The study aimed to analyze frequency and severity of adverse events (AEs) and other reasons for interruption of treatment and loss to follow up (LTFU) during first six months of treatment among tuberculosis patients on bedaquiline containing regimens.
MethodsThis pilot exploratory observational study included 275 patients enrolled consecutively over two years who received bedaquiline containing regimen under programmatic conditions in India.
ResultsAmong 275 patients with median age of 25 years, 86 (31.3%) patients had at least one interruption with 122 total episodes of interruption. Among these 70 were temporary, 35 were permanent interruptions and 17 were LTFU. The AEs due to drugs were the commonest reason for interruption observed in 81.4% of temporary interruption group and 97.1% of permanent interruption group. Among a total 192 adverse event episodes, (49.5%) were minor (grade 1–2) and (50.5%) were serious (grade 3–5). Personal factors were the commonest reason for interruption observed in LTFU (94.1%) group. The most common temporarily interrupted drug was bedaquiline in 8.7% and permanently stopped drug was linezolid in 5% of patients.
ConclusionsOur study observed that drug related AEs are important risk factors associated with treatment interruptions in bedaquiline containing regimens. Bedaquiline is the most common temporarily interrupted drug due to AEs.
Tuberculosis (TB) is a major public health problem worldwide. As per Global TB report 2019, globally 10 million people developed TB disease and about a quarter of those cases were reported from India in 2018.1 The proportion of cases who are infected with strains resistant to isoniazid and rifampicin, called multidrug-resistant tuberculosis (MDR-TB) among new and previously treated cases in India, were 2.8% and 14% respectively.1
Adherence to the long course of TB treatment is a complex, dynamic phenomenon with a wide range of factors impacting on treatment taking behavior.2 However, an estimated 50% of patients on long term therapy for chronic diseases, including TB, are non-adherent.3 Non-compliance leading to treatment interruption due to any reason may affect the outcome adversely.4 Multiple number of drugs leading to adverse events (AEs) in drug resistance TB (DR-TB), patients’ personal factors, TB programme related factors and environmental factors may be responsible for the interruptions and loss to follow up (LTFU) during the treatment period.5
Bedaquiline, is a novel drug recently approved for the treatment of tuberculosis. The addition of bedaquiline to an optimized background regimen (OBR) results in faster and significantly more culture conversions leading to higher successful outcome.6 The information about interruptions and AEs, especially with newer drugs and drug combinations, in bedaquiline containing regimen is sparse.7–9
The study aimed to analyze the frequency and severity of AEs and other reasons for interruptions of treatment and loss to follow up (LTFU) during the first six months of treatment among TB patients on bedaquiline containing regimens under programmatic conditions in India.
MethodsSettingThis was a pilot exploratory observational study. All patients, who received bedaquiline containing regimen through conditional access under programmatic management of drug resistant tuberculosis (PMDT) at a tertiary center in northern India were enrolled prospectively, over a period of two years from October 2016 to October 2018.
Study populationThe eligibility criteria for enrollment were adult patients with pulmonary DR-TB who required the addition of bedaquiline with/without other newer/repurposed drugs based on drug resistance pattern to construct an effective regimen as per recommendations of national programme for management of DR-TB.10
Ethical considerationsEthical and research approval was obtained from Institutional Research and Ethical Committee (office letter no. NITRD/PGEC/2018/6624 letter no. NITRD/RC/2018/5742 respectively).
DefinitionsIn this study, missed doses of all drugs or part of regimen (one or more drugs) was considered as interruption. The interruption was further classified into:
- 1
Temporary – If drug/drugs were restarted after interruption; temporary interruption was further classified as short if the duration of interruption was ≤2 days, and as long if the duration of interruption was >2 days to 30 days.11
- 2
Permanent – If drug/drugs were not restarted after interruption
- 3
Lost to follow up – If all drugs were discontinued for more than one month.10
The AEs of any drug involved in the treatment regimen were collected. According to the World Health Organization active drug safety monitoring project, serious adverse events (SAEs) include death or a life-threatening event, hospitalization or prolongation of hospitalization, persistent or significant disability, or congenital anomaly. SAEs included grade 3–5 AEs (grade 3: serious; grade 4: life threatening; grade 5: death). Minor AEs included those of grade 1 (mild) and grade 2 (moderate).7,12–14
Treatment regimenEnrolled patients received a treatment regimen of bedaquiline with companion drugs which were individually constructed based on drug resistance pattern as per recommendations of PMDT for management of DR-TB.10 Bedaquiline was given at 400 mg daily for two weeks and then 200 mg thrice weekly for 22 weeks.
