Benign endobronchial tumors are uncommon. Bronchoscopic removal is the preferred modality of treatment although surgery may be required in some cases. Rigid bronchoscopy is usually recommended in the management of these tumors. However, flexible bronchoscopy is also used in many centers. We present a case of endobronchial lipoma, where an unusual complication during flexible bronchoscopic resection using snare forceps necessitated urgent rigid bronchoscopy. This case highlights the importance of rigid bronchoscopy in the management of endobronchial tumors. We believe that with a large benign endobronchial tumor in tracheal or main-stem bronchus, physicians should initially employ rigid bronchoscopy, switching to flexible if more peripheral treatment is required.
Os tumores endobrônquicos benignos são raros. A remoção broncoscópica é a modalidade de tratamento preferida, embora a cirurgia possa ser necessária em alguns casos. A broncoscopia rígida é geralmente considerada a modalidade preferencial na abordagem destes tumores. No entanto, a broncoscopia flexível também é utilizada em muitos centros. Apresentamos um caso de lipoma endobrônquico, onde uma complicação invulgar durante a ressecção broncoscópica flexível utilizando pinças de laço necessitou de uma urgente broncoscopia rígida. Neste caso, destaca-se a importância da broncoscopia rígida na abordagem dos tumores endobrônquicos. Acreditamos