The Pulmonology Service of a Central Hospital in Lisbon created a Unit dedicated to the treatment of tuberculosis (TB).
ObjectivesCasuistic analysis and assessment of the predictive factors for in-hospital mortality, over a 10-year period.
DesignRetrospective study, from April 1999 to September 2009, through the Statistical Package for the Social Sciences application for binary logistic regression.
ResultsIn a total of 1917 patients, most were male (n=1450; 76%), Caucasian (76.6%), with an average age of 43±15.2 years, and 19.8% were immigrants. The retreatments were responsible for 26% of the hospitalizations. The presence of comorbidities was detected in 85.7%, particularly HIV infection (34.7%). The multidrug-resistant (MDR) and the extensively drug resistant (XDR) TB occurred in 6.6% and 6.8%, respectively. The average delay was 28.5±54.8 days, with the mortality rate at 8.6%. The mortality risk was more significant amongst men (OR 1.8; 95% CI 1.16–2.90; p<0.01), in patients with HIV infection (OR 3.7; 95% CI 2.47–5.49; p<0.001), and amongst those who presented MDR TB (OR 2.5; 95% CI 1.24–5.15; p<0.01) and XDR TB (OR 5.5; 95% CI 3.14–9.58; p<0.001).
ConclusionA high percentage of patients presented comorbidities, namely HIV infection. The main factors associated with mortality were HIV infection, XDR TB and MDR TB.
O Serviço de Pneumologia de um Hospital Central de Lisboa criou uma Unidade dedicada exclusivamente ao internamento de casos de tuberculose (TB).
ObjectivosAnálise casuística e avaliação dos factores preditivos de mortalidade intra-hospitalar, num período de 10 anos.
Material/MétodosEstudo retrospectivo, entre Abril de 1999 e Setembro de 2009, através da aplicação SPSS (Statistical Package for the Social Sciences) para a regressão logística binária.
Resultados: Do total de 1917 doentes, a maioria era do sexo masculino (n=1450; 76%), caucasiana (76,6%), com média de idades de 43±15,2 anos, e 19,8% de imigrantes. Os retratamentos foram responsáveis por 26% dos internamentos. A presença de comorbilidades foi encontrada em 85,7%, salientando-se a infecção pelo VIH (34,7%). A TB multirresistente (MR) e a extensivamente resistente (XDR) surgiu em 6,6% e 6,8%, respectivamente. A demora média foi de 28,5±54,8 dias e a taxa de mortalidade de 8,6%. O risco de mortalidade foi maior entre os homens (OR 1,8; IC 95% 1,16–2,90; p<0,01), nos doentes com infecção VIH (OR 3,7; IC 95% 2,47–5,49; p<0,001), e nos que apresentaram TB MR (OR 2,5; IC 95% 1,24–5,15; p<0,01) e XDR (OR 5,5; IC 95% 3,14–9,58; p<0,001).
ConclusõesUma elevada percentagem dos doentes apresentava comorbilidades, nomeadamente a infecção VIH. Os principais factores associados à mortalidade foram a infecção VIH, a TB XDR e a TB MR.
Even in the 21st century tuberculosis (TB), a treatable condition, is an infectious disease that still has one of the world's highest mortality rates,1 which corresponds to about 28/100,000.2
According to the 2008 World Health Organization (WHO) report, some 9.4 million new cases were documented worldwide in 2006, with an incidence of 139/100,000.2 It is estimated that about 7.7% were human immunodeficiency virus (HIV) infected.
In Portugal, in 2009, 2565 new cases of TB were diagnosed, with an incidence of 24.1/100,000.3 The mortality rate due to tuberculosis, in 2008, was 5.3%.4 Over the last decade, an average annual decrease of 7.3% has been achieved. As for the prevalence of Acquired Immunodeficiency Syndrome (AIDS) in patients with a TB diagnosis, in 2009, 13% of co-infected patients were reported, thus representing the largest percentage in all of the European Countries that report this condition.
