SARS-CoV-2 is a new beta coronavirus, similar to SARS-CoV-1, that emerged at the end of 2019 in the Hubei province of China. It is responsible for coronavirus disease 2019 (COVID-19), which was declared a pandemic by the World Health Organization on March 11, 2020. The ability to gain quick control of the pandemic has been hampered by a lack of detailed knowledge about SARS-CoV-2-host interactions, mainly in relation to viral biology and host immune response. The rapid clinical course seen in COVID-19 indicates that infection control in asymptomatic patients or patients with mild disease is probably due to the innate immune response, as, considering that SARS-CoV-2 is new to humans, an effective adaptive response would not be expected to occur until approximately 2–3 weeks after contact with the virus. Antiviral innate immunity has humoral components (complement and coagulation-fibrinolysis systems, soluble proteins that recognize glycans on cell surface, interferons, chemokines, and naturally occurring antibodies) and cellular components (natural killer cells and other innate lymphocytes). Failure of this system would pave the way for uncontrolled viral replication in the airways and the mounting of an adaptive immune response, potentially amplified by an inflammatory cascade. Severe COVID-19 appears to be due not only to viral infection but also to a dysregulated immune and inflammatory response. In this paper, the authors review the most recent publications on the immunobiology of SARS-CoV-2, virus interactions with target cells, and host immune responses, and highlight possible associations between deficient innate and acquired immune responses and disease progression and mortality. Immunotherapeutic strategies targeting both the virus and dysfunctional immune responses are also addressed.
Coronaviruses (CoV) are a diverse group of single-stranded RNA viruses that infect various vertebrates. They were first detected in humans in the 1960s1 and mainly cause mild upper respiratory disease. At the turn of the 21st century, however, new infections caused by zoonotic transmission of highly pathogenic strains of beta coronavirus started to emerge. These include the first severe acute respiratory syndrome virus (SARS-CoV-1) in 2002 and the coronavirus-related Middle Eastern respiratory syndrome coronavirus (MERS-CoV) in 2012, both with high respiratory disease mortality (10% and 34%, respectively).2 SARS-CoV-2 is a new beta coronavirus, similar to SARS-CoV-1, which emerged at the end of 2019 in the Hubei province of China.3 It is the cause of coronavirus disease 2019 (COVID-19).2,4
By March 11, 2020, SARS-CoV-2 had infected more than 100,000 people from over 100 countries around the world and caused 4000 deaths. The World Health Organization declared the situation a pandemic, the first ever due to a coronavirus.5 Infections have since grown exponentially across countries and continents, largely due to increased globalization and the ease and speed of international travel. The ability to gain rapid control of the pandemic has been limited by numerous factors, including a lack of detailed knowledge about SARS-CoV-2 biology and host immune responses, a lack of rapid diagnosis and case identification, and a lack of clearly effective treatments. A greater understanding of host-pathogen interactions is urgently needed to help identify reliable and effective diagnostic, control, and treatment strategies and prevent the spread of infection. At the same time, the medical and scientific community has generated knowledge and information at a dizzying rate and participated in unprecedented levels of sharing across the most diverse of scientific publication platforms.6,7
In this paper, the authors review the most recent publications on SARS-CoV-2 immunobiology, virus-receptor interactions, and host immune responses, with a particular focus on recent evidence pointing to a role for impaired innate and acquired immunity and dysfunctional immune responses to disease progression and mortality. The authors also briefly address immunotherapeutic strategies targeting the virus and aberrant immune responses.
MethodologyTo retrieve information for this narrative review, the authors searched PubMed and preprint servers (MedRxiv and BioRxiv) for articles published between January 2020 and January 2021, using the keywords “SARS-CoV-2”, “Immune response”, “Immunopathology”, and “Treatment”. The inclusion criteria were publications of all types addressing SARS-CoV-2 immune responses and COVID-19 immunopathology written in English, Spanish, or Portuguese. The results of this review are based on evidence from randomized clinical trials (RCTs) (n=14), systematic reviews (n=3), original research (n=52), observational studies (n=45), opinion/commentary articles (n=9), and selected reviews (n=47). We also examined cross-references from these publications.
The immune response to SARS-CoV-2Natural history of COVID-19The clinical consequences of SARS-CoV-2 infection have been extremely variable, ranging from a benign course to rapidly progressive disease leading to death within 2–3 weeks of symptom onset. While many infected individuals are asymptomatic8,9 or only experience upper respiratory symptoms, others develop interstitial pneumonia, which can quickly progress to respiratory failure and acute respiratory distress syndrome (ARDS), requiring mechanical ventilation and admission to an intensive care unit (ICU) and possibly culminating in multiorgan failure.10–12 In addition, asymptomatic patients have significantly longer viral shedding periods, which has implications for disease spread.13
Patients with severe COVID-19 can worsen rapidly. Rapid progression to respiratory failure was reported in the first case series published,14 with an average time from onset of symptoms of 1–2 weeks for ARDS requiring assisted ventilation in an ICU, 8 days for dyspnea, 9 days for ARDS, and 10.5–14.5 days for ICU admission/intubation. The main cause of death was respiratory failure (85%), associated with shock in a third of cases.15 Mortality rates, however, vary greatly from country to country for a variety of reasons, both general, such as healthcare infrastructure and testing availability, and specific, such as risk or protective factors and racial heterogeneity reflected in different genetic susceptibility backgrounds, and individual immune response factors.7,16,17
As SARS-CoV-2 is a new pathogen for humans, an effective adaptive immune response capable of neutralizing new antigens can be expected to develop about 2–3 weeks after contact with the virus.18 Considering this rapid chronology, infection control in patients with asymptomatic or mild disease is probably due to the innate immune response, where activation does not depend on recognition by antibodies and/or T cells. Severe forms of the disease, in turn, may be due to failure of nonspecific first-line defense mechanisms and/or the development of an acquired immune response, which, if amplified, could become pathogenic to the host, particularly in the presence of relevant comorbidities.
