Delayed diagnosis and treatment of tuberculosis contributes to the spread of the disease. In this study, we aimed to determine the patient and healthcare system delay among tuberculosis patients in Portugal and identify associated factors at individual and contextual level.
MethodsWe analysed all TB cases notified in Portugal between 2010 and 2014 using data from the national surveillance system. Patient and healthcare system delay were computed, log-transformed, and used as outcomes. Adjusted generalized linear models were fitted to identify sociodemographic, contextual and clinical determinants.
ResultsThe study included 6838 patients. The median of patient and healthcare system were 33 and 17 days, respectively. Adjusted regression models revealed that higher patient delay occurred in foreign patients (exponentiated beta: 1.177, 95%CI 1.091–1.270) and those addicted to alcohol (1.169, 1.072–1.276) and drugs (1.153, 1.027–1.295). Higher healthcare system delay was observed among patients with extra-pulmonary TB (2.067, 1.885–2.268) and pulmonary comorbidities – lung cancer (2.391, 1.656–3.452), sarcoidosis (3.316, 1.370–8.022) and COPD (1.295, 1.059–1.584) – and in patients residing further from a healthcare service (1.040, 1.018–1.062).
ConclusionWe found that various individual and contextual factors affect the time delay in tuberculosis treatment. Our findings indicate that some strategies, such as facilitating the access to healthcare services among foreign patients and patients with addictions and increasing the awareness towards TB among healthcare professionals, may result in better TB control.
Tuberculosis (TB) is a major public health problem: in 2016 there were an estimated 10.4 million cases worldwide.1 Despite the 22% decrease in the number of deaths between 2000 and 2015, TB is still one of the ten main causes of death worldwide.1 In 2015, the number of TB notifications in Europe represented 3% of notifications worldwide.2 Portugal stands out in the western European context for having one of the highest TB rates.2 In 2016, there were 1836 TB notifications in Portugal, representing a notification rate of 17.8 per 100,000 habitants.3 The End Tuberculosis Strategy, by the World Health Organization (WHO), aims to reduce the TB incidence rate by 90% and the number of deaths by 95% until 2035.1 Despite the decrease in the TB incidence in the last fifteen years, the current decline rate is still insufficient to achieve the WHO target.1
Several studies have demonstrated that the delay in TB diagnosis and treatment constitutes a major obstacle to TB control. Diagnosis and treatment delay increases the morbidity and mortality associated with TB and increases the period of infectiousness, fuelling TB transmission. Diagnosis and treatment delay of TB may be attributed to the patients and to healthcare systems characteristics.4–17 Patients may postpone seeking medical aid and the healthcare services may delay in recognizing and suspecting the disease. Demographic, socioeconomic and clinical factors may influence the delay in diagnosis and initiation of treatment5–8,10–22 and identifying and understanding these factors is crucial to make TB control programs more efficient. Unfavourable social and economic conditions, lower accessibility to the healthcare system, as well as TB associated factors, such as human immunodeficiency virus (HIV) co-infection, alcohol and drug addiction, malnutrition contribute to increasing TB transmission.23 Notice that Portugal has one of Europe's highest TB/HIV co-infection rates and the geographical areas of highest TB incidence are those with a high HIV infection rate, and a high unemployment and immigration rate.3,19
Although there are several studies on TB diagnosis and treatment delay, the majority was conducted in low-income countries, where the TB epidemic and the socioeconomic and healthcare systems are of a different nature.4–6,9,19,20,23–25 Studies from high-income countries are rare, and the majority focus on clinical and demographic factors, disregarding socioeconomic and contextual determinants.4,7–16 In Portugal, specifically, more studies are needed to understand the factors that influence TB treatment delay to make TB control programs more effective.
Given the previous gaps, we aimed to determine the patient and healthcare system delay in TB patients and to identify associated factors at individual and contextual level in Portugal.