Patient managementAfter obtaining informed written consent, eligible patients’ case summaries including demographic details, body mass index (BMI), drug susceptibility test report of National Reference Laboratory {available for rifampicin, isoniazid, pyrazinamide, second-line injectable drugs (i.e., amikacin, kanamycin, or capreomycin), flouroquinolones both low and high dose, cycloserine, ethionamide, clofazimine, linezolid and p-amino salicylic acid}, radiological profile including presence of cavity and extent of involvement as per National Tuberculosis Association of USA15 were recorded. Relevant blood investigations including serum electrolytes, thyroid function tests, audiometry, and baseline QTc in resting ECG using Fridericia's formula (QTcF) were done at baseline. ECG was repeated every week in first two months followed by monthly for next four months. Patients were monitored during the first six months of treatment period according to recommendations of PMDT for management of DR-TB.10 A designated treatment supporter visited the patient within 24 h of interruption, documented the episode and cause of interruption, and addressed the reason of interruption. Where he/she was unable to convince the patient, medical officer visited the patient’s house. If still unsuccessful, help was requested of district tuberculosis officer (DTO) to convince the patient to continue with treatment. All these issues were documented in patient treatment card. The interruption episodes which occurred during the first six months of treatment were studied for the type of interruption, whether temporary or permanent, duration for which the drug/drugs were interrupted and reason for interruption. The individual drugs which were interrupted, and organ system predominantly affected were also studied.
Data management and analysisPatient characteristics were summarized using frequencies and percentages for categorical variables, and median and interquartile ranges (IQRs) for continuous variables. Chi-square test was used to assess the relationship between categorical variables. Student t-test was used to test difference between proportions and means between study populations. Statistical analysis was done using Statistical Package for Social Sciences (IBM, Armonk, NY, USA) version 21.0. A p-value of <0.05 was considered statistically significant.
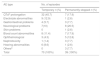
ResultsA total of 275 patients were enrolled. The demographic, radiological, microbiological characteristics, drugs used and number of drugs in the treatment regimen are summarized in Table 1. Among the 275 study subjects, 56.4% were males, median age was 25 (IQR, 21−36) years and median BMI was 18.73 kg/m2 [IQR, 15.5−20.16]. At treatment initiation, 63.6% had cavity in chest x-ray and 73.8% were Pre-XDR (MDR + Fluoroquinolone resistant – 70.2%; MDR + Injectable resistant – 3.6%). Patients having XDR TB {MDR-TB plus resistance to any fluoroquinolone and at least one of three second-line injectable drugs (i.e., amikacin, kanamycin, or capreomycin)} were 22.6%.
Baseline patient demographic, disease features, resistance pattern and drugs used in OBR of 275 study subjects.