que com um tumor endobrônquico benigno de grandes dimensões da traqueia ou do brônquio principal, os médicos devem inicialmente utilizar a broncoscopia rígida, alternando para a flexível, se for necessário um tratamento mais periférico.
Benign lung tumors comprise 2-5% of all lung tumors, of which adenomas and hamartomas are the most common.1,2 Benign endobronchial tumors are rare and the exact prevalence of these tumors remains unknown. These tumors are characterized by a slow growth rate and generally present with dry cough and wheezing. In fact, they are often misdiagnosed as asthma or chronic bronchitis and can remain undetected for months or years.3 Because of the frequent absence of hemoptysis, these tumors often grow quietly and obstruct a major part of the tracheal lumen before symptoms like dyspnea, wheezing and stridor develop. Computed tomography (CT) and magnetic resonance imaging (MRI) have emerged as useful non-invasive diagnostic tools especially in detection of fat containing lesions.4 Flexible bronchoscopic biopsy has a low diagnostic yield in many benign tumors because of the presence of a covering capsule. Bronchoscopic resection can be diagnostic as well as curative because of the benign nature of the tumor.5 A variety of flexible and rigid bronchoscopic techniques has been used for the removal of these tumors, and is generally considered the preferred mode of treatment of these tumors.5,6 We here present a case of endobronchial lipoma, where an unexpected complication occurred during FB and necessitated urgent rigid bronchoscopy. We also review the bronchoscopic management of endobronchial lipomas.
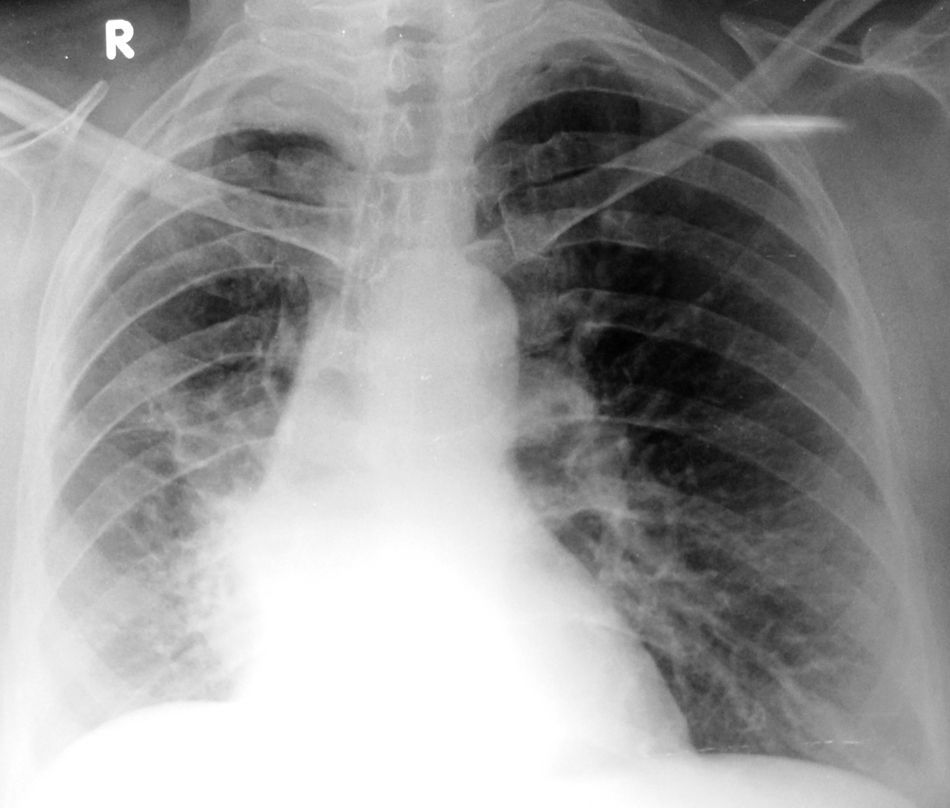
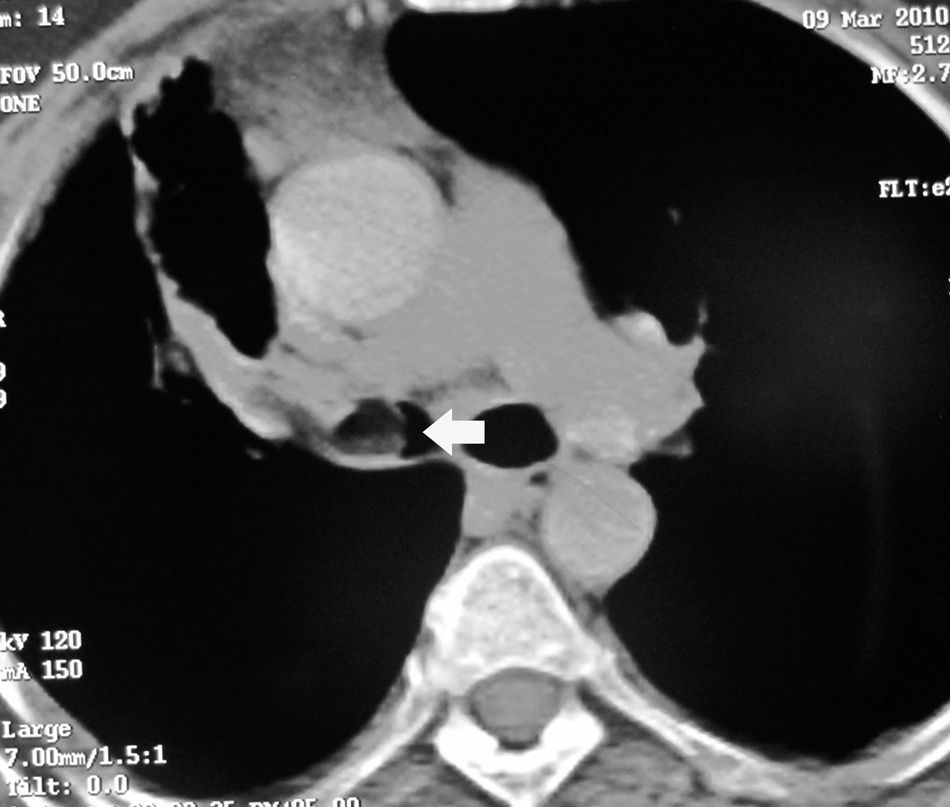
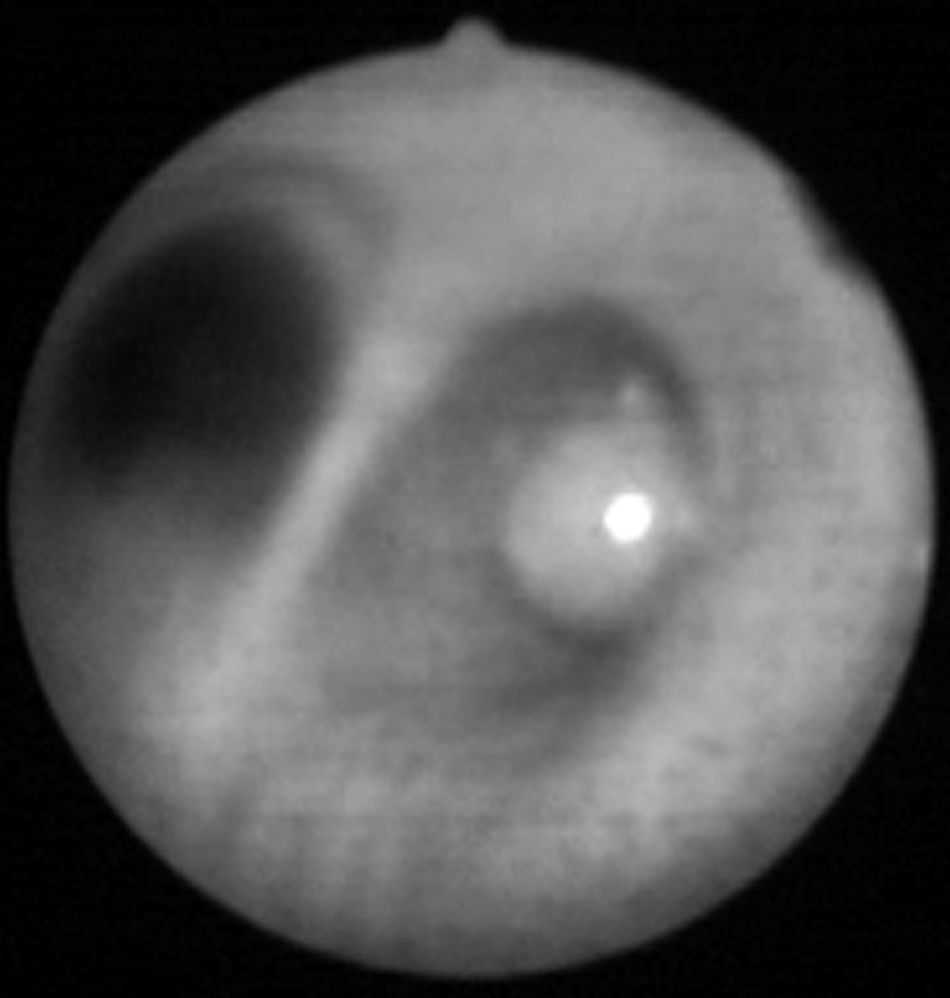
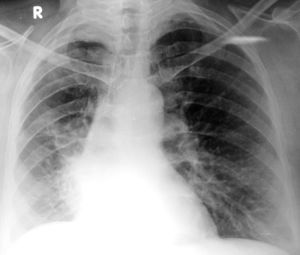
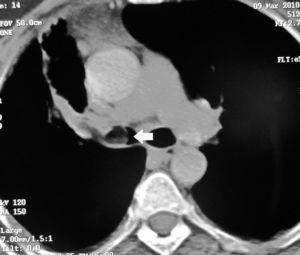
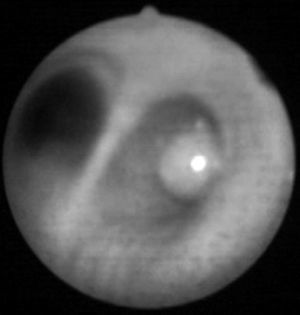
Case reportA 48-year old lady presented to the Chest Clinic with complaints of dry cough of six months duration. There was no history of fever, dyspnea, chest pain, wheeze or hemoptysis. She denied any addictions. Physical examination was unremarkable. Pulse oximetric saturation was 99% on room air. A chest radiograph was suggestive of volume loss in the right hemithorax (Fig. 1). Computed tomography (CT) of the thorax showed a low attenuation tumor in the right main bronchus suggestive of a fat containing lesion (Fig. 2). FB revealed the presence of a yellowish tumor with a smooth external surface causing near total occlusion of the right main bronchus (Fig. 3). The right upper lobe bronchus was not visualized and the bronchoscope could not be advanced into the right main bronchus. The patient was advised to have a rigid bronchoscopic removal of the tumor however she was not willing to have a general anesthesia.
