Is same-day discharge mode safe and feasible for thoracoscopic lobectomy? This study assesses the safety and feasibility of same-day discharge for patients undergoing thoracoscopic lobectomy.
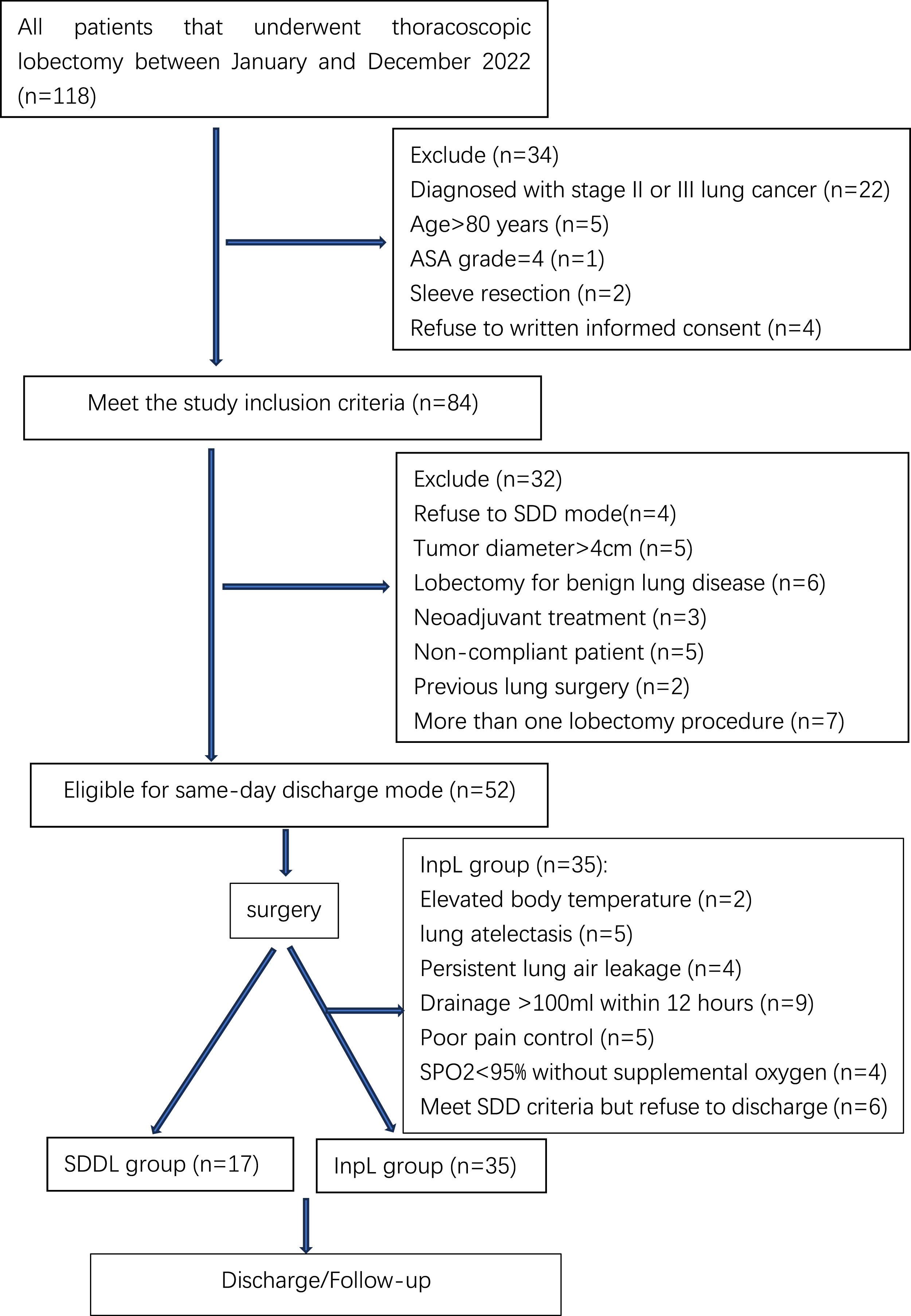
MethodsWe conducted a prospective cohort study from January to December 2022, all patients undergoing thoracoscopic lobectomy were screened for eligibility, and participating eligible patients were separated into a same-day discharge lobectomy (SDDL) group and an inpatient lobectomy (InpL) group based upon length of stay. All discharged patients underwent 30-day postoperative follow-up performed by a team of medical professionals. In addition, eligible patients that underwent thoracoscopic lobectomy from January to December 2021 were included in the historical lobectomy (HisL) group.
