Chronic and progressive dyspnea, the most characteristic symptom of chronic obstructive pulmonary disease (COPD), is often associated with physical activity reduction, not only because of the symptom itself but also because of the anticipation of discomfort caused by physical exertion.1,2 Fatigue is also one of the main symptoms, described as the second most prevalent.1,3 Therefore, relief of these symptoms is one of the primary goals in the management of patients with COPD.2
It is known that FEV1 is not useful in predicting dyspnea and some studies have evaluated the relationship between dyspnea and dynamic hyperinflation.1,4 Similarly, despite exercise-induced oxygen desaturation being observed in patients with COPD, mostly in those with more severe disease and with predominant emphysema phenotype, the underlying mechanism remains poorly understood.5 Also, limb muscle dysfunction may play an important role in exercise limitation.3
As far as we know, no previous study has evaluated the relationship between dyspnea and oxygen saturation (SpO2), nor between leg discomfort and distance walked.
The aims of this study were to investigate the association between dyspnea and SpO2, and between leg discomfort and distance walked in the 6-minute walk test (6MWT), as well as the impact of Pulmonary Rehabilitation (PR) program on these variables.
This was a longitudinal retrospective study of patients with COPD who completed an outpatient PR program during 2016 at Pulmonology Department of Centro Hospitalar Universitário Lisboa Norte, Portugal. Subjects attended a multicomponent PR program with patient-tailored therapies, 8–16 weeks long. Those with ambulatory oxygen supplementation maintained it during the 6MWT and exercise training.
At the beginning and at the end of PR program, all patients underwent 6MWT. The variables analyzed were the degree of dyspnea and leg discomfort at the end of each 6MWT according to Modified Borg Scale, minimum SpO2 observed by pulse oximeter and distance walked during the test.
Using software SPSS®, Wilcoxon or Student´s T-test were carried out, as appropriate, for comparison of variables at the beginning and at the end of the program. Associations were assessed using Spearman´s coefficient, considering significant p-values below 0.05.
Forty-six subjects with COPD completed the PR program, whose baseline characteristics are summarized in Table 1. Thirty-seven percent of them were on long-term oxygen therapy and 28.3% were on nocturnal noninvasive ventilation.
Baseline characteristics of the subjects.
| Characteristics | Results |
|---|---|
| Male n (%) | 37 (80.4) |
| Age (mean in years ± SD) | 68±10 |
| BMI (mean in kg/m2 ± SD) | 25.7±4.9 |
| Current/former smoker n (%) | 44 (95.7) |
| Comorbidities | |
| Arterial hypertensionn (%) | 29 (63) |
| Sleep obstructive apnea n (%) | 9 (20) |
| Bronchiectasis n (%) | 9 (20) |
| Anxiety/depression n (%) | 9 (20) |
| Atrial fibrillation n (%) | 6 (13) |
| Structural heart disease n (%) | 6 (13) |
| Pulmonary hypertension n (%) | 5 (10.9) |
| Charlson Comorbidity Index | |
| (mean±SD) | 3.9±1.5 |
| GOLD airflow limitation severity | |
| GOLD 1 n (%) | 4 (8.7) |
| GOLD 2 n (%) | 16 (34.8) |
| GOLD 3 n (%) | 19 (41.3) |
| GOLD 4 n (%) | 7 (15.2) |
| GOLD ABCD | |
| GOLD B n (%) | 22 (47.8) |
| GOLD D n (%) | 24 (52.2) |
| FEV1 post BD (mean in % ± SD) | 48.7±19.2 |
| FVC post BD (mean in % ± SD) | 83.4±21.8 |
| DLCO (mean in % ± SD) | 48.6±20 |
| Respiratory failure | |
| No respiratory failure n (%) | 4 (8.7) |
| Hypoxemic n (%) | 34 (73.9) |
| Hypercapnic n (%) | 8 (17.4) |
| Dyspnea | |
| mMRC 2 n (%) | 30 (65.2) |
| mMRC 3 or 4 n (%) | 16 (34.8) |
Legend: SD=standard deviation; BMI=body mass index; GOLD=Global Initiative Obstructive Lung Disease; FEV1=forced expiratory volume in one second; BD=bronchodilator; FVC=forced vital capacity; DLCO=diffusing capacity: mMRC=modified Medical Research Council Dyspnea Scale.
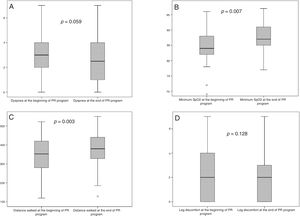
At the beginning and at the end of the PR program the mean degree of dyspnea was 3±1.8 and 2.5±1.7, and mean minimum SpO2 value was 84.9±5.4% and 87.6±4.3%, respectively. Only SpO2 improved significantly (p=0.007) (Fig. 1A and 1B). We observed no correlation between the degree of dyspnea and minimum SpO2, neither in the initial 6MWT (p=0.31) nor in the final one (p=0.09).
The mean distance walked was 340.7±105 and 373.3±95m in the initial and final 6MWT, respectively, with significant improvement (p=0.003) (Fig. 1C). The degree of leg discomfort reported in the initial and final 6MWT had a median value of 2±3 with no significant improvement after PR (p=0.128) (Fig. 1D). We observed a mild (rho=0.308) but significant (p=0.04) correlation between leg discomfort and distance walked in the initial 6MWT, but not in the final one (p=0.077).
This study shows the benefit of PR programs in patients with COPD, namely in oxygen saturation and exercise capacity. Similarly, previous studies evidenced improvement in arterial oxygenation with breathing techniques such as pursed lips breathing during exercise training, with physiological and clinical significance indicating its possible effect in decreasing airway collapse and respiratory rate.6
The multifactorial nature of dyspnea is well known and we observed no correlation between the degree of dyspnea and oxygen saturation. The maintenance of dynamic hyperinflation, airflow limitation and respiratory muscle weakness, leading to an increased mechanical load and a neuromechanical dissociation, might explain in part this absence of correlation and the lack of significant improvement in dyspnea.1,4 Peripheral muscle dysfunction, frequent in patients with COPD, also enhances exertional dyspnea and exercise intolerance.2,3 Those patients often have an augmented lactic acid production for a given exercise work rate, increasing their ventilatory demand.2,3
After PR program, our subjects reported a similar degree of leg discomfort for a significantly greater distance walked (32.6m). This is in line with extensive evidence showing improvement in exercise tolerance with a significant increment in distance walked by patients with COPD during 6MWT after PR program.7
Our findings reflect the multifactorial essence of dyspnea and fatigue as the most prevalent characteristics of patients with COPD, and the need for future research to clarify the underlying effects of PR on them.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interestNone.