The innate immune response to SARS-CoV-2Antiviral innate immunity has several humoral components, including components of the complement and coagulation-fibrinolysis systems, soluble proteins that recognize glycans on cell surfaces (e.g. mannose binding lectin [MBL]), interferons (IFN), chemokines, and naturally occurring antibodies (mainly IgM but also IgA and IgG). It also has several cellular components, namely natural killer (NK) cells and other innate lymphoid cells (ILCs) and gamma delta T cells, which generally limit the spread of viral infection by cytotoxic action on target cells, cytokine production, and induction of an adaptive response.
In the next sections, we will look at some of the mechanisms that are gaining recognition as having a possible role in the immunopathogenesis of COVID-19, such as soluble components and the production of interferon after the virus enters mucosal cells in the respiratory system.
SARS-CoV-2 exhibits extensive glycosylation in the S (spike) protein of the viral surface that binds to the host cell receptor: angiotensin-converting enzyme 2 (ACE-2).19 Glycosylation of the viral surface can influence several aspects of virus's biology, such as the stability of protein components, cell tropism, recognition by immune mechanisms, and camouflaging of antigens recognized by neutralizing antibodies. Recent experimental findings suggest that distal mutations (10nm away from the receptor-binding domain – RBD) may impact SARS-CoV-2 RBD-ACE-2 binding affinity. This polybasic cleavage site is a possible target to neutralize SARS-CoV-2 binding to its receptor.20
Natural antibodies. Anti-glycan antibodies are naturally detected in serum, that is, they are detected in the absence of prior immunization, similarly to naturally occurring ABO antibodies. Like ABO antibodies, they mainly belong to the IgM class. Natural IgM concentrations seem to mirror some of the patterns of clinical severity in COVID-1921: they decrease significantly with age (>40 years) and are found in lower concentrations in men and individuals with blood group A. A protective role of high anti-A antibody titers has been described for SARS-CoV-122 and has also been suggested for SARS-CoV-2.23 Conflicting findings, however, have been reported. In a large multi-institutional cohort of patients, Latz et al.24 concluded that blood type was not associated with the risk of progression to severe disease requiring intubation or causing death, but they did find that patients with blood type O had the lowest frequency of SARS-CoV-2 positivity. In another study, Zietz and Tatonettti25 found evidence for protective associations between O blood groups and enrichment of B blood groups among SARS-CoV-2-positive patients. This observation is contradictory, as anti-A antibodies are present in both B and O blood group individuals. Since only a fraction of COVID-19 patients experience severe disease (intubation or death), larger series are needed to understand these correlations.
Complement system. The complement system is a critical component of the innate immune response to viruses, but it can also trigger proinflammatory responses.
MBL, one of components of the complement system in innate immunity, recognizes mannose residues in the membrane of a diversity of microorganisms and acts as a soluble pattern recognition receptor (PRR). This recognition activates the complement system, inducing inflammation and enhancing phagocytosis. It is known that MBL can bind SARS-CoV, leading to C4 deposition in the virus, and, in experimental models, reducing its capacity for infection.26 The presence of mannose-rich glycans in the S1 region of SARS-CoV-2 has raised the hypothesis that glycan recognition and binding to MBL may inhibit S1-ACE interaction.19 Certain MBL genetic polymorphisms associated with lower serum MBL levels have also been linked to SARS-CoV susceptibility.27 Serum MBL levels are also known to decrease with age.28
Interferons and other cytokines. The IFN response constitutes a major first line of defense against viruses. For many respiratory viruses, including SARS-CoV-1, IFN types I and III (the so-called “innate” IFNs), appear to play a role in limiting infection29 by establishing a cellular state of viral resistance and activating adaptive immune responses.30
IFN types I and III are transiently produced in cells following interaction between microbial derivatives and cellular PRRs. This interaction activates two intracellular signaling cascades: transcription and activation of nuclear factor kB (NF-kB) and interferon regulatory factors. This activation stimulates the production of proinflammatory cytokines and type I and III IFNs, respectively. Via the JAK-STAT signaling pathway, IFNs induce expression of IFN-stimulated genes.30 These mechanisms result in two defense pathways: a cellular antiviral resistance pathway and a cell recruitment pathway via the production of several chemokines. Viral escape mechanisms based on the acquisition of genetic resistance characteristics are known to oppose these lines of defenses.31,32
Type I IFNs (IFN-α/β) are at the first line of the innate immune response to viral infection, inducing viral resistance in both infected cells (autocrine effect) and neighboring cells (paracrine effect), where they interfere with viral and cellular replication. Infection by SARS-CoV-1 and MERS-CoV causing acute respiratory disease has been characterized by a dysregulated inflammatory response in which delayed production of type I IFN favors the accumulation of inflammatory monocyte-macrophages.33 Recent data also point to a possible dysregulation of types I and III IFN in the response to SARS-CoV-2.31,34 Blanco-Melo et al.,34 on analyzing transcriptome profiles of various cells types, showed that SARS-CoV-2 infections elicit very low IFN I and IFN III expression and limited response from IFN-stimulated genes, while inducing normal expression of chemokines and proinflammatory cytokine genes. Another study identified an impaired type I IFN response in COVID-19 patients with severe or critical disease, accompanied by a high blood viral load and an excessive NF-kB-driven inflammatory response, associated with increased tumor necrosis factor (TNF)-α and interleukin (IL)-6.35
Bastard et al.36 recently hypothesized that neutralizing autoantibodies against type I IFNs (mainly IFN-α2 and IFN-ω) might underlie 10% of life-threatening COVID-19 pneumonia cases. Type I IFN dynamics during SARS-CoV-2 infection are not yet clear and further studies are needed to establish whether IFN production is already reduced at the onset of infection or whether it is delayed or exhausted after an initial peak.35
Type III IFN lambda (IFN-λ) (IL-28/IL-29), another member of the IFN innate immunity family, shares homologies with type I IFN and IL-10. Type III IFN expression is more restricted than that of the ubiquitous type I IFNs and mainly occurs on mucous (respiratory and gastrointestinal) barriers. The main difference between type I and type III IFNs is in the expression of their receptors: type I receptors are present in practically all cells while type III receptors (the complex IFNLR1/IL10RB) are restricted to epithelial cells, neutrophils, and certain activated immune cells (dendritic cells, macrophages, and B cells). This suggests that type III IFNs have a more specialized role in the mucosal immune response and in the regulation of the adaptive response. Type III IFNs have a particular role in pulmonary immune responses: they are induced earlier and by a lower viral load (compared with type I), and they also limit the initial spread of the virus37 and its transmission from the upper respiratory tract to the lungs.38 They do not have the proinflammatory potential of type I IFNs and may actually have anti-inflammatory and tissue protective effects.29,39