ResultsOf the 52 patients that met the eligibility criteria for same-day discharge, 17 were discharged within 24 h after surgery. In the SDDL group, of whom 1 (5.9%) underwent emergency treatment and readmission within 30 days after surgery due to a pulmonary infection, no patients experienced complications such as reoperation, air leakage, atelectasis, chylothorax, or blood transfusion events during the follow-up period. No differences in overall postoperative complication rates were detected between the SDDL and InpL groups (P>0.05), there was a non-significantly higher rate of readmission and emergency visits in the SDDL group relative to the other two groups (P>0.05).
ConclusionsThese results emphasize the safety and feasibility of same-day discharge for patients undergoing thoracoscopic lobectomy, it may further revolutionize the general approach to the hospitalization of thoracoscopic lobectomy patients.
Lung cancer is among the most common malignancies and remains the leading cause of cancer-associated mortality in the world, causing approximately 1.8 million deaths per year.1 Surgical tumor resection remains the primary approach to treating lung cancer, and patients with early-stage disease generally face a low risk of metastasis such that early surgical intervention can greatly improve patient survival outcomes.2 A randomized controlled clinical trial published by the Lung Cancer Study Group in North America in 1995 established anatomical lobectomy as the standard surgical approach to treating early-stage lung cancer.3 While several reports have found that segmental resection can achieve efficacy comparable to lobectomy in these patients,4,5 thoracoscopic lobectomy remains the primary approach to early-stage lung cancer patient management.
Rapid advances in enhanced recovery after surgery (ERAS) models have spurred growing interest in efforts to reduce the duration of postoperative hospitalization for surgery patients,6 leading to the emergence of the same-day discharge approach for certain procedures. Curfman et al. found that same-day discharge could be safely used as a feasible strategy in colon cancer patients,7 while Lee et al. confirmed that same-day discharge could be safely performed for hysterectomy patients, with 729 patients (8.1%) having successfully been discharged on the day of the procedure without any differences in rates of postoperative complications such as re-operation or rehospitalization.8 However, few studies to date have explored the application of a same-day discharge model in patients undergoing thoracoscopic lobectomy,9-11 emphasizing a need for research aimed at clarifying the safety and feasibility of this approach. As such, the present study was developed to address this gap in knowledge by evaluating thoracoscopic lobectomy patients in order to gauge the safety and feasibility of same-day discharge.
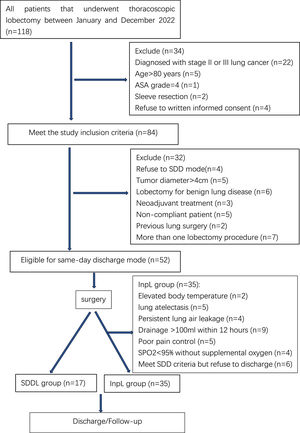
MethodsStudy designThis is a prospective cohort study. The current study follows Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for reporting observational studies, this study was performed in accordance with the Helsinki Declaration and has received approval from the Ethics Committee of Wenzhou Central Hospital (IRB number: L2021-02-052).All patients that underwent thoracoscopic lobectomy between January and December 2022 were screened for potential eligibility for same-day discharge and provided written informed consent prior to study participation.
