anatomic location of the papillomas, serotype of HPV, surgical procedures, other treatment modalities before bronchoscopy, endoscopic treatment, complete or partial remission, complications of the endoscopic treatment, malignant transformation and mortality.
ResultsFour patients were included: 3 women and 1 man. The average age was 53±19 years ranging from 27 to 72 years.
Two patients were smokers. No information regarding maternal genital HPV infection or sexual behavior was available. Serologic screening of patients for HIV-1 or HIV-2 was negative in all the patients. One patient had a history of breast and uterus tumor.
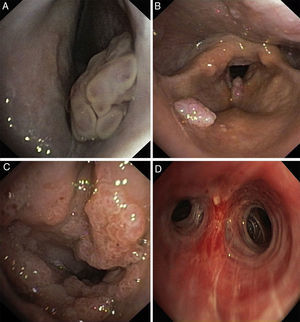
One patient had an epiglottis and vocal cord involvement and 3 patients had more extensive lesions: larynx and trachea in one case, pharynx, larynx and trachea in another case and one with a more exuberant and extensive form involving nasal cavity, pharynx, larynx, trachea and bronchus (Figs. 1–7).
Symptoms included hoarseness in three patients, dyspnea in two patients and stridor in one patient.
HPV detection by polymerase chain reaction was documented in three patients. One patient was infected with serotype 11, another with serotype 11 and 70 and another with serotype 16. In one patient, HPV was not available.
The four patients had been previously treated in the Ear Nose Throat (ENT) department where they were submitted to several treatments with CO2 laser vaporization and debulking with microdebrider, with an average of 6.5 treatments per patient. In one case transitory systemic treatment with Interferon was tried and stopped due to serious adverse effects.
Due to an impending respiratory failure, one patient had been submitted to an emergency tracheostomy (in another institution).
In our department, all the patients were submitted to diagnostic and therapeutic bronchoscopy for their papillomatosis (Figs. 2, 4 and 7B). Depending on the location, degree of obstruction, extension and number of the lesions, multiple and combined procedures were needed accordingly. Neodymium yttrium aluminum garnet (Nd:YAG) laser and electrocautery were used for hemorrhagic lesions, wire loop electrocautery was used for polyploid papillomatas with cryotherapy at the tumor base to prevent regrowth. Due to the rapid recurrence rate, local administration of cidofovir at the base of the lesions was also tried.
All the four patients had recurrence of the disease and were treated using the aforementioned bronchoscopic treatments, with a median disease recurrence free time of 3.5 months.
Three patients with disease recurrence were ultimately treated with intralesional administration of cidofovir. Cidofovir was administrated with an injection needle (metal sheath injection needles – NM-8L-1, Olympus®) inserted through the bronchoscope. Total dose was dependent on the extension of the base of papilloma, with an interval of 2–4 weeks. Patients needed a median of 2 administrations to achieve clinical improvement and 5 administrations on average for complete long term remission of the disease. Complete remission was achieved in the four patients without any complications. Two patients needed a second treatment course for a definitive remission of the disease until the present. The median follow-up was 6 years.
Two patients developed malignant transformation of the papillomata and another patient developed mild to severe laryngeal dysplasia. One patient infected with serotype 11 had an epidermoid carcinoma of the oropharynx and right tonsil. The other patient, infected by serotype 16 had a polytopic epidermoid carcinoma of the oropharynx, larynx and trachea. One patient, infected with serotype 11 and 70 had stable severe dysplasia of the larynx, with no progression to carcinoma, during the 6 year follow-up.
Of the 4 patients treated in our Department, one died after external beam radiotherapy, due to progression of the larynx epidermoid carcinoma.
The four cases, with different forms of presentation and outcome, are presented in Table 1.
Summary of the 4 clinical cases of recurrent respiratory papillomatosis treated in the endoscopic unit.
