Solitary endobronchial papillomas (SEPs) are rare non-invasive tumours mainly described as case reports. They exhibit a broad spectrum of clinical presentations and therefore, misdiagnosis is not uncommon.1 Still, prompt diagnosis and early treatment are mandatory due to the risk of malignancy, which has been associated to squamous cell subtype, human papilloma virus (HPV) infection, smoking and age greater than 40 years.2,3
We report a case of a 52-year-old man, heavy-smoker and drinker, referred to a follow-up appointment two months after being admitted for Streptococci pneumonia at our pulmonology ward. His past medical history revealed oligophrenia, chronic bronchitis and an episode of lower limbs erysipela.
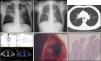
He had recent complaints of productive cough and minor bleeding sputum. Physical examination was unremarkable and routine blood sample analysis was normal. Chest X-ray showed significant improvements when compared to the initial abnormal findings, but showed a linear opacity at the horizontal fissure of the right lung and a heterogeneous and poorly defined opacity located above the left hilum. Chest computed tomography described fibrotic lesions at the upper right lobe, diffuse thickened bronchial walls and small bronchiectasis in the anterior segment of the upper left lobe. Positron-emission tomography reported a mild increase of metabolic activity in the right hilum region. Videobronchoscopy revealed a bleeding cauliflower lesion on the posterior segment of the right upper bronchus and minor hematic secretions. Bronchial biopsies disclosed bronchial squamous papilloma with moderate metaplasia, cellular atypia and moderate dysplasia of the respiratory epithelium (Fig. 1).
Chest X-ray before (A) and after (B) antibiotic treatment for pneumococci pneumonia. (C) Computed tomography scan showing diffuse thickened bronchial walls and small bronchiectasis in the upper left lobe. (D) Positron-emission tomography/Computed tomography with 18-fludeoxyglucose (FDG) displaying increased metabolic activity in the right hilum region. On bronchoscopic examination (E), a cauliflower lesion was observed on the posterior segment of the right upper bronchus. (F) High-power microscopic appearance of fibrovascular cores surrounded by squamous epithelium (original magnification 100×, haematoxylin and eosin stain).
HPV DNA has been detected in almost half of the squamous cell papillomas reported so far, why some consider SEPs as HPV-related neoplasms.3,4 Nevertheless, as we could verify in our case, detection by in situ hybridization is frequently negative.
Treatment options should consider the possibility of malignant transformation. Lung resection surgery or endoscopic removal of the lesion followed by close monitoring of the patient, are equally acceptable alternatives.2 However, some authors favour lung-sparing procedures due to previous descriptions of malignant involvement at distant sites of the lung.2,5,6 Our patient underwent endoscopic treatment with rigid bronchoscopy and neodymium-YAG laser. A fibreoptic bronchoscopy performed two weeks after the procedure confirmed complete destruction of the endobronchial lesion. Ultimately, the best treatment should be considered on an individual basis but, in our experience, bronchoscopy is a good and reasonable alternative treatment.