Inclusion and exclusion criteriaEligible patients for study inclusion were (i) 18-80 years of age, (ii) diagnosed with stage I lung cancer as per UICC 8th edition criteria, (iii) scheduled to undergo thoracoscopic lobectomy, (iv) with good cardiopulmonary function, (v) individuals with an American anesthesia score (ASA) < 4, (vi) individuals willing to provide written informed consent, and (vii) individuals willing to remain within 30 minutes of the hospital for the 48 hours immediately following discharge. Patients were excluded if they (i) exhibited a preoperative tumor diameter > 4 cm, (ii) were undergoing lobectomy to treat a benign lung disease, (iii) had undergone preoperative neoadjuvant treatment or prior lobectomy/partial lobectomy, (iv) were undergoing more than one lobectomy procedure, (v) exhibited poor patient compliance or a lack of family member compliance, or (vi) refused to provide written informed consent.
Data collectionData collected for study participants included age, sex, smoking status, lung function (FEV1/FVC%), ASA classification, clinical stage, tumor location, pathological type, operative duration, length of stay (LOS), estimated intraoperative blood loss, number of lymph nodes dissected, total hospitalization expenses, number of emergency visits and readmission within 30 days after operation, and postoperative complications (reoperation, atelectasis, lung infection, lung leakage, chylothorax, and blood transfusion),chief symptoms (cough, chest pain, hoarseness, and short of breath).
Preoperative preparationFor preoperative preparation, all patients meeting study eligibility criteria underwent preoperative examinations at the preoperative preparation center and signed the provided informed consent form. Analyses performed for these patients included chest computed tomography (CT) scans, brain magnetic resonance imaging (MRI), cardiac ultrasound, lung function, electrocardiogram, abdominal CT, blood gas analysis, coagulation function, liver and kidney function, routine blood, and carcinoembryonic antigen testing. After precluding any potential surgical contraindications, eligible patients underwent a consultation with the medical team regarding the potential for a 24 h discharge and perioperative recovery plan prior to admission, and purchased a simple digital pulse oximeter (50RMB). To enable postoperative follow-up, participating patients were required to join a WeChat group including members of the follow-up medical team, which included one thoracic surgery specialist nurse, one thoracic surgery resident, and one thoracic surgery attending physician with > 8 years of professional experience. This group was responsible for recording patient follow-up information within 30 days postoperatively and resolving any clinical issues raised by these patients.
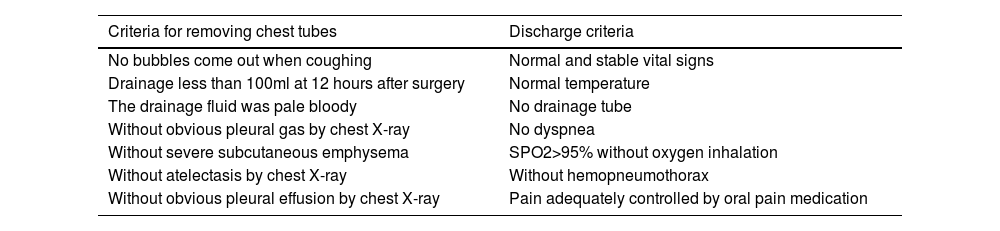
Postoperative management and study groupWithin 6-8 h after surgery, all patients underwent routine blood testing and blood gas analyses. At 12 h postoperatively, a bedside chest X-ray was performed to assess the pulmonary condition of each patient and to determine whether the drainage and leakage met the criteria for chest tube removal and discharge (Table 1). Patients who were discharged within 24 hours postoperatively were classified into the same-day discharge lobectomy (SDDL) group. While the other patients, including those who met the criteria for discharge within 24 hours, but chose to remain in the hospital, were classified in the inpatient lobectomy (InpL) group. To ensure that clinical data would be comparable for this study and with regulatory approval from the hospital ethics committee, those patients that underwent thoracoscopic lobectomy at our center between January and December 2021 meeting the above inclusion criteria for same-day discharge were included in these analyses as the historical lobectomy (His) group.