Recent findings from animal models of SARS-CoV-2 infection suggest that types I and III IFNs contribute to limiting local (type III) and systemic (type I) viral dissemination.3 They also, however, suggest that type I IFNs may induce an intense systemic and pulmonary inflammatory response. Blanco-Melo et al.,34 in their recent study of transcriptional responses to SARS-CoV-2 compared with other respiratory viruses (influenza A and SARS-CoV-1), reported findings suggesting a dysregulated host response, since SARS-CoV-2 did not trigger a robust IFN I/III response (at least at lower viral loads) but did induce robust production of chemokines able to recruit inflammatory cells. In these experimental models, which included pulmonary cell lines, animal models, and ex vivo samples (lung tissue from patients with COVID-19), they also demonstrated significant induction of monocyte- and neutrophil-associated chemokines (CCL2 and CCL8 and CXCL2 and CXCL8, respectively). Their findings are consistent with data from patients with COVID-19 that characteristically show peripheral neutrophilia, a prognostic biomarker40,41 and, in the severest cases, a predominance of peripheral-derived lung macrophages.42
Like intrinsic viral suppression of IFN responses, host age also appears to dictate cytokine profiles,30 suggesting that the imbalance that occurs between proinflammatory cytokines and IFN production in aging may have important pathogenic implications in COVID-19. COVID-19 severity and outcomes are strongly linked to age, with adults over 65 years accounting for 80% of all hospitalizations and showing a 23-fold higher risk of death than those under 65. Comorbidities such as cardiovascular disease, diabetes, and obesity also increase the risk of mortality due to COVID-19, but they alone do not explain why age is an independent risk factor.43 Like other organs and tissues, the immune system changes with age, and it does so in two main ways: immunosenescence and inflammaging. Immunosenescence is a gradual decline in immune function that interferes with pathogen recognition, alert signaling, and clearance, causing increased susceptibility to infections and other immune-related chronic disorders, such as autoimmune diseases and cancer.44,45 Inflammaging, in turn, is an increase in systemic inflammation that arises from an overactive yet ineffective alert system whereby a decline in cellular repair mechanisms causes an accumulation of genome and proteome damage, leading to systemic changes in the immune system and increased production of proinflammatory cytokines.46
IL-1 is another important cytokine associated with inflammation and innate immunity. It is mainly produced by activated mononuclear phagocytes and can induce other proinflammatory cytokines such as IL-6 and TNF. Although IL-1 administered in low doses can be protective, high levels produced during infection can be detrimental. IL-1 activated by SARS-CoV-2 stimulates the secretion of IL-6 and TNF, a proinflammatory complex that can trigger a cytokine storm with deleterious pulmonary and systemic effects.47 Moreover, it is now apparent that IL-1 and related cytokines (IL-33, IL-18), in addition to participating in classical generic inflammation, regulate innate immunity and inflammation in response to different microbial or environmental challenges. For instance, the differentiation and polarization of innate lymphoid cells (ILC-3/Th17) is also driven by IL-1.48
Neutrophils. Experimental data suggest that neutrophils may also be involved in the pathogenesis of COVID-19,34 as SARS-CoV-2 infection induces CXCL2 (GROβ) and CXCL8 (IL-8), two neutrophil-recruiting chemokines. This hypothesis is consistent with the characteristic peripheral neutrophilia seen in COVID-19 patients.40,41 Neutrophilia is a predictor of poor outcome and the neutrophil-to-lymphocyte ratio has been identified as an independent risk factor for severe disease and death.49,50 Some authors have suggested that neutrophils might have an important role in the inflammatory response to COVID-19 by promoting organ injury and coagulopathy (immunothrombosis) via direct tissue infiltration and formation of neutrophil extracellular traps (NETs) in a process known as NETosis.51,52
NETs are extracellular webs of DNA, histones, microbicidal proteins, and oxidative enzymes released in response to the activation of neutrophils by PPRs or chemokines.53 A growing body of evidence suggests that NETs may have a double-edged–sword effect. While NETs have microbicidal activity, their sustained formation also stimulates many disease processes and can trigger a cascade of inflammatory reactions that destroy surrounding tissues, facilitate microthrombosis, and result in permanent organ damage in the pulmonary, cardiovascular, and renal systems.54,55 Veras et al.,54 in an autopsy study, reported an increased concentration of NETs in plasma, tracheal aspirate, and lung tissue specimens from COVID-19 patients, and also found that circulating neutrophils were infected with SARS-CoV-2 and released high levels of NETs. The above results suggest that neutrophils participate in the innate immune response to SARS-CoV-2 infection, and NET-related necroinflammation probably has a central role in causing the cytokine storm in COVID-19, as well as sepsis and multiorgan failure.56
Antibody response dynamicsAs SARS-CoV-2 is new to humans, specific antibodies to its S glycoprotein are not detectable in the early phase of infection, that is, before an adaptive immune response is mounted.18 Most serological studies to date have analyzed acute stages of infection and their findings seem to suggest that IgM antibodies appear between day 8 and 12 and disappear by week 12. IgG antibodies, by contrast, seem to appear later (day 14) and last for longer. The intensity of the IgG response seems to be related to both viral load and disease severity.57,58 Long et al.13 found that asymptomatic individuals had significantly lower virus-specific IgG levels than their symptomatic counterparts. In addition, 40% of asymptomatic versus 13% of symptomatic individuals showed negative results for IgG in the early convalescent phase. The degree and duration of protection conferred by this response remain to be determined, but recent findings have raised concerns that humoral immunity against SARS-CoV-2 may not be long lasting in people who have experienced mild disease.59 While some preliminary findings suggest that the passive transfer of antibodies via convalescent plasma has therapeutic efficacy,60 a recent serological study showed that titers are only moderately correlated with viral neutralization activity.61 This study, which analyzed the plasma of 175 patients with moderate symptoms who recovered, confirmed that humoral response to SARS-CoV-2 occurs between day 10 and 15 of infection. Nonetheless, 47% of the patients had low or very low titers of neutralizing antibodies for up to 2 weeks after hospital discharge. As a possible explanation for why these patients recover with such low titers of neutralizing antibodies, the authors suggested the involvement of acquired immune response components other than antibodies (e.g., a T-cell response).
