Spontaneous pneumothorax is a rare complication of lung cancer and an even rarer form of presentation.1,2 Furthermore, there is no consensus regarding the pathophysiological mechanisms behind this association.
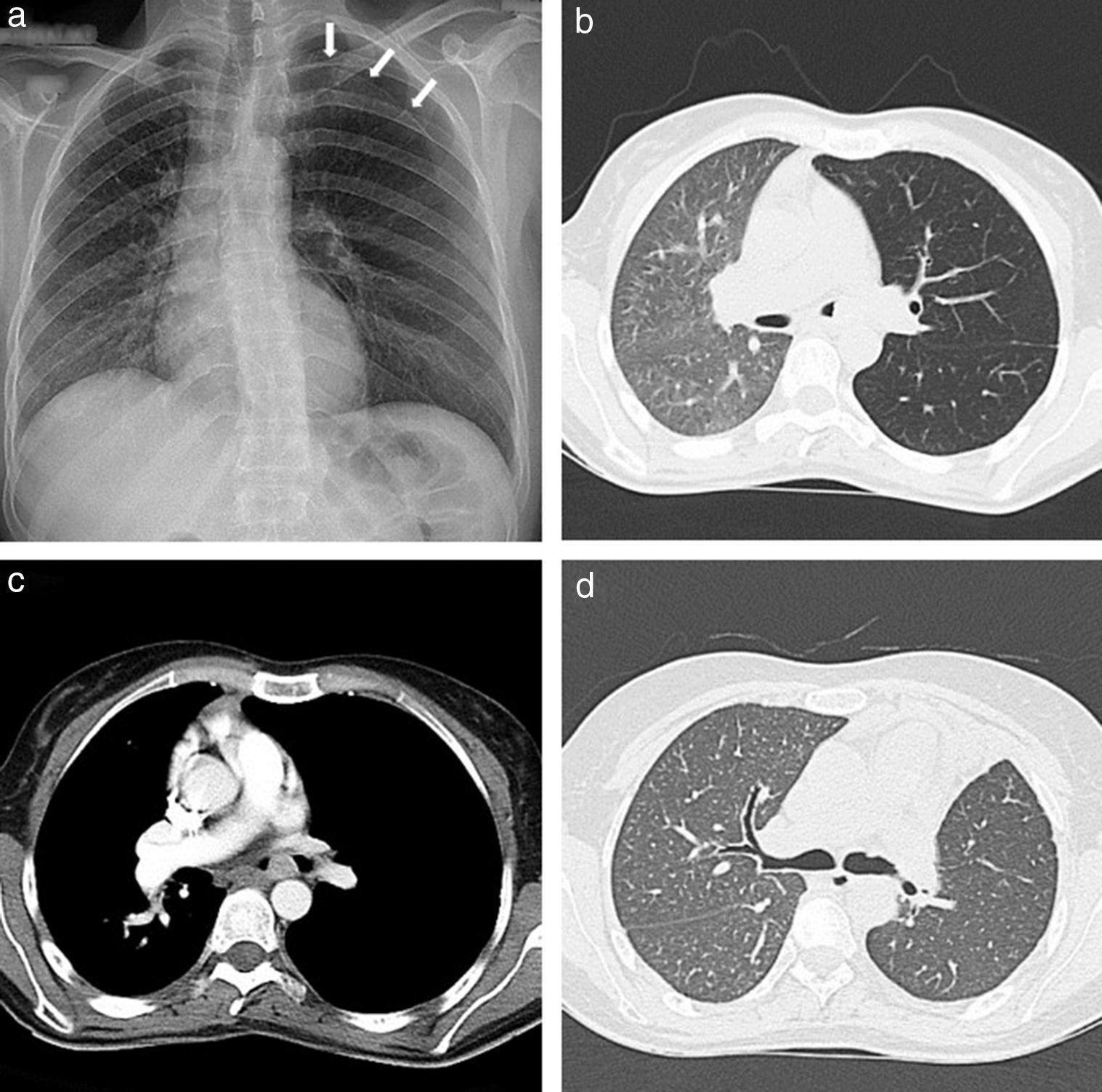
We report the case of a 30-year-old woman who presented to the emergency department of our hospital center with complaints of a recent left side pleuritic chest pain and a history of cough over the past 2 months. She was a non-smoker. Physical examination and chest radiograph indicated a left side pneumothorax (Fig. 1a). An intercostal tube was inserted; the lung fully expanded without any detectable air-leak and the chest tube was removed. At discharge the patient was asymptomatic and chest radiograph showed no abnormalities. Two months later she returned with new onset hemoptysis. Chest radiograph showed a small left side pneumothorax and increased ipsilateral lung volume with a contralateral mediastinum shift, both of which increased with expiration. A chest computed tomography (CT) confirmed these alterations with significantly decreased ipsilateral lung attenuation and showed a 2cm lesion in the left main bronchus (Fig. 1b and c). Bronchoscopy showed a cherry red polypoid tumor, easily hemorrhagic, causing an almost total obstruction of the left main bronchus. Biopsy of the tumor indicated a typical carcinoid tumor. An octreotide scan revealed uptake solely in the lesion of the left main bronchus and so a sleeve-type surgery was performed with excision of the main bronchus and lobectomy of left upper lobe. Histological examination confirmed a typical carcinoid tumor of the left main bronchus and showed no signs of emphysema or pleural blebs. The post-surgical period was insignificant and the patient was discharged home. Eighteen months after surgery she is asymptomatic, had no new pneumothoraces and her chest CT shows resolution of the mediastinum shift and similar bilateral lung attenuations (Fig. 1d).
a) Chest radiograph showing a left side pneumothorax (arrows). b) Chest CT showing increased left lung volume with contralateral mediastinum shift and decreased ipsilateral lung attenuation. c) Chest CT showing a 2 cm lesion in the left main bronchus. d) Chest CT, eighteen moths after surgery, showing resolution of the mediastinum shift and similar bilateral lung attenuations.