Criteria for removing chest tube and discharge.
A team of medical professionals conducted a 30-day postoperative follow-up for all discharged patients. The primary outcomes of this study included postoperative complication incidence, 30-day readmission rate, emergency visits. Secondary outcomes included postoperative LOS and total hospitalization expenses. Patients in both groups were followed up by telephone for one month after operation.
Statistical analysisThe sample size for our study was determined based on several factors, including the research question, statistical power considerations, and feasibility. Firstly, we conducted a power analysis to determine the appropriate sample size needed to detect a clinically significant difference between the groups. Secondly, we examined the availability of eligible participants within a reasonable timeframe. Based on these considerations, we arrived at the sample size of 52 we believe is adequate for this research. Data were analyzed with SPSS v 23.0 (SPSS Inc., IL, USA). Categorical variables were reported as percentages and compared using chi-square tests of Fisher's exact test. Normally distributed continuous variables are reported as means ± standard deviations and compared with independent sample t-tests or one-way ANOVAs. All other continuous variables are reported as medians (IQR) and compared with Mann-Whitney U tests or Kruskal Wallis H tests. P < 0.05 served as the cut-off for statistical significance.
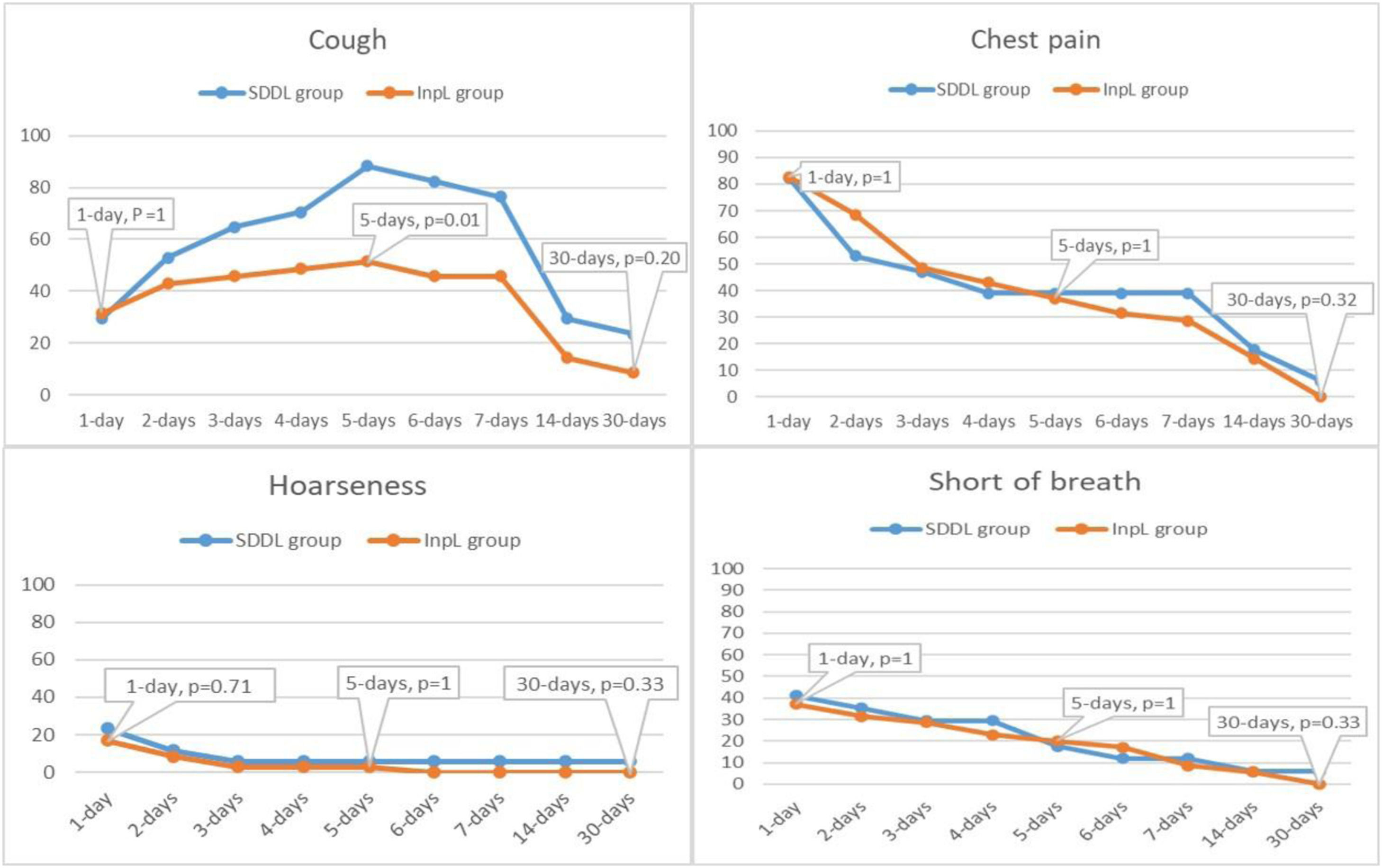
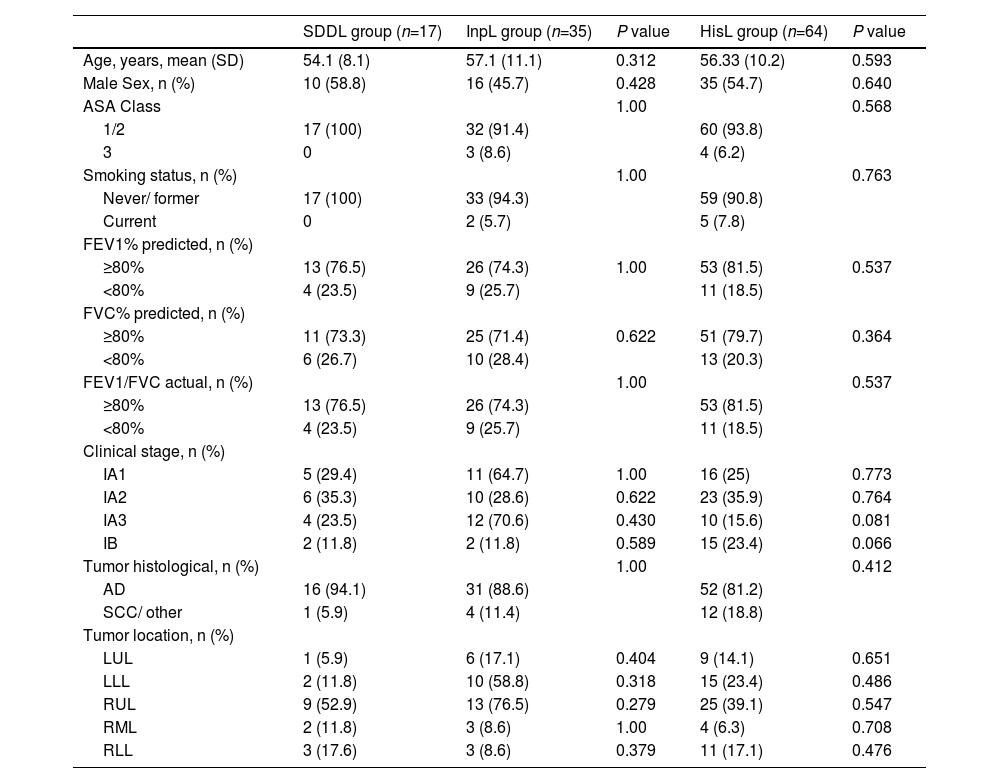
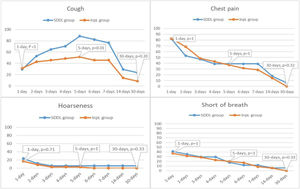
ResultsDuring the period of January to December 2022, a total of 118 patients underwent thoracoscopic lobectomy, as outlined in the study enrollment details (see Fig. 1). In addition, 64 patients in the HisL group met the criteria for same-day discharge, all of whom underwent thoracoscopic lobectomy. The patient characteristics in SDDL group and InpL group are shown in Table 2. There were no instances of intraoperative conversion to thoracotomy or blood transfusion. All patients included within the SDDL group were discharged 15–24 h after surgery. Of these patients, one (5.9%) was readmitted within 30 days after surgery owing to pulmonary infection (n=1). This infection was detected following a temperature increase on day 5 after discharge, at which time the patient went to the emergency department and chest CT scans revealed an infection necessitating hospital readmission. No patients experienced complications such as reoperation, chylothorax, or blood transfusion