One of the major problems in the fight against TB is the resistance of the Mycobacterium tuberculosis (Mt) to several anti-TB drugs, particularly Isoniazid and Rifampicin, thus defining and constituting TB's biggest threat ever: multidrug-resistance. In March 2006, an even more severe strain was detected, resistant additionally to second-line drugs (first-line drugs and any fluoroquinolone, and to at least one of the three following injectable drugs: capreomycin, kanamycin and amikacin), which was given the name extensively drug resistant TB (XDR TB).5
According to WHO data, in 2007, the existence of about 500,000 cases of multidrug-resistant TB (MDR TB) was estimated.6 At the European level, more than 70,000 cases develop multidrug-resistance annually.3
In Portugal, the incidence of MDR TB has been decreasing, representing an average of 1.7% of the total number of TB cases in 2009 (1.2% in new cases and 7.3% in retreatments), with a ratio comparable to the European Union average. In December 2009, there were 63 cases of MDR TB, 24% of which with XDR criteria.3
Due to the high prevalence and incidence of TB in Portugal by the end of the 20th century, in April 1999, the Pulido Valente Hospital created a Unit exclusively dedicated to the admission of TB patients.
The aim of this review was to analyse the casuistic and predictive factors of in-hospital mortality in this unit.
Materials and methodsThe authors conducted a retrospective study of all the patients admitted to the Tuberculosis Unit with TB, from April 12th, 1999, to September 30th, 2009.
The criteria for admission in the unit were: severe forms of presentation, existence of comorbidities, severe adverse reactions to therapy, poor socio-economic conditions and cases of bacillary MDR and XDR TB.
All the data used in the study were obtained from discharge notes and the diagnoses complied with the International Classification of Diseases, 10th Revision (ICD-10).
We present a description of the population and an analysis of its demographic characteristics, a classification of record and notification of TB suggested by the WHO, prior personal history of TB, main diagnosis, comorbidities, description of the adverse reactions to the anti-TB therapeutics, sensitivity standards, average delay, status at discharge and mortality.
For a statistical analysis, the differences between the groups of category variables were assessed by means of the chi square test (χ2) and the numerical variables through the t test. As for the factors associated with mortality, an analysis of binary logistic regression was performed. The application used was the Statistical Package for the Social Sciences programme, 15.0 version. The binary regression data are presented with Adjusted Odds Ratios (ORA), with the respective confidence intervals of 95% (CI) and the p values.
ResultsIn the period between April 12th, 1999, and September 30th, 2009, 1917 patients were admitted in the Tuberculosis Unit. Of these 1450 cases were male (76%).
The average age was 43±15.2 years (between 16 and 95 years of age). The average age for males was significantly higher than the age average of females (43±14.1 years vs 41±18.1 years; p<0.001).
It should be pointed out that 759 patients (39.6%) were between ages 35 and 49. It was also noted that the age groups with more male and female incidence were the 35-to-44 (29.9%) and 25-to-34 (30.2%) age groups, respectively.
Most of the population was Caucasian (n=1469; 76.6%) and of Portuguese nationality (n=1537; 80.2%). Only 380 patients (19.8%) were foreigners.
The immigrants were mostly male (n=292; 76.8%), and of African origin (n=299; 78.7%) in both genders. Only seven (1.8%) came from Western Europe. The 299 African immigrants were mostly from Portuguese-speaking countries.
As for occupation, 50.7% belonged to the active population group. Of these, most were factory workers and unskilled workers (n=764; 78.6%) and only 3.1% (n=30) belonged to senior or upper management levels. It should be pointed out that a significant proportion of the patients (n=682; 35.6%) were unemployed and 222 (11.6%) were retired.
The characteristics of the 1917 patients are summarized in Table 1.