Bronchial carcinoid tumors are rare accounting for 1–5% of all lung malignancies3 and usually present with evidence of bronchial obstruction (obstructive pneumonitis or atelectasis), cough or hemoptysis.3 The occurrence of a spontaneous pneumothorax as a complication of lung cancer is also rare, comprising only 0.05–1.4% of all pneumothoraces1,4 and occurring in just 0.05–0.46% of patients with pulmonary malignancy.1,2 In the majority (75–100%) of cases reported in lung cancer patients, spontaneous pneumothorax preceded the diagnosis of lung cancer,1,5 but there are reports of its occurrence during chemotherapy or radiotherapy.6,7 The association between lung cancer and pneumothorax has been reported for most histologic types of lung cancer1; however, it seems there is no previous description of a pneumothorax complicating a bronchial carcinoid tumor or of a bronchial carcinoid tumor presenting with a pneumothorax. The proposed mechanisms for this association have been the appearance of a bronchopleural fistula secondary to necrosis and invasion of the pleura by a peripheral tumor and, less frequently, the rupture of alveoli, emphysematous bullae or subpleural blebs due to hyperinflation of the peripheral airways caused by the tumor acting as a check-valve.1,7 In the reported case radiology shows hyperinflation of the left lung, leading to contralateral mediastinum shift increasing with expiration. We propose that the polypoid tumor in the left main bronchus functioned as a variable obstruction (check-valve), leading to an inability to fully exhale the inspired air volume from the left lung. This trapped air in association with the expiratory maneuvers caused an increase in alveolar pressure with rupture of alveoli and formation of a pneumothorax associated with ipsilateral lung hyperinflation. This is also supported by the fact that the patient was a young nonsmoker, with no history of lung disease, had no signs of pleural blebs or emphysema on histologic examination, and that, after removal of the bronchial carcinoid tumor, there was resolution of the ipsilateral hyperinflation and there were no new pneumothoraces.
This is a singular case of a bronchial carcinoid tumor presenting with a recurrent spontaneous pneumothorax explained by a large check-valve mechanism. Also, the reported case strengthens the safe approach in which recurrent pneumothoraces should be considered secondary, and search for a cause should be actively sought.