| Patient demographic, disease features, resistance pattern and drugs used in OBR | n (%) |
|---|---|
| Age, years - median (range) | 25 (21−36) years |
| Male | 155 (56.4%) |
| BMI, kg/m2 - median (range) | 18.73 [15.5−20.16] |
| BMI - <18.5 kg/m2 | 122 (44.4%) |
| Addiction habits | 39 (14.2%) |
| Diabetes mellitus | 33 (12%) |
| Hypertension | 5 (1.8%) |
| Alcoholic liver disease | 3 (1.1%) |
| Chronic renal disease | 2 (0.7%) |
| Hypothyroidism | 2 (0.7%) |
| Seizure disorder | 2 (0.7%) |
| HIV-positive | 2 (0.7%) |
| Other Comorbiditiesa | 4 (1.5%) |
| Contact with a DR-TB case | 39 (14.2%) |
| Previously treated with second-line drugs | 163 (59.2%) |
| Cavities on chest x-ray | 175 (63.6%) |
| Bilateral disease on chest x-ray | 218 (79.3%) |
| DST profilePre-XDR-TB resistant to injectablePre-XDR-TB resistant to FQsXDR-TB Poly drug resistant | 10 (3.6%) 193 (70.2%) 62 (22.6%) 10 (3.6%) |
| Drugs used in OBR Linezolid ClofazimineSecond Line Injectable Ethionamide Cycloserine Pyrazinamide Moxifloxacin -High doseP-amino salicylic acid Amoxicillin-clavulanate Delamanid Imipenem Ethambutol Isoniazid -High dose Moxifloxacin -Normal dose Levofloxacin | 260 (94.5%) 242 (88%) 204 (74.2%) 186 (67.6%) 182 (66.2%) 132 (48%) 119 (43.2%) 70 (25.5%) 58 (21.1%) 47 (17.1%) 45 (16.4%) 21 (7.6%) 8 (2.9%) 8 (2.9%) 2 (0.7%) |
| Number of drugs in the regimen 5 drugs 6 drugs 7 drugs 8 drugs 9 drugs | 14 (5.1%) 80 (29.1%) 146 (53.1%) 31 (11.3%) 4 (1.4%) |
BMI – Body mass index; DR-TB- Drug resistant tuberculosis; DST – Drug sensitivity test; XDR – Extensive drug resistant; FQs- Fluoroquinolones; OBR -optimized background regimen.
Among the 275 patients, interruption episodes occurred in 86 (31.3%) patients with 122 total episodes of interruption. Out of 86 patients, 21 (24.4%) patients had more than one interruption episode. Out of 275 patients, 17 (6.2%) patients were LTFU, 33 (12%) patients had permanent interruption and 50 (18.2%) had temporary interruption. Among the interruption episodes, 70 (57.4%) were temporary interruptions, out of which 56 (80%) episodes were long interruptions. Among 122 interruption episodes, 78.7% episodes occurred after two weeks of treatment period.
Reasons for interruptionsThe various factors analyzed for reasons of interruptions were drug related AEs, personal, provider and environmental related factors and are summarized in Table 2. The AEs due to drugs was the commonest reason in temporary (81.4%) and permanent (97.1%) interruption groups whereas personal factors were the commonest reason in LTFU (94.1%) group. The service provider and environmental related factors were not associated with any interruption episode.
Reason for interruptions in various episodes.
| Reasons | Any interruptionn (%) | Temporary interruption of any drug n (%) | Permanent interruption of ≥1 drug n (%) | LTFUn (%) |
|---|---|---|---|---|
| Drug related AEs | 92 (75.4%) | 57 (81.4%) | 34 (97.1%) | 1 (5.9%) |
| Personal factors | 30 (24.6%) | 13 (18.6%) | 1 (2.9%) | 16 (94.1%) |
| 1 (0.8%) | 0 | 0 | 1 (5.9%) |
| 18 (14.8%) | 13 (18.6%) | 0 | 5 (29.4%) |
| 1 (0.8%) | 0 | 1 (2.9%) | 0 |
| 10 (8.2%) | 0 | 0 | 10 (58.8%) |
| Total | 122 (100%) | 70 (100%) | 35 (100%) | 17 (100%) |
LTFU – lost to follow up; AEs - adverse events.
A total of 192 episodes of AEs occurred within first six months of treatment in 109 patients (Table 3). Out of these 192 episodes, 95 (49.5%) were classified as minor (grade 1–2) and 97 (50.5%) were classified as serious (grade 3–5). However, only 92 of these episodes of AE were associated with interruption. The type of AEs leading to temporary or permanent interruption episodes is shown in Table 4. The most common AEs in temporary and permanent interruption episodes were QTcF prolongation (45.7%) and nervous system (20.5%) related AEs, respectively.