MethodsData sources, outcomes and sample selectionWe analysed all TB cases notified in Portugal between 2010 and 2014 using data from the national surveillance system for TB (SVIG-TB).26
Patient and healthcare system delays were defined as outcomes. Patient delay denotes the time interval between the onset of symptoms and the first contact with healthcare system services; healthcare system delay the time interval from the first contact with healthcare services to the beginning of treatment; treatment delay is the sum of the two.4,5
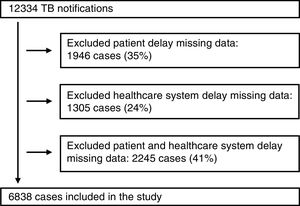
We excluded from the study the cases that had missing information in the patient delay, health care system delay or in both. As shown in Fig. 1, between 2010 and 2014, 12,334 TB cases were notified, but 5496 were excluded from the present study due to missing data: 35% due to missing information required to compute the patient delay and 24% due to missing information required to compute the healthcare system delay and 41% due to both.
Although effect sizes were rather small, excluded participants were more likely to have a drug addiction, to be in prison and to be homeless (see Supplementary Material 1).
CovariatesBoth individual and contextual variables were considered. The individual variables included were age, sex, place of birth, occupation, homelessness, incarceration, alcohol or other drugs addictions and clinical characteristics, more specifically pulmonary or extra-pulmonary TB involvement, HIV co-infection, other non-pulmonary comorbidities (kidney failure, lymphoma, auto-immune disease, diabetes, hepatic disease, cancer from other organs and other non-pulmonary diseases), silicosis, lung cancer, sarcoidosis and chronic obstructive pulmonary disease (COPD).
Occupations were classified according to the International Standard Classification of Occupations (ISCO-08) and grouped into three ordinal classes of decreasing social prestige and economic power: upper white collar (ISCO-08=1–3), lower white collar (ISCO-08=4–5), and blue collar (ISCO-08=6–9) occupations. The occupation class reflects to some extent the educational level of the patients, their earnings and their occupational exposures, variables that are not collected by SVIG-TB.27
Urbanity level was determined according to the classification of the urban areas, published by the Statistics Portugal in 2014. This classification groups the Portuguese civil parishes into three classes: predominantly urban areas, moderately urban areas and predominantly rural areas.28
The European deprivation index (EDI) was used to classify the civil parishes according to their level of socioeconomic deprivation.29,30 In Portugal, it resulted from the weighted sum of the following standardized variables: % overcrowded households, % households with no bath/shower, % households without indoor flushing, % households occupied by non-owners, % women aged 65 or more, % individuals with low education, % individuals in low-income occupation, and % unemployed individuals. The index was also categorized into quintiles (Q1-least deprived to Q5-most deprived).30
To estimate geographical accessibility to healthcare, the shortest road distance from the patient's civil parish to the nearest healthcare facility (primary care centres, hospitals or chest disease centres) was calculated using ArcGIS version 10.4.1 and the Network analyst extension following methods reported elsewhere.31
Statistical analysisFor the descriptive analysis, we calculated the median and interquartile range (IQR), as well as counts and proportions.
Since the variables patient delay and healthcare system delay did not follow a normal distribution, these were log-transformed.
For group comparisons, effect size was measured using Cohen's f. Values around 0.1, 0.25 and 0.4 correspond to small, medium and large effect sizes, respectively.32
Then, a multivariable linear regression was fitted to adjust for multiple risk factors. The backward stepwise method of variable selection was used, i.e., all variables were included in the initial model and they were then successively eliminated based on the Akaike Information Criteria (AIC), so that the final model presented the best fit.
Associations were presented as exponentiated beta coefficients and corresponding 95% confidence intervals.
Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS), version 24, and using R (package ‘powerAnalysis’).
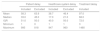
ResultsAmong the 6838 included patients (65.2% male), patient delay, healthcare system delay and treatment delay (the sum of the healthcare system delay and treatment delay) medians were 33 (IQR=51), 17 (IQR=40) and 68 (IQR=72) days, respectively (Table 1).