Recent reports from two small series of COVID-19 patients with primary humoral immunodeficiencies62,63 also suggest that antibodies do not have a critical role in the immune response to SARS-CoV-2. Four patients with primary agammaglobulinemia had a favorable outcome, despite developing pneumonia, while five with common variable immunodeficiency developed more severe forms of the disease. Although all the patients were treated with intravenous immunoglobulin therapy, the donor plasma did not contain specific antibodies for SARS-CoV-2 and would only have protected against secondary infections. Lacking the capacity for an effective “de novo” antibody response, these patients maintained an intact nonspecific immunity compartment (e.g., phagocytes, NK cells, and IFN). The authors also speculated as to whether COVID-19 complications might be associated with the presence of dysfunctional B cells (absent in agammaglobulinemia) or an acquired cellular immune response (T cells).
These observations further support the hypothesis that innate immunity is key in the initial response to viral infection,21 which precedes a specific acquired response dependent on B cells and their antibodies and T cells and their cytokines. Failure of the innate immune system would pave the way for uncontrolled viral replication in the airways and the emergence of adaptive immunity, potentially amplified by the inflammatory response.
B cells and plasmablastsIL-6 and TNF-α cooperate at different levels in the regulation of B-cell life and activity and act sequentially in B-cell-mediated immune response.64 Changes in circulating B-cell subpopulations have been shown in patients with COVID-19. A number of studies have shown that severe COVID-19 is characterized by an increase in proliferating, metabolically hyperactive, plasmablasts (PBs) and a relative decrease in memory B cells and found that these changes coincided with severity of inflammation and disappeared with convalescence.64–66 In some cases, PBs accounted for over 30% of circulating B cells, similar to levels observed in acute dengue and Ebola infections.65,67
A direct correlation has been observed between increased plasmablast frequency and oligoclonal expansion of antibody clones within the overall B-cell repertoire, suggesting that many of these large clonal expansions reside within the plasmablast pool.65 Nonetheless, transient increases in PBs and relative decreases in memory B cells were not correlated with specific antibodies levels.66 This lack of correlation between PB expansion and neutralizing antibodies suggests that a proportion of these large PB responses were generated against SARS-CoV-2 antigens other than the S protein.67
Finally, the high metabolic activity observed also suggests that PBs act as a nutrient sink, possibly contributing to metabolic exhaustion of the cells and/or altered glycosylation patterns of antibodies, which have also been linked to severe COVID-19.66
The T cell responseThe T-cell response is a key component of the adaptive immune response to viral infection.68 CD8+ T cells are important because of their specific cytotoxicity for infected cells, while CD4+ T cells are important because they activate CD8+ cells and B cells and also produce cytokines that favor cell recruitment.
One recent study described circulating activated SARS-CoV-2-specific T cells 7 days after the onset of COVID-19 symptoms in a patient with moderate disease who fully recovered.69 Grifoni et al.70 also measured SARS-CoV-2-specific CD4+ and CD8+ T-cell responses in patients with COVID-19 and observed CD4+ T-cell and antibody responses in all patients and CD8+ T cell responses in most. They also detected CD4+ T-cell responses in 40% to 60% of unexposed individuals. Sekine et al.71 showed that SARS-CoV-2 elicits highly functional memory T-cell responses. The strongest responses occurred in individuals who recovered from severe COVID-19, but lower-intensity responses were also observed in patients with mild disease and even in family members exposed to the virus, sometimes in the absence of SARS-CoV-2 specific antibodies. Acute-phase SARS-CoV-2-specific T cells displayed a highly activated cytotoxic phenotype, whereas convalescent-phase cells were polyfunctional and showed a memory phenotype.
It has been proposed that SARS-CoV-2-specific T cells in unexposed individuals might originate from memory T cells derived from exposure to common cold coronaviruses, which circulate widely in humans, causing mild self-limiting respiratory symptoms.72 Whether this immunity is relevant in influencing clinical outcomes is unknown, but it may be of value in herd immunity and vaccine development.
The immunopathology of COVID-19The pathophysiology of pulmonary disease caused by SARS-CoV-2 is very similar to that described for SARS-CoV-1 and MERS-CoV, where lung injury has been linked to an aggressive inflammatory response.73,74 The pathological basis appears to be damage to infected lung cells – type II pneumocytes and capillary endothelial cells – which leads to compromised pulmonary gas exchange (hypoxemia) and a considerable plasma exudate in alveolar spaces. Histopathological studies have confirmed diffuse alveolar damage, with the formation of hyaline membranes, mononuclear and macrophage infiltration of air spaces, and diffuse thickening of alveolar walls.74
Disease severity in COVID-19 appears to be modulated not just by viral infection but also by aberrant immune and inflammatory responses in the host. Recent data suggest that this immune dysregulation might be involved in an immunosuppression phase75,76 that would follow the proinflammatory (cytokine storm) phase and be accompanied by peripheral lymphopenia and a high risk of secondary bacterial infections.15
As mentioned, an imbalance in the innate immune system may be one of the triggering factors for viral proliferation and immune dysregulation, with subsequent components of the acquired immune response contributing to the expansion and perpetuation of this dysregulation. Some of the immunopathological mechanisms proposed for COVID-19 will be further analyzed in the next sections.