events within 30 days after surgery. Clinical results for these patients are summarized in Table 3. The primary postoperative symptoms for patients in the SDDL and InpL groups are shown in Figs. 2. On day 14 after surgery, symptoms for patients in both groups were notably alleviated, and the majority of these symptoms were absent by day 30 after surgery.
Patient characteristics.
SDDL=same day discharge lobectomy; InpL=Inpatient lobectomy; HisL= historical lobectomy; ASA= American anesthesia score; RMB=Renminbi; PC=Postoperative complications; SD= standard deviation; FEV1= Forced Expiratory Volume in the first second; FVC= Forced Vital Capacity; AD =adenocarcinoma; SCC= squamous carcinoma; RUL= right upper lobe; RML= right middle lobe; RLL=right lower lobe; LUL= left upper lobe; LLL= left lower lobe. Continuous data (normal distribution parameters) is shown as mean (SD), categorial data are shown as n (%).
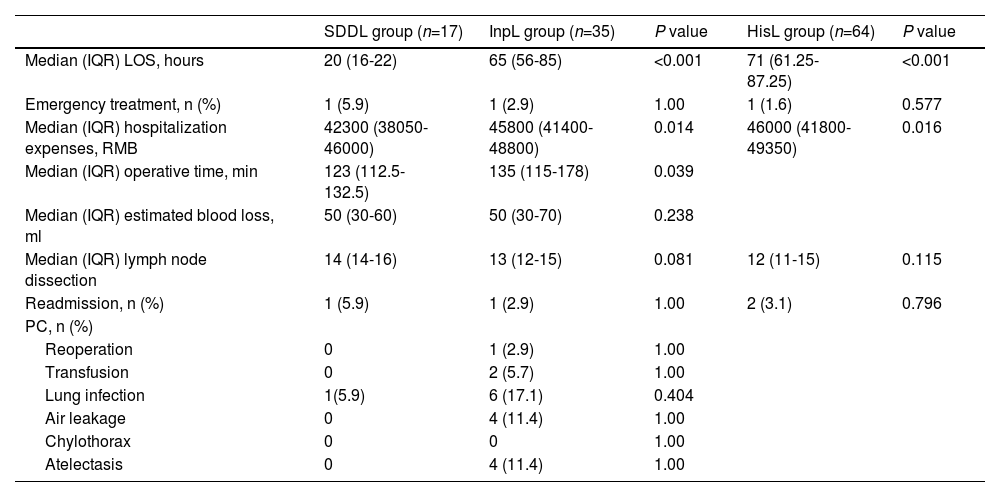
Clinical outcomes.
SDDL=same day discharge lobectomy; InpL=Inpatient lobectomy; HisL= historical lobectomy; RMB=Renminbi; LOS=length of stay; IQR= interquartile range; RMB=renminbi; PC=Postoperative complication. Continuous data (non-normal distribution parameters) are shown as Median (IQR), categorial data are shown as n (%).