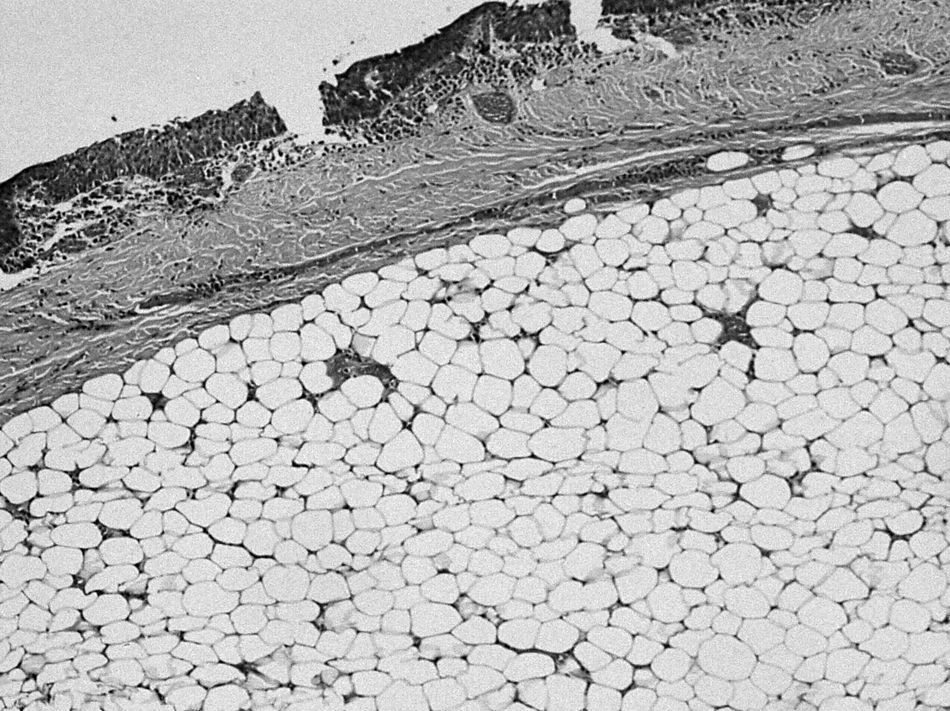
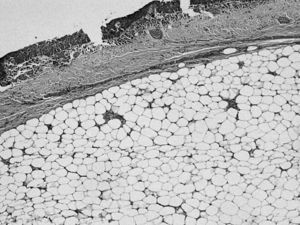
As a result it was decided to perform a flexible bronchoscopic removal of the tumor in the bronchoscopy suite. A wide channel bronchoscope (Pentax FB-19TV, Asahi Optical Co., Japan) was used and electrosurgical excision of the tumor was performed using the snare wire (Pentax DH2711S, Asahi Optical Co., Japan). However, before the tumor could be extracted, patient had a bout of coughing and the tumor slipped into the left main bronchus. During the next 3-5minutes, the patient became hypoxic, required endotracheal intubation and was shifted to the respiratory ICU. Despite mechanical ventilation, the oxygen saturation could be maintained at only 75-80%. As hypoxemia continued, FB was performed through the endotracheal tube and the growth was pushed into the left lower lobe using the bronchoscope. With this maneuver, the oxygen saturation increased to 85-90%. Because of refractory hypoxemia, it was decided to extract the growth using RB. The procedure was performed after administration of total intravenous anesthesia using intravenous propofol 100mg and succinyl choline 50mg. RB was performed at the bedside using a ventilating tracheobronchoscope (8.5mm diameter, 43cm length, Karl Storz GmbH & Co. KG, Germany), and the tumor was extracted using rigid bronchoscopic forceps (Alligator forceps grasping with double active jaw, Karl Storz GmbH & Co. KG, Germany). The RB procedure itself took about three minutes. There was immediate improvement in oxygenation, and the patient was extubated the same day and discharged from hospital the following day. Histopathological examination revealed a well encapsulated tumor composed of lobules of mature adipose tissue without any cytological atypia, lined by respiratory epithelium with squamous metaplasia, confirming the diagnosis of endobronchial lipoma (Fig. 4).
On follow-up at one month, there was complete resolution of cough. FB revealed minimal residual lipoma in the anterior segment of the right upper lobe (Fig. 5). The patient refused any further surgical intervention for the residual tumor.
