M. tuberculosis infection remains a highly relevant topic worldwide and it is estimated that approximately 25% of the population is infected, with 95% of cases occurring in developing countries1.
The manifestations of tuberculosis can be divided into pulmonary and extrapulmonary, the latter occurring in approximately 15% of cases2. Skin involvement in tuberculosis is rare, and represents less than 2% of extrapulmonary manifestations3.
The main agent responsible for the skin lesions is Mycobacterium tuberculosis, but they can also be caused by M. bovis or the BCG vaccine4. They can manifest as inflammatory papules, verrucous plaques, chronic ulcers or suppurative nodes, as in the case presented3. This variety results from the mechanism of entry of M. tuberculosis into the skin (autoinoculation, exogenous inoculation or hematogenous route) 5, the patient's immune status, sensitization of the host to the agent 3, factors inherent to the host such as age, sex and race, and environmental factors such as climate and geographic location 4.
Skin lesions are essentially divided into true cutaneous TB, a direct result of infection, and tuberculids, indicating hypersensitivity to M. tuberculosis antigens3. Sarcoidosis, abscesses, and nontuberculous infections are common differential diagnoses3. The diagnosis can be challenging, culture and histological study must be performed, histopathology can show nonspecific inflammation, without the formation of granulomas5. The definitive diagnosis is confirmed by a positive culture for M. tuberculosis3.
The authors present the case report of a 75-year-old independent man who visited his Assistant Physician due to a 6-month history, approximately, of multiple, recurrent, suppurating skin lesions in the right and left supraclavicular regions and upper thoracic regions.
On physical examination, the lesions had painless, granulomatous ulcer with a fibrinous base and the patient had another abscess next to the sternocleidomastoid muscle. He also showed signs of collateral circulation (Fig. 1).
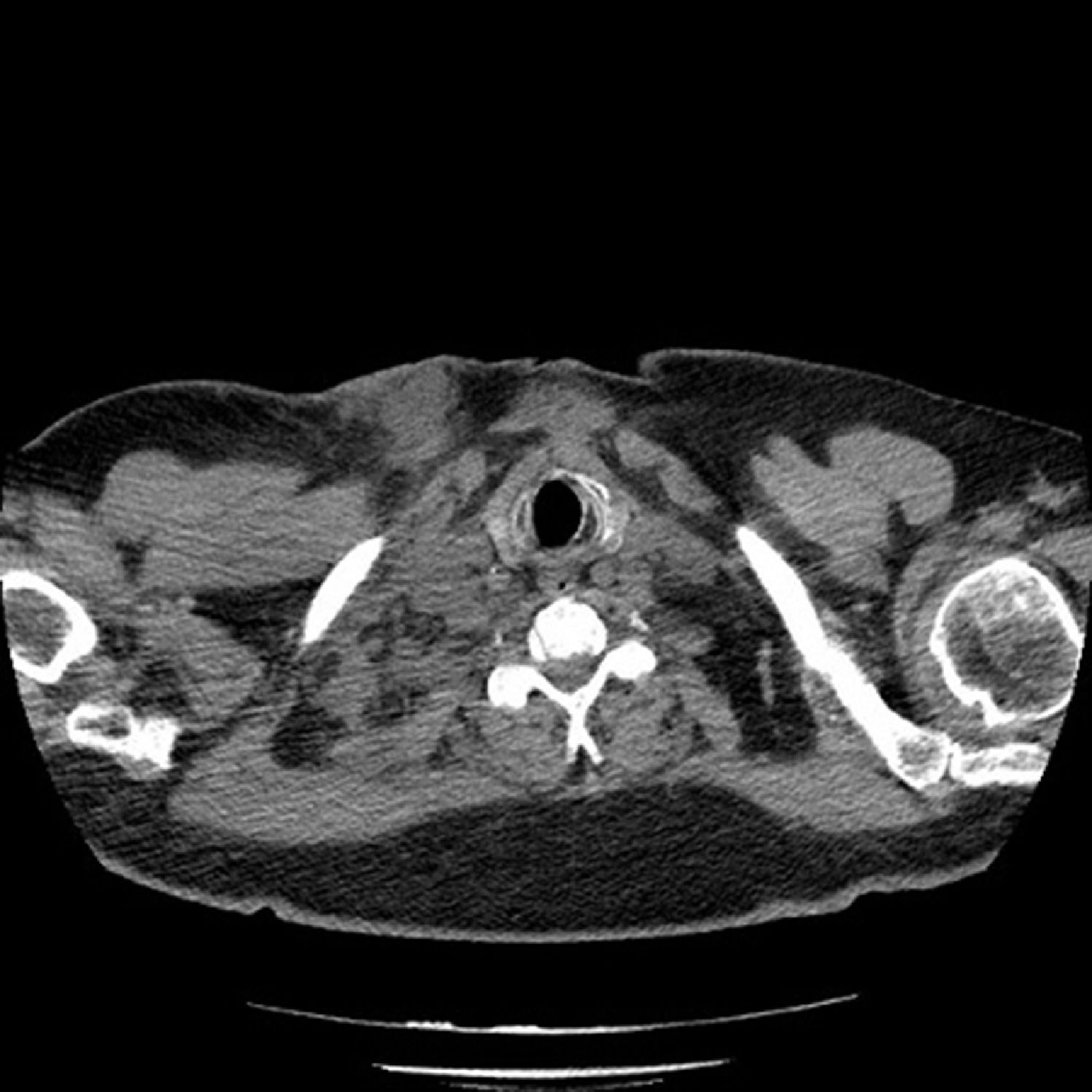
This was immunocompetent patient with no relevant medical history and no usual chronic medication. Laboratory results showed a slight increase in inflammatory markers (PCR 5.81 mg/dl) with negative procalcitonin and serum tumor markers. Computed tomography of the neck and chest showed several abscesses, namely in the right and posterior lateral cervical region and in the right supraclavicular cavity (Fig. 2), there was no pulmonary involvement. The patient underwent a video bronchial fibroscopy that showed no endobronchial lesions; the microbiology and cytology of the aspirate and bronchoalveolar lavage were negative.
The abscess in the right supraclavicular cavity was aspirated. The cytology revealed a necrotic area with an associated inflammatory process and the culture in Loewenstein-Zensen medium was positive for Mycobacterium tuberculosis. The patient was sent to the Pneumology Diagnosis Center (CDP) and began treatment with the four initial antitubercular drugs (isoniazid 300 mg/day, rifampin 600 mg/day, pyrazinamide 1500 mg/day and ethambutol 1200 mg/day).
The treatment is similar to that of systemic tuberculosis, with tuberculostatic drugs3, and biopsies or surgical debridement may sometimes be necessary5. With the exception of disseminated miliary cutaneous forms, skin lesions respond well to treatment and have a good prognosis 5.
With this case, the authors intend to show a rare form of a condition that still has a very negative impact on World Public Health, reinforcing the need to maintain strong clinical suspicion 3,5 so as not to delay the start of effective therapy.
FundingThe authors declare that no funding was received for this paper.
IMAGES: Show me your skin and I will tell you who you are