Postpartum spontaneous pneumomediastinum (Hamman's Syndrome) is a well-known but rare complication of pregnancy which is potentially lethal. However, current international pneumothorax guidelines do not give any advice on the management of this life-threatening event.1–4
We report the case of a 30-year-old woman who came to our attention at the 40th week of her pregnancy. She was a non-smoker and had no history of pulmonary diseases.
During the later part of labor, she suddenly developed facial edema, subcutaneous thoracic emphysema and dyspnea.
Arterial blood gas analysis revealed severe hypoxemia and hypocapnia.
Blood pressure and cardiac rate were normal and sensorium was intact (Kelly score=1).
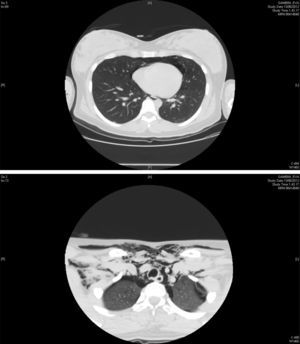
Chest CT scan showed a large pneumomediastinum with bilateral pneumothorax (Fig. 1).
The patient was submitted to cardio-respiratory monitoring and treated with oxygen and conservative therapy.
Within five days of hospitalization, the patient's condition improved with complete resolution of the subcutaneous emphysema and a partial reabsorption of both pneumomediastinum and pneumothorax.
After a follow-up of two weeks, chest X-ray turned out to be normal.
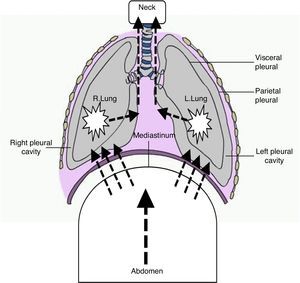
Patho-physiologically, the development of pneumomediastinum during spontaneous delivery is linked to the sudden laceration of the alveola due to the increase of intrathoracic and intra-abdominal pressure caused by repeated Valsalva maneuvers (Fig. 2).
The main physiological alterations of the respiratory system that occurred during the last part of pregnancy are mainly the consequence of the progestin stimulation of the respiratory drive and consist of a reduction in the functional residual capacity and an increase of about 70% in alveolar ventilation due to a breathing pattern with augmented respiratory rate and tidal volume.
During the second stage of labor, hyperventilation and increase of intra-abdominal pressure caused by repeated Valsalva maneuvers are risk factors for the development of pneumothorax and pneumomediastinum, especially in patients with pre-existent subpleural blebs.5,6
In this case report, the pneumomediastinum was likely to be due to this baro-traumatic mechanism.
The current guidelines for the management of pneumothorax and pneumomediastinum do not indicate a specific treatment for Hamman's syndrome. The recommendation of the experts is to encourage better coordination between thoracic surgeons, gynecologists and lung specialists so that this condition can be managed better.1,7,8 Lung specialists should be able to recognize this rare complication of pregnancy in order to coordinate a useful collaboration with other specialists during patient observation and treatment.
Conflicts of interestThe authors have no conflicts of interest to declare.