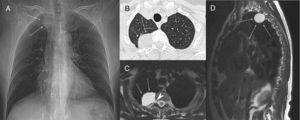
A 68-year-old woman was admitted to hospital with a history of dry cough and mild back pain with chronic evolution. She did not have fever, weight loss, chills or any other symptom, and had a history of smoking one pack per day for 25 years (25 pack-years). Chest radiography demonstrated a posterior mediastinal mass (Fig. 1A), which led her to consult a pulmonologist. Chest computed tomography showed a round hypodense lesion with fluid attenuation, smooth margins, and nocontrast enhancement, originating in the right D2–D3 intervertebral foramen (Fig. 1B). Magnetic resonance imaging (MRI) of the thoracic spine showed a purely cystic non-enhancing lesion originating in the D2–D3 intervertebral foramen, and closely related to the emergent nerve root sheaths (Fig. 1C and D). The cyst was explored surgically and resected through left laminectomy and foraminectomy. Histological examination revealed that it was a perineural cyst. The surgical treatment was curative. After 1 year, the patient remains asymptomatic.
Scout view of a computed tomography (A) showing a right paravertebral mass (arrows) at the D2–D3 level. Axial chest computed tomography (B) demonstrating an oval mass (arrows) originating in the posterior mediastinum, at the level of the right D2–D3 intervertebral foramen. T2-weighted axial (C) and sagittal (D) magnetic resonance images showing a hyperintense round lesion (arrows), with signal intensity similar to fluid, originating in the extradural space at the level of the right D2–D3 intervertebral foramen (arrowhead).
The spinal perineural cyst, also known as the Tarlov cyst (TC), is a rare anomaly of the nervous system and a subtype of meningeal cyst. A TC is defined as a cystic dilatation between the perineurium and endoneurium of the spinal nerve roots, located at the level of the spinal ganglion and filled with cerebrospinal fluid (CSF). Histologically, TCs are characterized by the presence of nerve fibers in the fibrous tissue of their walls.1–4
The origin of these lesions is controversial and unclear. Theories proposed for TC formation include inflammation in the subarachnoid space, traumatic hemorrhage that leads to the blockage of venous drainage of the perineurium and epineurium, congenital diverticula from persistent embryonic fissures, and hydrostatic CSF pressure.1–3 It has been suggested that restricted communication with CSF in the thecal sac may result in a ball-valve mechanism that permits one-way entry of CSF into the cyst during systolic pulsations, with no exit during diastole.2
TCs are found predominantly at the lumbosacral level of the spine; they may occur at all spinal levels, but they are rarely seen in the thoracic spine.1–4 Meningeal cysts are classified according to location relative to the dural and arachnoid space, and to cyst wall pathology. Type I cysts are extradural. Type II cysts are perineural TCs or spinal nerve root diverticula, and their cyst walls can contain nerve fibers. Type III cysts are intradural.3
Most TCs are asymptomatic and clinically insignificant.2–4 Symptoms of perineural cysts depend on their localization and size. Large cysts can compress and damage nerve roots, the spinal cord, and/or surrounding bone.2 They can be present as single or multiple lesions at various levels, and their incidence is higher in females than in males.2,4
Computed tomography myelography and MRI are useful imaging tools for the diagnosis of TC. On computed tomography myelography, the absence of early contrast enhancement is a characteristic finding. MRI typically demonstrates signal intensity characteristics consistent with CSF-containing cysts. However, the final diagnosis is made histopathologically, often during surgery.1,3
No standard treatment for TC has been established. Controversy surrounds the treatment of symptomatic lesions, with a broad range of options from conservative medical management to percutaneous cyst aspiration to open cyst fenestration or excision. When a patient has neurological deficits caused by spinal cord compression by a growing tumor, surgery is mandatory.1–3
The literature contains very few case reports describing thoracic TCs.1,2,5 The main entities considered in differential diagnosis are other cystic nerve root sheath tumors. The presence of a solid component and contrast enhancement of the cyst suggest cystic schwannoma and cystic neurofibroma as important considerations in differential diagnosis.6
Conflicts of interestThe authors declare that they have no conflicts of interest to express.