The current treatment for advanced non-small cell lung cancer (NSCLC) patients harboring epidermal growth factor receptor (EGFR) mutations is centered around EGFR-tyrosine kinase inhibitors (EGFR-TKIs).1,2 However, resistance to EGFR-TKIs frequently develops. Multiple reports have shown that the T790 M mutation is present in approximately half the patients who develop resistance to a first- or second-generation EGFR-TKIs. Osimertinib is approved for the treatment of NSCLC harboring T790 M, highlighting the clinical relevance of the detection of this mutation.3 Genotyping for EGFR T790 M initially required a tissue biopsy, with its inherent risks and possible treatment delay. More recently, noninvasive genotyping of cell-free plasma DNA emerged as a safer and faster alternative for detection of EGFR T790M.4 There was no previous data on the prevalence of T790 M mutation in the Portuguese patients with advanced NSCLC. Therefore, the objective of this study was to determine the frequency of this mutation in patients with advanced NSCLC.
This prospective, analytical, multicenter study included 40 adult patients with locally advanced or metastatic NSCLC treated at 13 Portuguese oncology centers, from November 2017 to March 2019, and who had progressed or discontinued due to adverse effects following therapy or after two or more lines of treatment with EGFR-TKI and chemotherapy. The presence of T790M-EGFR mutation was assessed both in tissue and blood biopsy. Blood samples were analyzed by Ampliseq™ EGFR Hot Spots NGS panel from Thermo Fisher, cobas® EGFR Mutation Test v2 US-IVD from Roche Molecular Diagnostics and digital PCR EGFR T790 M by Thermo Fisher. All patients signed an informed consent form, and the study was previously evaluated and approved by the Ethics Committee of the participating sites.
Patients median age was 69 years (interquartile range 62–74.25 years) and 65% were females. Prior to sample collection, 32 (80%) subjects had received treatment with EGFR-TKIs, 7 (17.5%) had had chemotherapy and EGFR-TKIs, and one received EGFR-TKIs, chemotherapy and immunotherapy. Thirty-nine patients had conclusive results for liquid biopsy (one subject did not perform tissue biopsy and had an inconclusive result in liquid biopsy) and 12 patients for tissue biopsy.
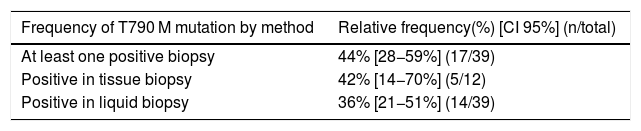
The frequency of T790 M mutation was 44% (95% CI: 28−59%), Table 1.
This study was limited by the low recruitment rate that implied the end of the study with 40 patients instead of the target sample of 155 subjects. Moreover, only 12 samples were obtained for tissue biopsy. For these reasons, it was not possible to draw statistically significant conclusions regarding our secondary objectives, namely the concordance between liquid vs. tissue biopsy, and the comparison between techniques for determining the T790 M mutation of the EGFR gene in liquid biopsy.
Nonetheless, the frequency of T790 M mutation in the target population was comparable to that reported in the literature5 which underlines the relevance of the testing.
In Portugal, the criteria for EGFR genetic screening varies between medical institutions and it is still not a routine assessment in clinical practice. These results, as well our unforeseen low recruitment, highlight the importance of issuing guidelines and implementing them in current practice.
Conflicts of interestThe authors have no conflicts of interest to declare.
FundingThis work was supported by AstraZeneca-Produtos Farmacêuticos, Lda.
We thank all the participating investigators for their contribution in data collection, and patient selection/evaluation during the study: Dr. Gabriela Fernandes, Prof. Dr. António Araújo, Dr. Bárbara Parente, Dr. Ana Barroso, Dr. Ulisses Brito, Dr. José Albino Lopes, Dr. Lourdes Barradas, Dr. Marcos Pantarotto, Dr. Margarida Felizardo, Dr. Ricardo Luz, Dr. António Meleiro, and Dr. Fernando Barata.