Mean, median, interquartile range, minimum and maximum of patient delay, healthcare system delay and treatment delay (days) of patients included and excluded from the study.
| Patient delay | Healthcare system delay | Treatment delay | |||
|---|---|---|---|---|---|
| Included | Excluded | Included | Excluded | Included | |
| Mean | 58.3 | 63.9 | 38.7 | 46.4 | 97.0 |
| Median | 33.0 | 45.0 | 17.0 | 21.0 | 68.0 |
| IQR | 51.0 | 50.0 | 40.0 | 50.0 | 72.0 |
| Minimum | 1 | 0 | 1 | 1 | 3 |
| Maximum | 995 | 818 | 947 | 960 | 1480 |
IQR – interquartile range.
Table 2 presents the sample characteristics and the patient and healthcare system delays according to patient individual and contextual characteristics. Patient delay was higher in foreign patients. The majority of foreign patients are originally from the former Portuguese colonies in the African continent (70.2%), especially from countries with high TB incidence rate, such as Angola, Cabo Verde, Guiné-Bissau, Moçambique and São Tomé e Príncipe. Patient delay was also higher in patients with alcohol or drug addiction, and lower among older and younger patients, among patients with non-pulmonary comorbidities, blue-collars, residents in moderately urban or predominantly rural areas and at a longer distance from a healthcare service. Healthcare system delay was higher in older patients, in those with extra-pulmonary TB, pulmonary and non-pulmonary comorbidities, among patients from predominantly rural areas, and at longer distances from the healthcare services; and it was lower in male, foreign and homeless individuals, patients with HIV infection and patients with alcohol and drugs addiction. It is important to note that, except for the variable TB involvement, effect sizes were generally small.
Median of patient and healthcare system delays (days) according to patient characteristics.
| Variables | n (%) | Patient delay | Healthcare system delay | ||
|---|---|---|---|---|---|
| Median | Effect size f | Median | Effect size f | ||
| Sex | |||||
| Men | 4458 (65.2) | 34.0 | 15.0 | ||
| Women | 2380 (34.8) | 32.5 | 0.01 | 22.0 | 0.11 |
| Place of birth | |||||
| Portugal | 5660 (83.0) | 32.0 | 18.0 | ||
| Foreign country | 1162 (17.0) | 40.0 | 0.07 | 13.0 | 0.06 |
| Age group | |||||
| <18 | 261 (3.8) | 27.0 | 12.0 | ||
| 18–39 | 2284 (33.4) | 36.0 | 13.0 | ||
| 40–69 | 3177 (46.5) | 35.0 | 17.0 | ||
| ≥70 | 1115 (16.3) | 29.0 | 0.08 | 30.0 | 0.17 |
| Urbanity level | |||||
| Predominantly urban | 5452 (79.9) | 35.0 | 17.0 | ||
| Moderately urban | 809 (11.9) | 29.0 | 16.0 | ||
| Predominantly rural | 564 (8.3) | 30.0 | 0.07 | 22.0 | 0.04 |
| Socioeconomic deprivation | |||||
| Q1 – least deprived | 2669 (39.2) | 35.0 | 18.0 | ||
| Q2 | 1512 (22.2) | 32.5 | 17.0 | ||