Innate immunity and inflammatory pathwaysExcessive cytokine production. Some viruses, including SARS-CoV, are cytopathic, that is, they induce cell damage and death in infected tissues by pyroptosis.68 Increased levels of IL-1β, one of the characteristic proinflammatory cytokines released during pyroptosis, were recently reported in patients with SARS-CoV-2 infection.14 The components released by the lysis of respiratory epithelial cells – ATP, DNA etc. – can then be detected as DAMPs (damage-associated molecular patterns) by the PRRs of other epithelial cells and alveolar macrophages, resulting in their activation. In a physiological situation, this response in the deep lung would favor the elimination of microorganisms due to the clearance activity of alveolar macrophages. However, some patients, whether because of a high viral load77 and/or individual immunogenetic risk factors, may experience a dysfunctional immune response, resulting in systemic and/or diffuse pulmonary hyperinflammation, triggered by overproduction of cytokines (cytokine storm syndrome)76 or macrophage activation syndrome (MAS).78
Age-related changes may increase disease susceptibility and hamper the mounting of an effective immune response against SARS-CoV-2 in the elderly. The interplay between immunosenescence and inflammaging has been hypothesized to contribute to the cytokine storm in elderly patients with COVID-19.79 Excessive activation of the immune system has also been observed in several autoimmune, infectious, and neoplastic disorders. The term “cytokine storm syndrome” could therefore apply to a group of diseases other than COVID-19 and probably also some clinical stages of COVID-19. Inflammation and multiorgan involvement are the hallmark of these diseases.80 The cytokine storm has been associated with ARDS, the main cause of mortality in patients with COVID-19, and a clinical picture similar to MAS may be observed in a subset of patients with severe disease.78 In this context, some authors have suggested that COVID-19 might fall within the spectrum of hyperferritinemic syndromes. However, not all patients with COVID-19 meet the diagnostic criteria for hyperferritinemic syndrome, as they have modestly elevated ferritin levels and the lung is the target organ in severe disease.80 It is not yet clear whether ferritin is a mere acute-phase protein or an active pathogenic mediator in COVID-19.81
Elevated plasma levels for a wide range of cytokines have been observed in critical-care COVID-19 patients.14 Circulating IL-6 levels seem to be related to prognosis in these patients,15,82 together with the expression of cellular markers pointing to the activation of proinflammatory monocytes, either in the lung42 or in circulation.83 Some experimental studies, using cell lines or ex vivo lung tissue,34,84 have confirmed SARS-CoV-2-mediated induction of chemokines such as CCL2 (MCP-1), CCL8 (MCP-2) and CXLC10 (IP10) involved in the recruitment and activation of monocyte-macrophages, suggesting their involvement in the pathogenesis of the cytokine release syndrome/MAS.77,78 Silvin et al.,85 in turn, observed that severe COVID-19 was specifically associated with a burst of circulating calprotectin, which precedes the cytokine release syndrome; low levels of non-classical monocytes in peripheral blood; and emergency myelopoiesis, which stimulates the release of immature and dysplastic myeloid cells with an immunosuppressive phenotype.
Grant et al.86 collected bronchoalveolar lavage fluid samples from 88 patients with SARS-CoV-2-induced respiratory failure. In most patients, the alveolar space was persistently enriched with T cells and monocytes, suggesting that SARS-CoV-2 infects alveolar macrophages, which in turn respond by producing T-cell chemoattractants. These T cells would produce IFN-γ to induce the release of inflammatory cytokines from alveolar macrophages and further promote T-cell activation, forming a positive feedback loop driving persistent alveolar inflammation.
The cytokine release syndrome has both systemic and pulmonary effects within this hyperinflammatory response. Elevated levels of proinflammatory cytokines (IL-1/TNF/IL-6) are associated with multiorgan failure that can result in myocardial injury, hypotension, and shock, a combination that has been named “viral sepsis syndrome”75 and is observed in patients with severe COVID-19. SARS-CoV-2 can reach organs other than the lung, especially if coexpressing ACE-2 and associated proteases.87,88 The relative contribution of the virus and the host's cytokine response to the multiorgan failure seen in some patients, however, is not yet clear.75
There have been a number of recent reports of a pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 and with overlapping features of Kawasaki disease and toxic shock syndrome. Reports from Italy, the United Kingdom, the United States, and France89–92 showed a delay of 30–45 days between signs of COVID-19-like illness (or contact with someone with known or presumed COVID-19) and the onset of the inflammatory syndrome, raising the possibility that it was actually a post-infectious delayed immunologically mediated phenomenon of COVID-19.
Complement activation. When activated, the complement system plays a central role in host defense against infections93 via efficient recruitment of phagocytes and engulfment of pathogens and cellular debris by (C3b- or C5-mediated) opsonization. In the lectin pathway, MBL binds to carbohydrate arrays of mannan and N-acetylglucosamine residues on the surface of viruses or virus-infected cells, resulting in the activation of MBL-associated serine protease-2 (MASP-2).94 Gao et al.95 showed that SARS-CoV-2, MERS-CoV, and SARS-CoV-1 share a common mechanism connecting the viral N proteins to binding and potentiation of MBL-dependent auto-activation of MASP-2, leading to uncontrolled activation of the complement cascade. Persistent complement activation, in turn, leads to uncontrolled inflammation and acute lung disease.96 Evidence of C3a deposition in lung biopsy samples and increased serum C5a levels have been observed in patients with severe COVID-19 who died.95 Complement activation must be controlled as it causes disseminated intravascular coagulation, inflammation, cell death, multiorgan failure, and death.