| Case 1 | Case 2 | Case 3 | Case 4 | |
|---|---|---|---|---|
| Sex | Male | Female | Female | Female |
| Age | 47 | 69 | 27 | 56 |
| History of cancer | None | Uterus and breast cancer | None | None |
| Location of papillomas | Nasal fossa, left conjunctival sac, larynx and bronchus (Fig. 1) | Larynx, trachea | Larynx: vocal cords, epiglottis | Larynx, trachea |
| HPV serotype | HPV 11 | HPV 16 | Not available | HPV 11 and 70 |
| Previous ENT treatments | 7 surgical excisions with CO2 laser of the nasal and pharynx–larynx papillomas | None | 9 surgeries of the larynx papillomas (microdebrider and laser YAG) | Multiple surgeries of the larynx (microdebrider and laser YAG) |
| Tracheostomy (in another hospital) because of severe airway compromise | ||||
| Presenting symptoms | Dyspnea | Stridor and dyspnea | Hoarseness | Dyspnea, hoarseness |
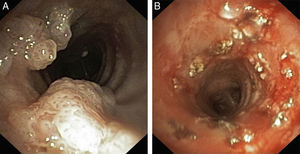
| Endoscopic findings | Multiple polyploid papillomas in the nasal fossa, pharynx, larynx and proximal trachea | Larynx papillomas | Papilloma of the left vocal cord | Multiple polypoid papillomas of the larynx and proximal trachea (Figs. 6 and 7) |
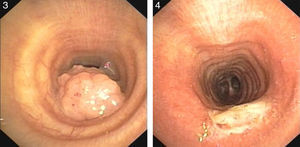
| Significant obstruction of the trachea (>80%) | Exophytic mass obstructing 80% of the tracheal lumen (Fig. 3) | |||
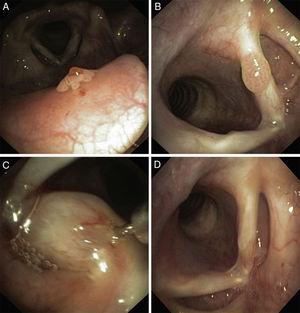
| 1° line endoscopic treatment | Removal of the tracheal mass by an electrocoagulation snare | Removal of the tracheal mass by an electrocoagulation snare (Fig. 4) | Intralesional administration of cidofovir at the left vocal cord (Fig. 5) | Nd:YAG laser vaporization in the larynx and tracheal lesions (Fig. 8) |
| Coagulation of the tracheal tumor base with Nd:YAG laser (Fig. 2) | Photocoagulation of the tracheal lesions with Nd:YAG laser (Fig. 4) | No complications | Local administration of cidofovir at the base of the tracheal papillomas | |
| Results of the 1° line endoscopic treatment | Tracheal papilloma relapse | Tracheal papilloma relapse | Papilloma relapse in the right vocal cord and epiglottis (Fig. 5) | Tracheal papilloma relapse |
| 2° line endoscopic treatment | Laser vaporization and cryotherapy of the tracheal lesions | Electrocoagulation and cryotherapy of the tracheal lesions | Intralesional administration of cidofovir at the vocal cords and epiglottis | 2 treatment with cidofovir at the base of the tracheal papillomas |
| No complications | ||||
| Results of the 2° line endoscopic treatment | Tracheal papilloma relapse | Tracheal papilloma relapse | Remission of the larynx papillomatosis | Complete resolution of the papillomas. |
| Papillomatosis spread to apical segment of right upper lobe bronchus (B1) | No complications | |||
| 3° line endoscopic treatment | Intralesional administration of Cidofovir in the tracheal lesions | Electrocoagulation and cryotherapy of the tracheal lesions | ||
| Cryotherapy in the bronchus papilloma | ||||
| Result of the 3° line endoscopic treatment | No regrowth of the tracheal and bronchus papillomas | |||
| Malignant transformation | Epidermoid carcinoma of the oropharynx and tonsil with a cervical metastasis | Epidermoid carcinoma of larynx and trachea | None | Mild to severe dysplasia of the larynx, which remain stable on a 6 year follow-up. |
| Outcome | Undergone cervical external beam radiotherapy treatment. The patient is still alive. | Refused surgery. She died due to tumor progression. | After 4 years of follow-up, no further recurrence was observed. | No progression to carcinoma. Tracheotomy was closed. |
Recurrent respiratory papillomatosis (RPP) is a rare disease caused by human papillomavirus (HPV), characterized by the presence of recurrent growth of benign papillomatas within the respiratory tract.1 The estimated incidence is 2 per 100,000 in adults and 4 per 100,000 in children.2 Two clinical patterns are described: the adult and the juvenile form. The juvenile form is considered to be more aggressive and 75% are diagnosed before the age of 5. The adult form has a slight male predominance with the peak age between 20 and 40 years.
RPP is more common in the larynx, particularly in the vocal folds and rarely involves the trachea or bronchus. In our series the larynx was the most affected by RPP especially the glottic area but trachea was also frequently involved. We also had a patient with involvement of the entire respiratory tract: from nasal fossa to bronchus.