| Q3 | 956 (14.1) | 31.0 | 17.0 | ||
| Q4 | 846 (12.4) | 33.0 | 18.0 | ||
| Q5 – most deprived | 820 (12.1) | 34.5 | 0.05 | 14.0 | 0.03 |
| Distance to healthcare | |||||
| Less than 1km | 1883 (27.6) | 36.0 | 15.0 | ||
| 1–2km | 3236 (47.4) | 35.0 | 17.0 | ||
| More than 2km | 1706 (25.0) | 30.0 | 0.09 | 18.0 | 0.04 |
| Occupation | |||||
| Upper white-collars | 743 (19.8) | 36.0 | 17.0 | ||
| Lower white-collars | 889 (23.7) | 36.0 | 19.0 | ||
| Blue-collars | 2119 (56.5) | 31.0 | 0.05 | 19.0 | 0.03 |
| Incarceration | |||||
| No | 6659 (99.1) | 33.0 | 17.0 | ||
| Yes | 63 (0.9) | 35.0 | 0.004 | 15.0 | 0.01 |
| Homelessness | |||||
| No | 6656 (99.1) | 33.0 | 17.0 | ||
| Yes | 62 (0.9) | 32.0 | 0.01 | 8.0 | 0.04 |
| TB involvement | |||||
| Pulmonary | 5551 (81.8) | 34.0 | 14.0 | ||
| Extra-pulmonary | 1238 (18.2) | 33.0 | 0.001 | 33.0 | 0.22 |
| Silicosis | |||||
| No | 6750 (98.7) | 33.0 | 17.0 | ||
| Yes | 88 (1.3) | 31.0 | 0.01 | 21.0 | 0.01 |
| Lung cancer | |||||
| No | 6773 (99.0) | 33.0 | 17.0 | ||
| Yes | 65 (1.0) | 30.0 | 0.01 | 49.0 | 0.06 |
| Sarcoidosis | |||||
| No | 6826 (99.8) | 33.0 | 17.0 | ||
| Yes | 12 (0.2) | 26.0 | 0.004 | 56.0 | 0.02 |
| COPD | |||||
| No | 6613 (96.7) | 34.0 | 17.0 | ||
| Yes | 225 (3.3) | 31.0 | 0.01 | 26.0 | 0.03 |
| HIV infection | |||||
| No | 6168 (90.2) | 33.0 | 17.0 | ||
| Yes | 670 (9.8) | 33.0 | 0.002 | 15.0 | 0.04 |
| Other non-pulmonary comorbiditiesa | |||||
| No | 4820 (70.5) | 35.0 | 15.0 | ||
| Yes | 2016 (29.5) | 31.0 | 0.03 | 22.0 | 0.07 |
| Alcohol addition | |||||
| No | 5766 (87.4) | 33.0 | 18.0 | ||
| Yes | 834 (12.6) | 37.5 | 0.04 | 10.0 | 0.09 |
| Drugs addition | |||||
| No | 6096 (92.1) | 33.0 | 18.0 | ||
| Yes | 522 (7.9) | 37.0 | 0.03 | 10.0 | 0.09 |
Table 3 shows the results from multivariable regression. Patient delay is increased by being foreign (exponentiated beta: 1.177, 95%CI 1.091–1.270), and addicted to alcohol (1.169, 1.072–1.276) or drugs (1.153, 1.027–1.295) and decreased by residence in moderately urban areas (0.865, 0.791–0.946), distance from healthcare facilities (0.961, 0.942–0.979), and having HIV infection (0.893, 0.807–0.987) and other non-pulmonary comorbidities (0.935, 0.878–0.996). Healthcare system delay, on the contrary, was negatively associated with being foreign (0.876, 0.795–0.966), and addicted to alcohol (0.772, 0.691–0.863) or drugs (0.799, 0.689–0.927), together with area socioeconomic deprivation (0.974, 0.958–0.991), and positively associated with extra-pulmonary TB (2.067, 1.885–2.268) and pulmonary comorbidities – lung cancer (2.391, 1.656–3.452), sarcoidosis (3.316, 1.370–8.022) and COPD (1.295, 1.059–1.584) – and with distance from a healthcare service (1.040, 1.018–1.062).