Smell impairment has been described in patients with systemic diseases characterized by hyperactivation of the complement system, such as systemic lupus erythematosus and hereditary angioedema.97 It has thus been speculated that complement dysregulation, in addition to damage to the olfactory pathways via expression of ACE-2 receptors, might have a pathogenic role in dysosmia in COVID-19.98
In conclusion, activation of the complement system may have a role in both early and late stages of COVID-19. In the early stage, it might be involved in the initial immune response, critical for pathogen clearance, while in the second stage, it might be involved in inflammatory damage.98 Immunomodulatory drugs targeting the complement cascade may be effective for controlling inflammation in Cov-related diseases.99
Intravascular coagulation and endothelial injury. Histopathological examination of postmortem lung tissue from patients with COVID-19 has shown signs of pulmonary congestion, thrombosis, and microvascular occlusion.100 Altered coagulation parameters and elevated d-dimers are also biomarkers in COVID-19101 and are associated with a worse prognosis.102,103 As SARS-CoV-2 does not appear to have intrinsic procoagulant effects,104 coagulation test abnormalities seen in infected patients are most likely to be a result of the profound inflammatory response described above. Activation of host defense systems activates the coagulation cascade105 – “thromboinflammation” – through several procoagulant pathways: contact, activation of coagulation factors by complement products, pathogen-associated molecular mechanisms, formation of NETs (as described above), and endothelial injury mediated by cytokine inflammation.106 Mononuclear cells express tissue factor (CD142) in response to proinflammatory cytokines (mainly IL-6), and CD142 is known to promote the transformation of prothrombin into thrombin. In the absence of vascular injury, initiation of the coagulation cascade is completely dependent on the recruitment of tissue factor–expressing inflammatory monocytes by activated endothelial cells.107
As COVID-19 is associated with hypercoagulability and increased thrombotic risk in critically ill patients, Chow et al.108 evaluated the use of aspirin in 412 hospitalized patients and found that it was associated with a decreased risk of mechanical ventilation, ICU admission, and in-hospital mortality compared with no aspirin.
Recent studies have detected endotheliopathy in COVID-19 and pointed to a probable association with critical illness and death.109,110 Tan et al.111 reported an association between statin use and better outcomes in COVID-19 patients and suggested several possible mechanisms, including 1) statin inhibition of HMG-CoA reductase, which would help reduce viral entry and transmission in COVID-19 by reducing the availability of cholesterol inside cells and tissues; 2) statin-induced blockade of molecular mechanisms, such as NF-kB and TLR signaling, which are responsible for the cytokine storm in severe disease; and 3) statin-based endothelial protection.
Renin–angiotensin system and ACE-2. SARS-CoV-2, like SARS-CoV-1, uses the ACE-2 receptor to enter cells. This receptor is expressed in the epithelium, macrophages, and vascular endothelium of the lung. ACE-2 lung tissue expression is also upregulated by comorbidities frequently observed in patients with COVID-19, such as hypertension, diabetes, and chronic obstructive lung disease.112 SARS-CoV infection induces reduced ACE-2 expression in the lung.68 As ACE-2 participates in the regulation of the renin–angiotensin system, a reduction in levels following infection could disrupt this system, influencing blood pressure and hydroelectrolytic balance and enhancing pulmonary vascular permeability and inflammation.113
Adaptive immunity and amplification pathwaysAntibody production and immune complexes. The exact mechanisms behind the progression of ARDS and the systemic production of IL-6 in COVID-19 remain unclear. One observation that has puzzled clinicians and researchers21 is the coincidence between symptoms of respiratory failure and ARDS and the first signs of an adaptive immune response. Interestingly, specific IgA, IgM, and IgG levels seem to be higher (and occur earlier) in patients with worse clinical outcomes.18,114 Although these observations may be explained by high viral load and replication, they also suggest that an adaptive immune response may contribute to the pathogenesis and severity of pneumonia.
The putative mechanisms involved are diverse and may relate to the formation of pathogenic immune complexes (ICs).115 COVID-19 patients quickly develop specific IgA antibodies which, by forming local ICs, can cause inflammation and microthrombosis.115,116 IgM and IgG ICs can also lead to inflammation and intravascular coagulation through complement activation.117 The binding of virus-antibody ICs to the Fc receptors of alveolar macrophages may cause them to produce CXCL8 (IL-8) and CCL2 (MCP-1), contributing to local inflammation.118 Additionally, non-neutralizing IgG antibodies for SARS-CoV-2 might favor infection by facilitating the fusion of viral particles to the cell membrane in an “antibody-dependent enhancement” mechanism.119,120 Another intriguing observation, also observed with other viruses, is that certain sequences of SARS-CoV-2 may show similarity to host constituents, potentially favoring immunological cross-reactivity and, consequently, an autoimmune response.121 All these observations also seem relevant and informative for the development and safety of future vaccines.
T-cell response. The first autopsy study of a COVID-19 patient with ARDS described strikingly reduced levels of circulating CD4+ and CD8+ T cells associated with hyperactivation phenotypes (Th17 and cytotoxicity).74 Recent studies have also described a strong CCR6+CD4+ T-cell signature in severe COVID-19, indicating a potential role for Th17 cell-mediated immunopathology, including the release of key cytokines such as IL-17 and GM-CSF.74,122 Parackova et al.123 showed that neutrophils skew the polarization of T cells toward Th17 promotion and Th1 suppression in COVID-19 patients, contributing to the dysregulation of the immune response against SARS-CoV-2. An increased Th17 signature may also be associated with elevated IL-6, an important cytokine in the development of Th17 cells.124 IL-17 produced by Th17 cells mediates the activation of monocytes/macrophages, dendritic cells, and neutrophils, and enhances the production of cytokines (IL-1, IL-6, IL-8, IL-21, TNF-α, and MCP-1) by these cells, thus contributing to the cytokine storm.124
Other large COVID-19 series have reported that most patients with severe disease show a significant and sustained reduction in the number of circulating T cells (especially CD8+) and an increased number of neutrophils, with the neutrophil/CD8+ ratio serving as a marker of severity.40,41 Persistent peripheral lymphopenia is also related to a greater risk of secondary bacterial infections15 within an immunosuppression stage following the hyperinflammation phase.75,76 The causes of this lymphopenia are not yet fully understood. A cytopathic effect of the virus does not seem likely, since T cells do not express ACE-2. Possible explanations include intense recruitment of lymphocytes to infected organs,68 apoptotic mechanisms via Fas/Fas Ligand or related to TNF,75,125 and use of corticosteroids to mitigate inflammation.107 It is worth noting that some recent findings point to the possible involvement of CD147 as an alternative gateway to SARS-CoV-2, favoring the direct invasion of T cells and consequent lymphopenia.126,127
Immunotherapeutic approaches to COVID-19No treatments have yet proven effective for COVID-19. Multiple options driven by a better knowledge of the immune response to SARS-CoV-2 have been proposed or are being tested, but they should be considered experimental and require ethical approval and inclusion in a clinical trial.128
Immunotherapeutic strategies to date have focused on two main targets: the virus itself, where the goal is to prevent its interaction with cell receptors and/or intracellular replication, and the consequences of infection, where the goal is to control an overexuberant immune response.