Patients with RPP usually present symptoms of airway involvement like progressive hoarseness, stridor, dyspnea, acute respiratory distress or chronic cough. The average time from onset of the symptoms and diagnosis ranges from 1 to 8 years. In our patients the most frequent symptoms were hoarseness and dyspnea, revealing obstructive compromise of the airway by the papillomata.
Nearly 110 different HPV types have been identified but the most frequent serotypes are type 6 and 11, the same that cause genital condiloma.3 Although it is a benign neoplasm, RPP can undergo malignant transformation, increasing morbidity and mortality.4 HPV serotypes are classified according to risk of malignization: low risk (like serotype 6 and 11), moderate risk and high risk of malignization (HPV 16, HPV 18, etc.).
In our population, serotype 11 was the most frequent. Curiously, malignant transformation and severe dysplasia occurred in 2 patients infected with serotype 11 which is usually considered a low risk of malignization serotype. Both patients with malignant transformation presented with an epidermoid carcinoma.
There is no known cure for RPP but ENT surgery remains the mainstay of treatment with a goal of complete removal of the papillomas and preservation of the normal structures. The preferred methods are resection using microdebrider or CO2, Nd:YAG or pulse-dye Laser.6,7
As RPP tends to recur, most of the patients require repeated surgeries and complications like web formations, subglottic and glottic stenosis can severely compromise the airway and lead to the need for a tracheostomy.1
In our series, one patient had had an emergency, life-saving tracheotomy. It has been suggested that tracheotomy may activate or contribute to the spread of disease lower in the respiratory tract.5 Therefore, most authors agree that tracheotomy is a procedure to be avoided unless absolutely necessary, and, when a tracheotomy is absolutely necessary, decannulation should be considered as soon as possible, once the disease is controlled and the airway stabilized.
Our population of adult patients with RPP had undergone repeated surgeries (6.5 per patient) before admission to our endoscopic unit and the most frequent treatments were CO2 Laser and microdebrider.
However, when surgical therapy is needed more than four times in 12 months, adjuvant medical therapy should be considered. It is estimated that up to 20% of the patients need adjuvant therapy.8
Adjuvant therapies used for RPP include interferon, cidofovir, indole-3-carbinol, ribavirin and acyclovir. As a rare disease there is a serious lack of large population studies to prove the efficacy of these drugs. Up to now, the most extensively investigated adjuvant therapies are interferon-alpha (1990) and cidofovir (2000).
Subcutaneous interferon was first introduced in 1990 but has been recently replaced by cidofovir due to severe associated drug toxicity.9,10
Cidofovir is a recent antiviral drug, a nucleoside analog, approved by the FDA (Food and Drug Administration) for intravenous use to treat cytomegalovirus retinitis in patients with acquired immunodeficiency syndrome. Although it has not been approved for intralesional administration, cidofovir has been used to treat RPP since 1998, with promising results.
Intralesional cidofovir should be started when surgical debulking is required every 2–3 months. Administration should remain below to the established safety limits of dosing (3mg/kg) and volume.11,9,12–17
Its safety profile has recently been debated because of a possible eventual oncogenic potential but that risk has not been confirmed by recent human studies and it has been recommended for the treatment of moderate to severe RPP.19–21 However, high-quality data are needed and so informed consent (including discussion of off-label use and acute kidney injury, especially in children), is mandatory.
In our experience, intralesional cidofovir provided complete remission of the papillomatosis, in all the treated lesions, reducing the number of surgeries and improving the quality of life. We had no complications with cidofovir. One patient treated with cidofovir in the tracheal lesions developed mild to moderate dysplasia of the larynx, where the drug had never been injected (case 4). In another case (case 1), cidofovir was administrated in tracheal lesions and the epidermoid carcinoma developed in preexisting pharyngeal papillomatas, again in lesions never treated with the drug (case 1). A possible relationship between local administration of cidofovir and malignant transformation of the papillomatosis seems unlikely.
ConclusionPapillomatosis of the airway is a rare condition that can be life-threatening and become malignant. Bronchoscopic treatment is important for the removal of the papillomas which are not accessible by laryngoscopy (YAG Laser, cryotherapy, electrocoagulation) and for resistant moderate/severe cases of RPP because it allows intralesional administration of efficient adjuvant therapy like cidofovir.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.