Obesity seems to play an important role in the pathogenesis of obstructive sleep apnea (OSA).1,2 The prevalence of OSA is estimated to be around 5–25% in the adult population,2–4 reaching up to 45% in obese subjects.2 However, it is the location of body fat accumulation rather than the total amount which seems to be most relevant in assessing the risk of OSA.3,5 Neck and visceral fat accumulation has been described as risk factors for OSA in obese patients.3 Several mechanisms have been proposed for the greater impact of fat accumulated in the abdomen and neck regions in OSA compared with the peripheral ones: reduced pharyngeal lumen size due to fat deposition in the airway walls and increased abdominal pressure in the thorax reducing end-expiratory lung volumes, consequently reducing tracheal traction and increasing collapsibility of the upper airway.1 Nevertheless the impact of regional fat accumulation on the onset and progression of the disease is unclear and studies investigating this complex association would be helpful for a better management of these patients.
The authors, therefore, designed a prospective cross-sectional study which aimed to analyze and compare the impact of cervical and abdominal fat accumulation on the presence and severity of OSA, in a Portuguese group of individuals with suspected diagnosis.
Overnight polygraphy and CT scan of the neck and abdomen, for the measurement of neck fat area (NFA), subcutaneous abdominal fat area (SFA) and visceral fat area (VFA), were performed on a cohort of subjects attending our sleep laboratory with symptoms of sleep disordered breathing, between October 2013 and May 2014. Body mass index (BMI), neck circumference (NC) and waist circumference (WC) were recorded.
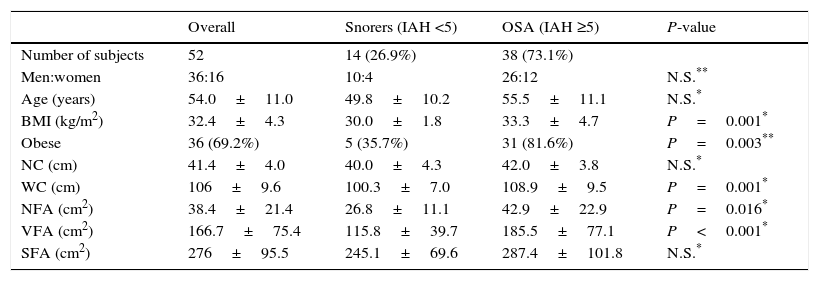
Fifty-two patients were enrolled in the study: the mean±SD BMI was 32.4±4.3kg/m2, 69.2% of the subjects were obese (BMI ≥30kg/m2). The subjects with OSA (n=38, apnea/hypopnea index (AHI) ≥5h–1) had a greater BMI, WC, NFA and VFA than those without OSA (n=14, AHI <5h–1) (Table 1). There was a positive correlation of AHI with BMI (r=0.490, P<0.001), VFA (r=0.417, P=0.002), WC (r=0.417, P=0.002), NFA (r=0.377, P=0.007), SFA (r=0.308, P=0.026) and NC (r=0.282, P=0.04). The BMI, VFA, NFA and WC increased significantly from snorers to severe OSA (Table 2). The multivariate stepwise linear regression analysis was used to analyze the independent factors contributing to AHI: only BMI and VFA were independent risk factors for AHI (model R2=0.303).
Patient characteristics and comparisons of the demographics, clinical parameters and the CT scan measurements between the subjects with and without OSA.
| Overall | Snorers (IAH <5) | OSA (IAH ≥5) | P-value | |
|---|---|---|---|---|
| Number of subjects | 52 | 14 (26.9%) | 38 (73.1%) | |
| Men:women | 36:16 | 10:4 | 26:12 | N.S.** |
| Age (years) | 54.0±11.0 | 49.8±10.2 | 55.5±11.1 | N.S.* |
| BMI (kg/m2) | 32.4±4.3 | 30.0±1.8 | 33.3±4.7 | P=0.001* |
| Obese | 36 (69.2%) | 5 (35.7%) | 31 (81.6%) | P=0.003** |
| NC (cm) | 41.4±4.0 | 40.0±4.3 | 42.0±3.8 | N.S.* |
| WC (cm) | 106±9.6 | 100.3±7.0 | 108.9±9.5 | P=0.001* |
| NFA (cm2) | 38.4±21.4 | 26.8±11.1 | 42.9±22.9 | P=0.016* |
| VFA (cm2) | 166.7±75.4 | 115.8±39.7 | 185.5±77.1 | P<0.001* |
| SFA (cm2) | 276±95.5 | 245.1±69.6 | 287.4±101.8 | N.S.* |
AHI: apnea/hypopnea index; BMI: body mass index; NC: neck circumference; NFA: neck fat area; SFA: subcutaneous fast area; TFA: total fat area; VFA: visceral fat area; WC: waist circumference; OSA: obstructive sleep apnea.