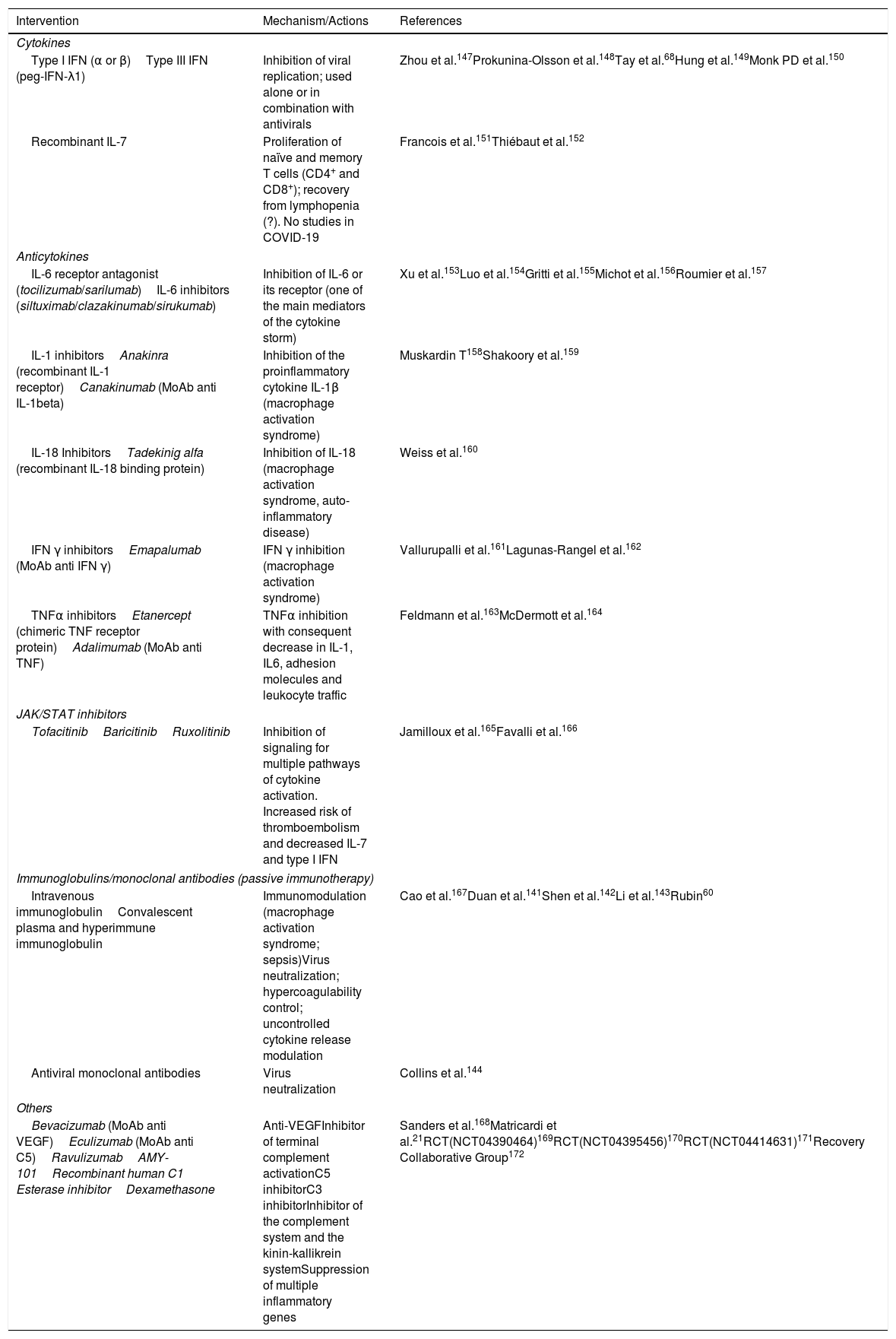
The main interventions based on the proposed immunopathology of COVID-19 are summarized in Table 1.
Immunotherapeutic interventions for COVID-19.