Association (exponentiated beta coefficients and 95% confidence intervals) between TB treatment delays (log-transformed) and individual and contextual variables (multivariable analysis).a
| Variables | Patient delay | Healthcare system delay |
|---|---|---|
| Exp beta (IC95%) | Exp beta (IC95%) | |
| Place of birth | ||
| Portugal | Ref. | Ref. |
| Foreign country | 1.177 (1.091–1.270) | 0.876 (0.795–0.966) |
| Urbanity level | ||
| Predominantly urban | Ref. | |
| Moderately urban | 0.865 (0.791–0.946) | |
| Predominantly rural | 0.955 (0.850–1.073) | |
| Socioeconomic deprivation score | 0.974 (0.958–0.991) | |
| Distance to healthcare (km) | 0.961 (0.942–0.979) | 1.039 (1.017–1.062) |
| Homelessness | ||
| No | Ref. | |
| Yes | 0.769 (0.567–1.043) | |
| TB involvement | ||
| Pulmonary | Ref. | |
| Extra-pulmonary | 2.067 (1.885–2.268) | |
| Lung cancer | ||
| No | Ref. | |
| Yes | 2.391 (1.656–3.452) | |
| Sarcoidosis | ||
| No | Ref. | |
| Yes | 3.316 (1.370–8.022) | |
| COPD | ||
| No | Ref. | |
| Yes | 1.295 (1.059–1.584) | |
| HIV infection | ||
| No | Ref. | Ref. |
| Yes | 0.893 (0.807–0.987) | 0.900 (0.790–1.025) |
| Other non-pulmonary comorbiditiesa | ||
| No | Ref. | Ref. |
| Yes | 0.935 (0.878–0.996) | 1.083 (0.999–1.174) |
| Alcohol addition | ||
| No | Ref. | Ref. |
| Yes | 1.169 (1.072–1.276) | 0.772 (0.691–0.863) |
| Drugs addition | ||
| No | Ref. | Ref. |
| Yes | 1.153 (1.027–1.295) | 0.799 (0.689–0.927) |
aAdjusted for sex and age.
The present study aimed to determine the patient and healthcare system delay in tuberculosis patients in Portugal and identify associated factors. Median patient delay (33 days) was longer than healthcare system delay (17 days), totalizing a total median of 68 days between the onset of symptoms and the beginning of treatment. According to a systematic review of studies from high income countries, the median of patient delay, healthcare system delay and total treatment delay were 25.8, 21.5, and 61.3 days respectively.4 In Portugal, a study conducted in 2012, revealed higher mean values for patient delay and healthcare system delay than the ones observed in our study (patient delay: 92 vs 58.3 days; healthcare system delay: 56 vs 38.7 days). However, this investigation was a single centre study conducted during a two months’ time period.8 Our results corroborate those obtained in studies from high-income countries, where patient delay is usually longer than the healthcare system delay.7,11,12,15
We found that various individual and contextual factors affect TB treatment delay. The individual-level factors associated with increased patient delay were foreign nationality and addictions. Foreign patients face many difficulties in legalization process, have unfavourable socioeconomic conditions and may have a more limited access to healthcare services (due to both cultural and economic barriers).33 Individuals with addictions are also less likely to visit the healthcare services.34 On the other hand, as shown in others studies, from the time these patients are first seen, the time to diagnosis and the time to the beginning of treatment are lower because of the high suspicion index.10,11,14 This is especially relevant in Portugal, as many of these foreign patients are from countries of high TB incidence, namely from the ex-colonies. High suspicion index also explains why addicted patients go later to the healthcare services, but have lower healthcare system delays.6,13,24
Individual factors, such as older age, presence of extra-pulmonary TB and pulmonary comorbidities also contribute to increase healthcare system delays. Although older patients go earlier to healthcare services, the diagnosis is delayed due to the presence of multiple comorbidities. As in other studies, the presence of extra-pulmonary TB and comorbidities increases healthcare system delays, because of the multiple clinical presentations that make diagnosis difficult.14,22 The coexistence of other pulmonary diseases may delay the TB diagnosis, since they share many of the signs and symptoms. Sarcoidosis is a good example, because like TB it is a granulomatous disease, with a similar clinical, radiological and histologic presentation.