Classification of adverse drug reactions as per Common Terminology Criteria for Adverse Events.
| Adverse events (%) | Grade | No. of episodes n (%) |
|---|---|---|
| Minor | I – Mild | 30 (15.6%) |
| II - Moderate | 65 (33.9%) | |
| Serious | III - Severe or medically significant | 95 (49.5%) |
| IV - Life-threatening consequences | 2 (1.0%) | |
| V - Death related to AEs | 0 | |
| Total | 192 |
Type of Adverse event associated with temporary and permanent interruption episodes.
| AE type | No. of episodes | |
|---|---|---|
| Temporary n (%) | Permanently stopped n (%) | |
| QTcF prolongation | 32 (45.7) | 7 (17.9) |
| Electrolyte abnormalities | 9 (12.9) | 1 (2.6) |
| Gastrointestinal problems | 4 (5.7) | 3 (7.7) |
| Neurological problems | 7(10) | 8 (20.5) |
| Skin problems | 0 | 1 (2.6) |
| Blood count abnormalities | 8 (11.4) | 7 (17.9) |
| Ophthalmological | 3 (4.3) | 5 (12.8) |
| Nephrotoxicity | 1 (1.4) | 3 (7.7) |
| Hearing abnormalities | 6 (8.6) | 1 (2.6) |
| Othersa | 0 | 3 (7.7) |
| Total | 70 (100%) | 39 (100%) |
AE – Adverse Event; QTcF - QTc in resting ECG using Fridericia's formula.
Among the drugs associated with temporary and permanent interruptions, bedaquiline was the most common temporarily interrupted drug (8.7%), the mean duration of stoppage being 5.4 days. Linezolid was the most common permanently stopped drug (5%).
Effect of interruption on interim treatment outcome and mortalityAfter excluding 17 LTFU patients for interim outcome analysis, the interim successful outcome among non-interrupters and interrupters at the end of six months of treatment were 86.8% and 81.2% respectively. However, the difference was not statistically significant (p = 0.260). 33 (12%) patients expired within six months of treatment initiation and more than half (57.6%) of these expired within first three months. As per the assessment by causality assessment committee of the institute none of the deaths was found to be causality related to AEs due to drugs. Also 22 (66.7%) patients among those who died were culture converted before death.
DiscussionThis is the first observational study on treatment interruption patterns and various reasons for interruptions during the first six months of treatment among DR-TB patients from a TB endemic country who received a bedaquiline containing regimen under the national TB programme. This study also analyzed the frequency and severity of AEs due to anti-TB drugs in this cohort of patients.
The study observed that among the 275 patients, around one third of patients had treatment interruption episodes, in more than half of these patients the interruptions were temporary, and three-quarters of the interruptions were due to drug related AEs. The commonest drugs associated with temporary and permanent interruption episodes were bedaquiline (8.7%) and linezolid (5%), respectively. A retrospective study done by E. Sanchez-Padilla et al.16 found drug related AEs (11.6%) and need for return to work (24.4%) as the main cause for interruptions.
Personal factors like busy schedule, lack of family support and no improvement with treatment were the major causes (94.1%) for interruption in LTFU group. More than half of the patients (59%) interrupted treatment due to no or slow response, as many of these patients had advanced disease at baseline. Every effort should be made to retrieve these patients at the earliest and restart the treatment in timely manner. It is important that patients be actively counselled by treatment supporter on each visit to continue with the treatment.
In our study, no interruptions were observed due to service delivery and environmental related factors, thus highlighting the relatively good performance of PMDT services in study area. However, in a study by I. Zão et al.17 healthcare system related factors were one of the reasons for delay in diagnosis and management of TB patients although less common than patient related factors.
In our study, QTc prolongation was more frequent than reported in bedaquiline-treated patients in previous studies,14,18–21 possibly because most patients (96.4%) received one or more additional QTc-prolonging drugs such as moxifloxacin (high dose) (43.2%), clofazimine (88%) or delamanid (17.1%). However, majority of the events were associated with dyselectrolytemia and once corrected, bedaquiline could be reintroduced in the majority of patients. Although bedaquiline was associated with temporary treatment interruptions in around 8.7% of patients, it required permanent discontinuation in only 2.9% of patients, indicating bedaquiline may have good safety profile. However, a retrospective study by Lorenzo Guglielmetti et al.22 found that bedaquiline was permanently discontinued in 6.7% patients due to QTc prolongation.