No significant differences in baseline preoperative clinical characteristics were observed among groups (Table 2). As expected, the SDDL group exhibited the shortest postoperative LOS (median, 20 h; IQR, 16–22), whereas the median postoperative LOS in the InpL group was significantly longer (median, 65 h; IQR, 56-85) (P<0.001). The median postoperative LOS in the HisL group was 71 h (IQR, 61.25–87.25), and significant differences were observed among the three groups (P <0.001). There was a significant difference in total hospitalization costs between the SDDL and InpL groups (P=0.014) and between all three groups (P=0.016). The median operative duration in the SDDL group was also significantly less than that in the InpL group (P=0.039). No difference in postoperative complication incidence was observed when comparing the SDDL and InpL groups (P>0.05), although there was a non-significantly higher rate of postoperative pulmonary infections in the InpL group relative to the SDDL group. There was also a higher but non-significant increase in the proportion of readmissions and emergency visits in the SDDL group relative to the InpL and HisL groups (P>0.05).
DiscussionThe development of ERAS management practices has been conducive to the more efficient utilization of medical resources while simultaneously lowering medical costs and improving overall patient satisfaction.12 Accordingly, these ERAS approaches have been widely implemented in clinical settings, and the application of same-day discharge models further builds upon the advantages of this approach. The present study was developed to assess the safety and feasibility of same-day discharge among patients undergoing thoracoscopic lobectomy at our center. Of the 52 patients who were eligible, 17 (32.7%) completed same-day discharge after undergoing thoracoscopic lobectomy. None of these patients experienced any readmissions or emergency visits within 72 h following discharge, while 1 was readmitted on day 5 after surgery owing to the onset of a pulmonary infection. The remaining 94.1% of these patients did not exhibit any serious complications over the 30-day follow-up interval, and there were no significant differences in postoperative complication rates, emergency visits, or readmissions in the SDDL group relative to the InpL group. These results emphasize the safety and viability of using a same-day discharge model when managing a select group of thoracoscopic lobectomy patients, thereby maintaining low rates of complications, emergency visits, and readmissions.
Among the approximately one-third of participating patients in this study that completed same-day discharge, the primary clinical symptoms reported during follow-up were cough and chest pain, both of which were effectively managed using oral antitussive drugs and painkillers. These patients experience the alleviation of these clinical symptoms within 14 days after surgery, and these symptoms were absent in the majority of cases at 30 days after the procedure, in line with prior reports.13 This emphasizes the safety of this same-day discharge model. The potential for severe complications such as pulmonary embolism or active bleeding after discharge is a major potential concern for patients undergoing this form of expedited discharge. As such, the inclusion criteria for this study required the enrolled patients to remain within 30 minutes of the hospital for the 48 hours immediately following discharge. Patients were also directed to purchase a simple finger pulse oximeter, allowing them to monitor postoperative oxygen saturation and heart rate to provide preliminary insight into whether that patient is facing a critical situation. All of these measures were developed to maximize the post-discharge safety of participating patients. In prior studies, a mobile app was employed to remotely monitor colon surgery patients, but such an app may be inconvenient for widespread use and difficult to use for older individuals.14
To further gauge the viability of these study results, longitudinal and transverse comparisons were conducted, but no significant differences in preoperative clinical features were observed among these groups. The operative duration in the SDDL group was significantly lower than that in the InpL group (P=0.039), potentially owing to the highly selected nature of patients in the SDDL group. The number of lymph nodes dissected has previously been reported to impact the LOS for surgery patients,15 but no differences in lymph node dissection were detected among the three groups in this study. Relative to the SDDL group, a non-significantly higher risk of postoperative pulmonary infection was evident in the InpL group, in line with prior evidence that prolonged LOS may contribute to an elevated risk of hospital-acquired infection.16 As compared to the InpL group, patients in the SDDL group exhibited significant reductions in both LOS and hospitalization expenses. Wang et al. similarly confirmed that same-day discharge can reduce both LOS and hospitalization expenses, highlighting the advantages of this discharge model.17
