Non-invasive ventilation (NIV) was clearly one of the most relevant developments of Respiratory medicine in the last decades. Acute exacerbations of COPD are among the strongest indications for NIV.1 For stable COPD, although there are new data pointing to a survival and quality of life benefit,2 there are still some reservations around this indication.
During the national congress of Pulmonology in November 2015, in an interactive session called “NIV in COPD: why, whom and when”, we polled approximately 150 participants. The group consisted of 42% Pulmonology specialists, 14% residents, 8% nurses, 20% clinical physiologists, 1% physiotherapists and 15% doctors from other disciplines. About 40% of the participants had been involved in the previous month in the prescription/titration of more than 4 cases of NIV for chronic respiratory failure (CRF) patients. However 25% had had no practice with NIV for CRF in the previous month.
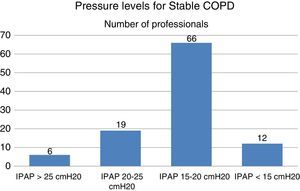
Concerning pressure levels in stable COPD, only 24% of respondents used pressures above 20cmH2O of IPAP, and the majority (64%) prescribed pressures between 15 and 20cmH2O (Fig. 1).
Importance of procedures performed before prescribing domiciliary NIV for COPD were in 29% a combination of nocturnal SpO2, TcCO2 and sleep studies. Around 20% did not perform any of these.
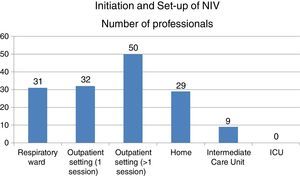
Initiation and set-up of NIV was done in one third of cases in the outpatient setting in more than one daily session, with 20% performed in the respiratory ward and 19% at home (Fig. 2).
Our findings suggest that a wide group of professionals are interested/involved in the prescription of NIV in Portugal. There is some heterogeneity in the experience of prescribing NIV, with a minority of centres (21%) with more than 10 set-ups per month. Only 26% of prescriptions were initiated during elective admission to hospital (respiratory ward or intermediate care unit), supporting the current trend of outpatient NIV initiation.3
Prescriptions for high intensity ventilation are low in Portugal. Nocturnal polygraphy with TcCO2 monitoring should be considered more highly for evaluation and follow-up of these patients.
Reinforcing education in this area together with creation of referral centres specialized in the prescription and control of NIV is highly recommended.
Conflicts of interestThe authors have no conflicts of interest to declare.