Characteristics of the 1917 patients with tuberculosis.
| Patient characteristics | n (%) |
| Age group (years) | |
| 16–24 | 151 (7.9) |
| 25–34 | 513 (26.8) |
| 35–49 | 759 (39.6) |
| 50–70 | 368 (19.2) |
| >71 | 126 (6.6) |
| Sex | |
| Male | 1450 (75.6) |
| Female | 467 (24.4) |
| HIV infection | |
| Positive | 665 (34.7) |
| Negative | 1252(65.3) |
| Sites of infection | |
| Pulmonary TB | 1485 (77.5) |
| Extra-pulmonary TB | 422 (22.5) |
| Lymphatic | 221 (52.4) |
| Pleural | 144(34.1) |
| Miliar | 121 (28.7) |
| CNS | 23 (5.5) |
| Larynx | 17 (4) |
| Others | 54 (12.8) |
| WHO classification | |
| New cases | 1418 (74) |
| Retreatments | 499 (26) |
| Country of birth | 380 (19.8) |
| Angola | 109 (36.5) |
| Cape Verde | 98 (32.8) |
| Guinea-Bissau | 58 (19.4) |
| Mozambique | 16 (5.4) |
| Sao Tome & Principe | 13 (4.3) |
| Others | 86 (22.6) |
HIV=human immunodeficiency virus; TB=tuberculosis; CNS=central nervous system; WHO=World Health Organization.
Of the 1917 patients diagnosed with TB, 74% (n=1418) were new cases and 26% (n=499) corresponded to retreatment cases. These were mostly due to recurrences (49.7%) and to interruption in prior treatments (38.5%).
From a radiological perspective, the most frequent presentation within the cases of pulmonary TB was the cavitary variety. The various presentations of extra-pulmonary TB are shown in Table 1.
Only 274 patients (14.3%) did not present other associated pathology. The remaining 85.7% (n=1643) had at least one comorbidity. The most frequent ones were metabolic/nutritional changes (n=773; 47%) and addictive behaviours (n=663; 40.4%), namely alcoholism (n=410; 61.8%) and drug addiction (n=326; 49.2%).
Another comorbidity with great impact among this population was HIV infection, present in 665 patients (34.7%) and, of these, 528 (79.4%) were male. This group was mostly Caucasian (n=502; 75.5%); immigrants accounted for 18.2% (n=121), mostly African (n=108; 89.3%) from Cape Verde (n=36; 29.8) and Guinea-Bissau.
Of the 425 patients with HIV who had their CD4 levels counted, 311 (73.2%) had less than 200cells/mm3, with the average number being significantly lower compared to the group of patients without HIV co-infection (162±192.1 vs 747.7±349.4; p<0.001), which confirms those patients’ deficient immunity.
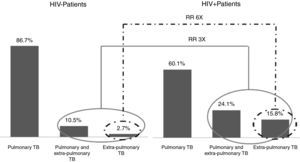
When comparing the types of TB presentation between the group of patients with HIV and those not infected by this virus, we noticed that, although the distribution is very similar, amongst HIV+ patients the occurrence of exclusively extra-pulmonary TB and mixed types is much more frequent (Fig. 1).
In this study, it was also noted that in 213 patients (12%) there were adverse reactions to therapy. The most frequent were the hepatic reactions (n=102; 47.9%) and hypersensitivity (n=61; 28.6%). Most adverse reactions occurred in HRZE schemes (Isoniazid+Rifampicin+Pyrazinamide+Ethambutol).
It is important to point out that adverse reactions were more frequent in patients with HIV (13.7%) than in non-infected patients (9.7%).
We obtained the results from the TB-drug sensitivity tests (DST) in 1492 (77.8%). Of these, 1129 (75.7%) showed sensitivity to all first-line anti-TB drugs. The mono-resistance (particularly to streptomycin) was found in 131 patients (8.8%) and poly-resistance in only 32 (2.1%). In 98 patients (6.6%) the DST presented a multidrug-resistance pattern, with XDR TB in 102 patients (6.8%).