In our study, linezolid required permanent discontinuation in 5% patients out of total 260 patients who received linezolid in their regimen. These observations are similar to studies by N. Ahmad et al.,23 Z. Lan et al.24 and R. Singla et al.25 which found that linezolid was associated with SAEs more often compared to other drugs used in the treatment regimen. Anemia was the significant SAE responsible for permanent interruption of linezolid in our study, similar to findings in systematic review and meta-analysis done by G. Sotgiu et al.26 Therapeutic drug monitoring can be utilized to measure drug levels in patients receiving long term linezolid therapy.
There are concerns regarding the use of bedaquiline and delamanid together in patients having extensive level of drug resistance beyond XDR-TB because of increased propensity for cardiotoxicity. Delamanid was used as one of companion drugs in 17% of such patients in our study, but it required permanent discontinuation in only two patients. This indicates that the addition of delamanid to bedaquiline containing regimen may not lead to significant increase in SAEs. Efficacy of this combination could not be evaluated in this study.
In India as per PMDT guidelines, patients on bedaquiline containing regimen need to be more closely monitored during first two weeks of treatment.10 However, it was observed that almost 80% of interruptions were reported after second week of treatment initiation and these interruptions were mainly due to drug related AEs. Hence, all patients on bedaquiline containing regimen need intense monitoring by the treatment supporters during follow up even after two weeks of treatment. Directly observed treatment (DOT) improves adherence to TB treatment by identifying AEs earlier and manages them appropriately. In a systematic review and meta-analysis by Toczek et al.27 lower default rates for drug-resistant TB were seen with DOT.
Twelve percent of the patients expired within six months of treatment initiation which was very similar to the studies done by Sergey E. Borisov et al.28 (13.4%) and Kathryn Schnippel et al.29 (12.6%). The India TB report 2019, at national level, also shows a death rate of 14%.30 Mortality is higher in patients with advanced or disseminated forms of TB and as found by L. Meira et al31 in their study that 36% of patients who died in first six months of TB treatment had disseminated disease. Similarly, poor general condition and severe form of disease were the main cause for mortality rather than treatment failure in patients who died, thus indicating the good efficacy of these drugs.
The interim successful outcome was 80% at the end of six months of treatment. These results are far better than the previously reported successful outcomes among the severe forms of DRTB patients treated with conventional regimens in India.32 This may indicate that bedaquiline added to a background regimen can improve the rate of successful outcome among severe DRTB patients. The successful outcome was higher in patients among non-interrupters group, although it was not statistically significant.
The strengths of this study are that this is the first study analyzing various reasons of treatment interruptions in the first six months of treatment of bedaquiline containing regimens especially in high TB burden countries, like India, under programmatic conditions. Secondly the safely profile and QTc prolongation effect of bedaquiline given along with other QTc prolonging drugs in a large number of patients was also analyzed. This study also had significant number of patients on bedaquiline with delamanid combination, with or without other QTc prolonging drugs, and showed a reassuring safety profile when used together as part of a multi-drug regimen.
There were some limitations of this study. The patients in this study cohort represented most patients with severe disease with extensive drug resistance pattern. Extrapolation of results to other MDR-TB patients without extensive disease, and extensive resistance patterns may not be appropriate.
To conclude, the study observed that drug related AEs and personal factors are the most important risk factors associated with treatment interruptions. Hence, it is important to identify AEs earlier and manage them appropriately. Although, the treatment outcome among non-interrupters was better, it was not statistically significant. Hence, larger studies may be required to evaluate this.
Conflict of interestNone.
Author contributionRupak Singla and Sekar Natarajan conceived this study and supervised all aspects of its implementation. Neeta Singla and Jose A. Caminero collaborated in the inception of the study. Amartya Chakraborty carried out the analysis of the data. Amitesh Gupta and Vikas Kumar collected the data and collaborated in the analysis. All the authors contributed to the interpretation of the results and the proof reading of the manuscript.
Funding/ GrantNone.