| Intervention | Mechanism/Actions | References |
|---|---|---|
| Cytokines | ||
| Type I IFN (α or β)Type III IFN (peg-IFN-λ1) | Inhibition of viral replication; used alone or in combination with antivirals | Zhou et al.147Prokunina-Olsson et al.148Tay et al.68Hung et al.149Monk PD et al.150 |
| Recombinant IL-7 | Proliferation of naïve and memory T cells (CD4+ and CD8+); recovery from lymphopenia (?). No studies in COVID-19 | Francois et al.151Thiébaut et al.152 |
| Anticytokines | ||
| IL-6 receptor antagonist (tocilizumab/sarilumab)IL-6 inhibitors (siltuximab/clazakinumab/sirukumab) | Inhibition of IL-6 or its receptor (one of the main mediators of the cytokine storm) | Xu et al.153Luo et al.154Gritti et al.155Michot et al.156Roumier et al.157 |
| IL-1 inhibitorsAnakinra (recombinant IL-1 receptor)Canakinumab (MoAb anti IL-1beta) | Inhibition of the proinflammatory cytokine IL-1β (macrophage activation syndrome) | Muskardin T158Shakoory et al.159 |
| IL-18 InhibitorsTadekinig alfa (recombinant IL-18 binding protein) | Inhibition of IL-18 (macrophage activation syndrome, auto-inflammatory disease) | Weiss et al.160 |
| IFN γ inhibitorsEmapalumab (MoAb anti IFN γ) | IFN γ inhibition (macrophage activation syndrome) | Vallurupalli et al.161Lagunas-Rangel et al.162 |
| TNFα inhibitorsEtanercept (chimeric TNF receptor protein)Adalimumab (MoAb anti TNF) | TNFα inhibition with consequent decrease in IL-1, IL6, adhesion molecules and leukocyte traffic | Feldmann et al.163McDermott et al.164 |
| JAK/STAT inhibitors | ||
| TofacitinibBaricitinibRuxolitinib | Inhibition of signaling for multiple pathways of cytokine activation. Increased risk of thromboembolism and decreased IL-7 and type I IFN | Jamilloux et al.165Favalli et al.166 |
| Immunoglobulins/monoclonal antibodies (passive immunotherapy) | ||
| Intravenous immunoglobulinConvalescent plasma and hyperimmune immunoglobulin | Immunomodulation (macrophage activation syndrome; sepsis)Virus neutralization; hypercoagulability control; uncontrolled cytokine release modulation | Cao et al.167Duan et al.141Shen et al.142Li et al.143Rubin60 |
| Antiviral monoclonal antibodies | Virus neutralization | Collins et al.144 |
| Others | ||
| Bevacizumab (MoAb anti VEGF)Eculizumab (MoAb anti C5)RavulizumabAMY-101Recombinant human C1 Esterase inhibitorDexamethasone | Anti-VEGFInhibitor of terminal complement activationC5 inhibitorC3 inhibitorInhibitor of the complement system and the kinin-kallikrein systemSuppression of multiple inflammatory genes | Sanders et al.168Matricardi et al.21RCT(NCT04390464)169RCT(NCT04395456)170RCT(NCT04414631)171Recovery Collaborative Group172 |
C5 – complement factor 5; IFN – interferon; IL – interleukin; MoAb – monoclonal antibody; RCT – randomized clinical trial; VEGF – vascular endothelial growth factor.
Type III IFN, which has tissue protective and inflammatory damage–limiting properties, is being investigated in four clinical trials.129–132 The balance between the benefits and risks of this treatment, however, remain to be determined, as does the best window for effective administration. Early administration of IFN-λ has been found to confer protection in an animal model of COVID-19.133 Recent data from Broggi et al.134 suggest that type III IFN increases the risk of life-threatening bacterial superinfections in chronically inflamed lungs. Understanding the location and timing of IFN production is probably key to the use of this cytokine as a treatment for COVID-19.
Finding an appropriate window of opportunity for administration may also apply to anti-cytokines, such as IL-6 receptor antagonists (e.g. tocilizumab), for which apparently contrasting data have been reported. Early nonrandomized studies suggested benefits and in some cases showed dramatic reductions in mortality.135,136 More recent RCTs, however, did not find that early administration improved disease progression in moderately ill patients with COVID-19 pneumonia137 or prevent intubation or death.138 As with other conceptual treatments proposed for COVID-19, these contrasting results will probably be further clarified with the publication of results from ongoing trials of tocilizumab.139
Convalescent/hyperimmune plasma treatments have also generated controversial results140, but findings have led to the suggestion that they have a role in viral neutralization (passive immunization with donor neutralizing antibodies), hypercoagulability control, and modulation of cytokine release.60,141–143 Much has been published about the use of neutralizing monoclonal antibodies, either alone or in combination. A recent National Institutes of Health document144 concluded that the main lessons to be learned from the use of neutralizing antibody therapies in other conditions (e.g. Ebola) is that antibody potency is key to efficacy and that cocktails may help prevent resistance. That said, logistic and regulatory challenges remain.
In the context of a new infectious disease in a pandemic setting, concepts regarding best treatment practices for COVID-19 are evolving rapidly, and results from ongoing RCTs may well require changes to approaches currently viewed as valid. It is also possible that both positive outcomes and new adverse events may become apparent in long-term observational follow-up studies and RCTs. Appropriate action in this situation is to closely follow the results of ongoing studies and reconsider the use of any treatment if an RCT produces (or fails to produce) convincing results. To this end, we recommend periodic monitoring of updated expert treatment guidelines145 and literature databases,146 which are excellent sources for key updates on COVID-19 treatment strategies.
ConclusionsIn this review, we have analyzed several of the multiple pathways involved in the immune response to SARS-CoV-2 and examined recently acquired knowledge generated in an unprecedented global effort by researchers and clinicians to build a shared and much-needed understanding of COVID-19 pathogenesis. Much of the data from these first 12 months indicate that actions aimed at controlling the inflammatory response and immune dysregulation will be as important as those targeting the virus and its replication mechanisms.
This narrative review has some limitations: information on COVID-19 immunopathology is still limited and our understanding of the disease is evolving rapidly. Thus, the current evidence may soon change with the accumulation of new knowledge of SARS-CoV-2 biology and host immune responses. Several of the questions addressed are based on evidence from very recent medical and scientific literature, conclusions from which need to be replicated by different groups and settings before their findings can be consolidated.
Finally, many of the hypotheses reviewed here are based on a broad discussion among researchers, academics, and clinicians who have been following and coming to terms with this new reality of COVID-19. They are therefore incomplete and may even prove wrong in the near future. Despite these limitations, we hope that this review is aligned with the fourth and final strategic area defined by the World Health Organization (WHO Director-General, 2020) to control this pandemic, which is to innovate and learn.
FundingThis research received no external funding.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors would like to thank all colleagues who contributed with the exchange of experiences, ideas, information, and discussion to the organization of this review, namely Ana Margarida Pereira, André Moreira, Andrea Leonardi, Bernardo Sousa Pinto, Cristina Lopes, Diana Silva, Eduardo Costa, Fábio Kuschnir, Gustavo Wandalsen, Jean-Luc Fauquert, João Fonseca, Jorge Palmares, José Artur Paiva, José Luiz Rios, Luís Araújo, Osvaldo Correia, Paolo Matricardi, Solange Valle, and Tiago Rama.