A feature of patients with MDR TB showed that about 78 (80%) were Portuguese, 38 (38.8%) were infected with HIV, and 40 patients (40.8%) had a history of drug abuse. Most corresponded to cases of retreatment (n=52; 53.1%). In this group of patients, 70 (71.4%) were discharged due to an improvement in their clinical status; the mortality rate was 11% (n=11).
As far as XDR TB is concerned, most individuals (n=86; 84.3%) were also Portuguese and 67 (65.7%) were infected with the HIV virus. Also in this group, 43 (42.2%) presented drug addiction. Only 20 (19.6%) were new cases, with the remaining 82 (80.4%) belonging to retreatment. In this group of patients, 62 (60.8%) were discharged due to an improvement in their clinical status; the mortality rate was 25.5% (n=26).
When comparing patients with and without HIV infection, we noticed that the number of XDR TB within the first group was 3.6 times higher than within the second group (10.1% vs 2.8%).
We also noticed that retreatment cases increased 5.6 times the risk of developing strains of MDR or XDR TB and that HIV infection increases that risk 2.3 times, compared to patients with new cases of TB.
Concerning the status of the patients at discharge, 1636 patients (85.3%) were discharged due to an improvement in their clinical status. In this group of patients, 91.9% (n=1504) did not show multidrug resistance, 4.3% (n=70) were MDR TB cases and only 3.8% (n=62) were XDR TB.
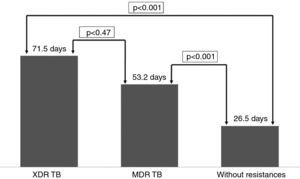
Patients’ average lenght of in the hospital, which was 28.5±54.8 days, was slightly longer for women compared to men, but with no statistical significance (30.5 days vs 27.9 days; p<0.16). The average lenght of analysed according to sensitivity patterns, as well as the respective levels of significance, can be found in Fig. 2.
In this sample, the average lenght of of TB patients without HIV infection did not show statistically significant differences compared to those co-infected with HIV (28.4±45 vs 32.9±35.1; p<0.093).
The mortality rate was 8.6% (n=165). Of the deceased, 139 patients (84.2%) were male; the average age was significantly higher compared to patients who were discharged (48.7±17.2 years vs 42±14.9 years; p<0.001), and most of them did not have any prior history of TB (n=116; 70.3%).
Of the 165 deaths, 112 patients (68%) had three or more comorbidities and 94 (57%) were infected with HIV, while 65 (73%) experienced drug addiction. Other comorbidities frequently found amongst the deceased included pulmonary thromboembolism (n=17; 10.3%), diabetes mellitus (n=15; 9.1%) and neoplasms (n=14; 8.5%).Amongst HIV+ patients who died, the average CD4 count was 78.3±109.4cells/mm3, and amongst HIV+ patients who survived it was 173.2±198cells/mm3 (difference with statistical significance; p<0.001).
The analysis of the factors associated with in-hospital mortality consisted of a binary logistic regression model, in which the dependent variable was mortality and the independent variables were male gender, HIV infection, MDR TB and XDR TB. Table 2 shows the results of the analysis, indicating the adjusted odds-ratios and respective confidence intervals.
Analysis of binary logistic regression for the mortality amongst patients with tuberculosis.
| Variables | Ajusted odds-ratio (95% CI) | p value |
| Male sex | 1.831 (1.155–2.901) | <0.01 |
| HIV infection | 3.679 (2.465–5.491) | <0.001 |
| MDR TB | 2.530 (1.244–5.148) | <0.01 |
| XDR TB | 5.487 (3.143–9.579) | <0.001 |
HIV=human immunodeficiency virus; MDR TB=multidrug-resistant tuberculosis; XDR TB=extensively drug resistant tuberculosis; CI=confidence interval.