Comparison of BMI, neck and waist circumferences and cervical and abdominal fat areas among snorers and OSA subjects of different severity.
| Snorers | Mild OSA | Moderate OSA | Severe OSA | P-value | |
|---|---|---|---|---|---|
| Number of subjects | 14 (26.9%) | 12 (23.1%) | 14 (26.9%) | 12 (23.1%) | – |
| BMI (kg/m2) | 30.0±1.8 | 32.9±5.4 | 31.8±2.4 | 35.3±5.4 | P=0.014 |
| NC (cm) | 40.0±4.2 | 41.1±5.3 | 42.1±2.1 | 42.6±3.7 | N.S. |
| WC (cm) | 100.3±7.0 | 107.2±14.7 | 108.3±6.3 | 111.3±5.7 | P=0.022 |
| NFA (cm2) | 26.8±11.1 | 36.2±17.6 | 42.6±25.5 | 49.9±23.9 | P=0.042 |
| VFA (cm2) | 115.8±39.7 | 170.3±65.6 | 189.6±95.4 | 195.9±67.4 | P=0.019 |
| SFA (cm2) | 245.1±69.6 | 264.7±107.0 | 269.7±93.4 | 330.6±100.6 | N.S. |
AHI: apnea/hypopnea index; BMI: body mass index; NC: neck circumference; NFA: neck fat area; SFA: subcutaneous fast area; VFA: visceral fat area; WC: waist circumference; OSA: obstructive sleep apnea.
Although more marked in OSA group (81.6%), 35,7% of isolated snorers were obese, probably due to the association of obesity with snoring and daytime sleepiness6 leading to the suspicion of OSA. Among fat measures, VFA and NFA were significantly higher in OSA subjects. Both increased significantly from snorers to severe OSA and were positively correlated with the AHI, although correlation between AHI and NFA was somewhat less strong than with VFA. In multivariate analysis, only BMI and VFA were significantly associated with AHI, suggesting that VFA had a greater impact on the increasing severity of OSA in our sample. The association of OSA with several body habitus measures has been studied and results vary widely among trials. At present, there is no consensus that any one particular habitus phenotype is more important in the pathophysiology of OSA. It is possible that different types of fat distribution are more important in specific subgroups defined by factors such as sex4,7 or ethnicity.7,8 Furthermore the impact of body habitus as a predictor of OSA may vary with age.9
In this study, we found a significant positive correlation between AHI and the anthropometric measures WC and BMI, but not NC. The reason why NC did not show differences between groups and was not correlated with AHI while NFA did, could probably be due to the greater impact of cervical fat depot compared to NC on the presence and severity of OSA in our sample. Thus, a greater amount of NFA to the same perimeter could lead to a reduction of the size of the cervical airway structures and facilitate upper airway collapse.
The main limitation of our study was the small cohort size; however, this could be offset by the prospective nature of the study which allowed the measurement of anthropometric values by the same professional and control of the timing of when sleep and imaging studies took place.
This study characterizes the distribution of body fat accumulation in our OSA patients, analyzes its association with disease severity, and assesses the location of fat distribution with the greatest impact on the disease. These findings suggest a complex association of interactive effects between visceral fat and OSA, with pathophysiologic and therapeutic implications. Continuous positive airway pressure has proven beneficial in these patients3 and they could also benefit from personalized nutrition interventions, exercise programs, or even surgical interventions, with the aim of reducing intra-abdominal visceral fat.
FundingNo funding was received for this research.
Conflict of interestAll authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest, or non-financial interest in the subject matter discussed in this manuscript.
Ethical approvalAll procedures performed in the study were in accordance with the ethical standards of the institutional ethics committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consentInformed consent was obtained from all individual participants included in the study.