In the present study we observed that contextual determinants affected TB treatment delay, although in a different direction to what has been reported so far. It is important to mention that most studies that analysed the impact of contextual determinants have been conducted in low income countries, where socioeconomic factors and geographical accessibility have a major impact in healthcare provision.5,20,21
For instance, we observed that patient delay was lower in patients living in rural and moderately urban areas, which was, in part, explained by the predominance of older people in rural areas. Future research should evaluate further reasons for this association. The patient delay was also lower in the patients who live further from healthcare services. The distances to health services in Portugal are short (average distance 1.8km, minimum 300m, maximum 34.5km). This distance was calculated in relation to the healthcare service closest to the patient residence, whether it is a primary, secondary or tertiary healthcare service. In addition to the fact that primary health care in Portugal is widespread throughout the national territory, a large percentage of TB cases occurred in the large metropolitan areas, where the abundance of healthcare services is greater, contributing to reduction of the distances presented in this study. On the contrary, the healthcare system delay was higher among patients living further from the healthcare services. These patients reside mainly in rural areas, where accessible healthcare centres have fewer human and material resources. This is reflected in the lower access to medical appointments and in the need to refer patient to other centres with more resources, which may contribute to increase the healthcare system delay.
In our study, residence in most economically deprived areas was associated with a lower healthcare system delay. Disadvantaged socioeconomic conditions contribute to the increase in TB transmission, increasing the suspicion index by physicians towards patients from economically deprived areas and therefore speeding the diagnosis.23
The present study presents several limitations that merit further discussion. The main limitation is the large number of missing data on patient delay and/or healthcare system delay – only half of the TB patients were included. Lack of data on treatment delay might result from difficulties in defining the date of symptom onset or from incomplete file completion. Although differences were small, excluded patients were generally younger, with a higher exposure to TB risk factors and with more disadvantaged socioeconomic conditions. Since some of these covariates were associated with increased treatment delays, the exclusion of these participants could have led to an underestimation of the treatment delays, particularly patient delay. Besides, because patient delays were determined retrospectively and the date of symptoms may not be easy to locate, patient delay estimates could have been affected by recall bias. Regarding terminology, although we used the term ‘delay’ for the sake of comparison with international literature, we acknowledge that in some cases it corresponds to the expected time between symptoms and healthcare contact or first healthcare contact and treatment and not a true delay.
Yet the present study has several strengths. First, we analysed the impact of both individual and contextual determinants and we gave great emphasis to the socioeconomic determinants of health, a top priority nowadays. Second, we used the SVIG-TB database, a very powerful and solid source of data at a national level. Finally, we analysed separately the correlates of patient and healthcare system, since we acknowledged that the factors that affect each of these dimensions would be different given the different players involved.
ConclusionsIn conclusion, although the median delay in diagnosis and in the initiation of treatment in Portugal matches what has been reported in other high-income countries, there is still room for improvement, especially in certain sociodemographic and clinical groups. Our findings suggest that it is important to promote policies that facilitate access of foreign patients to healthcare services, and implement strategies that facilitate TB diagnosis and control in high-risk groups, such as patients with alcohol or drug addiction. On the other hand, there should be an increase in awareness of TB among healthcare professionals, especially in patients where the diagnosis of TB may be more difficult, such as older patients with comorbidities and patients with extrapulmonary TB. The results from this study may contribute to a new analysis on the TB transmission dynamics, and to reformulate prevention and control strategies.
FundingThis study was funded by FEDER through the Operational Programme Competitiveness and Internationalization and national funding from the Foundation for Science and Technology – FCT (Portuguese Ministry of Science, Technology and Higher Education) under the EPIUnit – Instituto de Saúde Pública, Universidade do Porto, Porto, Portugal (POCI-01-0145-FEDER-006862; Ref. UID/DTP/04750/2013).
Conflicts of interestNone declared.
The authors are grateful to Marta Gomes (Vila Nova de Gaia/Espinho Hospital Center) for providing the database for the statistical analysis.