Results show that XDR TB and HIV infection had a greater impact on life expectancy. MDR TB and the male gender were also significantly correlated with the likelihood of death.
The data analysed correspond to the total of admissions during the 10 years. The authors considered it important to highlight the results divided into two major periods of 5 years (Table 3). In the last five years there were decreases in the number of hospitalizations (but no significant differences in the average stay), HIV infection, numbers of retreatment, cases of MDR or XDR TB and in-hospital mortality. So, currently, there is a better control of the disease.
DiscussionAs expected, and according to the epidemiology of TB in Portugal,3 in this Unit most cases were detected in males, with the largest proportion amongst young adults and individuals with the poorest socio-economic conditions.
The ratio of immigrants in this study (19.8%) was slightly higher than the percentage found in 2009 in Portugal (15%).3 This probably reflects an increased need for admission of these patients due to the low socio-economic support.
The importance of immigration has been shown to be quite variable in different case studies. We should point out that in the one conducted in 2001 in a Spanish Hospital (Madrid)7 only 9% were immigrants, while a study published by a hospital in Paris8 revealed that immigrants accounted for 43.6%.
In our case study, the forms of pulmonary TB were the most prevalent, although the extra-pulmonary forms also carried significant weight amongst HIV+ patients, which agrees with what is described in the available literature. Miliary TB is also prominent, along with the forms of pleural TB and lymphatic-intrathoracic TB.
In 2009 13% of TB and AIDS cases were recorded in Portugal. As expected, the percentage obtained in these 10 years of operation was substantially higher (34.7%); this figure is easily explained by the urgent need to admit these patients into hospital. The figures for co-infection published in other case studies range from 6.9%8 to 43.6%.7
In this study, the incidence of adverse reactions to anti-TB drugs (12%) was relevant, as they were higher than in some previously published studies.9 This finding is probably due to the high number of comorbidities associated with these patients. It should be pointed out that alcoholism was a significant comorbidity, which may also contribute towards the development of drug hepatotoxicity.
The high number of retreatments (26%) is quite striking. We draw attention to the need for an increasingly strict control of patients receiving outpatient treatment and who respond favourably to the therapy, in order to deter the development of multidrug-resistant strains.
Since this Unit was specially designed for the admission of MDR/XDR cases, the rates (6.6% and 6.8%, respectively) were much higher compared to national data (2%).3 With regard to other case studies,8,10–13 our results were almost always higher, and only in relation to the study in Madrid were lower (30%).7
Our global average lenght of stay (28.5 days) was substantially higher compared to other studies,12,13 presumably due to the larger number of MDR and XDR TB cases admitted and also due to the high number of comorbidities.
Compared to other studies,14,15 which show a hospital mortality rate between 5 and 30%, the rate found in this unit (8.6%) was close to the best numbers ever recorded. We refer to the Madrid study7 with very similar results (9%), and the Brazil case study10 with considerably higher numbers (18.4%).
Mortality was mostly associated with males, HIV co-infection, the comorbidities and with the MDR and XDR strains of TB.
ConclusionsWe can conclude that, to control TB cases, the screening tests amongst younger age groups are of utmost importance, particularly when associated with risk factors, such as addictions, HIV infection, poor socio-economic conditions and immigration from countries with high prevalence of TB; thus, in the control of TB needs the maintenance of outpatient support structures (TB and HIV antiretroviral therapy programme) is crucial.
The existence of units exclusively dedicated to the admission of patients with MDR TB and XDR TB is of emerging importance and a burning contemporary issue. To that end, we need to restructure these units in order to improve the quality of patient isolation, with no multi-bed wards.
It is important for policymakers, clinicians and administrators to be involved in the infection control of TB, so as to avoid potential nosocomial transmission of MDR and XDR TB cases.
Conflict of interestThe authors declare they have no conflict of interest.
Please cite this article as: Lopes, T. Casuística de dez anos de actividade (1999–2009). S0873-2159(11)00073-0.