The development of ERAS strategies has increasingly revolutionized clinical thinking regarding surgical procedures, spurring growing interest in the same-day discharge of patients undergoing a range of procedures. Same-day discharge models are used increasingly often following appendectomy, cholecystectomy, hysterectomy, and colon cancer resection.7,8,18,19 There have been few reports assessing the safety or feasibility of same-day discharge for patients undergoing thoracoscopic lobectomy, however. Jiang et al. retrospectively analyzed stage I non-small cell lung cancer patients undergoing lobectomy, wedge resection, or segmental resection, and found same-day discharge to be feasible and safe, with 87 (41.6%) patients ultimately completing the SDDL mode,10 this study is worthy of recognition. However, some of the patients included in this study cohort were discharged with a test tube, which is inconvenient and associated with a poorer safety profile. The study conducted by Dong et al. was also based on retrospective clinical analyses that demonstrated the safety and feasibility of same-day discharge for patients with early-stage lung cancer, with the SDDL mode being successfully completed for 127 (93.38%) patients.11 While this study enrolled far fewer cases than these two prior reports, it is nonetheless the first prospective analysis of the safety and feasibility of same-day discharge for patients undergoing thoracoscopic lobectomy.
Postoperative complication rates can be dramatically reduced through a combination of effective preoperative communication, the implementation of strict criteria for chest tube removal and discharge, and the application of stringent perioperative management measures. In this study, chest tube removal was based on a volume of < 100 mL in 12 h, with this value being lower than in other studies.20 Follow-up after discharge is also very important for patients that undergo same-day discharge. Here, a professional team performed all patient follow-up, and patients were required to preoperatively join a specific WeChat group. Following discharge, the medical team responded to any clinical questions raised by the patients. If emergencies arose, these doctors were also able to contact patients via video for risk assessment and to determine whether emergency treatment was necessary, thereby minimizing the risk to these patients to the greatest extent possible.
This study is subject to certain limitations. For one, patients who were eligible were permitted to elect to continue hospitalization in consideration of cultural and social factors, and fewer patients were included in the final study cohort as a result, with just 32.7% of patients electing to undergo same-day discharge. The patients in this study cohort were also highly selected, with just 45.6% (52/114) of them having met the study inclusion criteria. It is thus not feasible to extend the same-day discharge model to all patients, although the eligible patient population has the potential to be expanded through multidisciplinary perioperative cooperation and appropriate preoperative education. During the preparation of this manuscript, 10 additional patients in our center underwent same-day discharge, further supporting the safety and feasibility of this approach. However, this study had a relatively short follow-up interval, and further research will be vital to determine whether this same-day discharge mode has any impact on long-term patient survival or quality of life.
ConclusionThese results offer preliminary evidence that same-day discharge can be safe and feasible in a highly selected subset of patients undergoing thoracoscopic lobectomy. This approach represents a pronounced shift in the hospitalization strategy associated with this procedure, emphasizing the suitability of same-day discharge for certain patients scheduled to undergo thoracoscopic lobectomy provided sufficient preoperative education, refined perioperative management, and postoperative follow-up support from a professional team are available. This strategy has the potential to facilitate the better optimization of medical resource allocation while lowering patient medical costs and reducing the incidence of hospital-acquired infections.
CRediT authorship contribution statementYL Zheng: Conceptualization, Methodology, Formal analysis, Resources, Writing – original draft, Writing – review & editing, Funding acquisition. CC Wang: Methodology, Investigation, Writing – original draft, Writing – review & editing. LD Jin: Methodology, Investigation, Writing – original draft, Writing – review & editing. XY Liang: Methodology, Data curation, Writing – original draft, Writing – review & editing. WS Ye: Formal analysis, Writing – review & editing. RS Huang: Conceptualization, Methodology, Resources, Writing – original draft, Writing – review & editing, Funding acquisition.