DiscussionBenign endobronchial tumors present with clinical symptoms depending on the type of tumor (for e.g. most patients with carcinoid manifest with hemoptysis), extent of endobronchial obstruction, and the degree of distal parenchymal damage due to the obstruction.6,7 Lipomas constitute 3.2-9.5% of all benign endobronchial tumors.1 Nearly three-quarters of the patients are symptomatic and almost 80% have demonstrable chest radiographic abnormalities.6 The CT findings of the presence of a lesion with an attenuation of fat (−100 HU) and absence of enhancement following contrast administration is usually diagnostic of lipoma.4 Histologically, endobronchial lipomas are described by their primary mesenchymal component as hamartomatous, fibromatous, chondromatous, lipomatous, or leiomyomatous.8 The index case fits into the lipomatous variety. Squamous metaplasia may be seen in the overlying epithelium, as in the index case.9
Historically, surgery has been performed in endobronchial lipomas due to the presence of post-obstructive changes in the parenchyma and difficulty in differentiating the lesion from a malignant tumor.6 Surgical procedures (pneumonectomy, lobectomy, bilobectomy, and resection by bronchotomy) should however, be reserved for cases with possible coexistent malignant tumor, distal irreversible parenchymal destructive changes, extra-bronchial extension or subpleural disease and expected technical difficulties during bronchoscopic resection like multidirectional tumor growth.6,10
Currently, bronchoscopic resection has been proposed as the first line of management of endobronchial lipomas as removal is both diagnostic and curative, and both flexible and rigid bronchoscopy have been used successfully.5,6 In a retrospective review of 64 endobronchial lipomas, 6 did not undergo any treatment while 41 underwent surgical resection. The remaining 17 cases were treated with flexible bronchoscopy (7 by Nd:YAG LASER, 5 by electrosurgical snaring forceps, and another 5 with a combination of LASER and electrosurgical snaring forceps).6 In a multicenter retrospective study of interventional bronchoscopic management of endobronchial lipomas, RB was performed in 94.7% (36 of 38) patients who underwent tumor removal with LASER application and mechanical debulking (76.3%).5 In the remaining 2 patients, FB and LASER was used. In 5 patients, FB procedure was followed by a RB therapeutic procedure.5 The recurrence rate of endobronchial lipoma is low, and in two large series employing interventional bronchoscopy for management of endobronchial lipoma there was no recurrence of the tumor in any patient.5,6
Several techniques can be used with the flexible bronchoscope for the removal of endobronchial tumors. The most often used technique is to excise the tumor (either piecemeal or completely in case of a pedunculated growth) using the electrocautery snare. The excised tumor can be extracted using a biopsy forceps or a Dormia basket forceps.11 The procedure can also be performed with the rigid bronchoscope using the barrel of the rigid scope to mechanically debulk the tumor and the growth can be extracted using the rigid forceps. Additional ablative techniques can be used concomitantly and include Nd:YAG laser,5 ethanol injection into the base,12 electrosurgical snaring,6 argon plasma coagulation of base,13 and cryotherapy,5 Endobronchial electrosurgery, which is relatively inexpensive and widely available has been reported to be most cost-effective and one of the easier techniques to perform.14
The choice of FB vs. RB depends on the availability, the operator's experience, the underlying pathology and anatomic location of the tumor, degree of airway compromise, and the respiratory status of the patient. Central tumors with airway compromise or endobronchial tumors with a high propensity to bleed such as carcinoids usually necessitate rigid bronchoscopic management. Our case highlights the perils associated with the use of FB. In our patient, obstruction of a unilateral left main bronchus caused life-threatening hypoxemia despite a patent right main bronchus (tumor site). This is probably due to severe ventilation-perfusion mismatch caused by acute obstruction of the normal left main bronchus while compensatory pulmonary vasoconstriction on the diseased right side persisted due to long standing endobronchial obstruction. Our report also emphasizes the advantages provided by RB over FB when removing large tumors from the airway. As the majority of the diagnostic and many therapeutic bronchoscopic procedures can be effectively performed with FB, RB training is not regularly available at most teaching institutes.15 The rigid bronchoscope however remains the most important instrument for therapeutic airway procedures and provides excellent airway control as illustrated in this case. Further, flexible bronchoscope can be introduced through the barrel of rigid bronchoscope and appears to be the preferred mode for performing such therapeutic procedures. Complete eradication of benign endobronchial tumors has been successfully achieved by performing electrosurgical snaring with a fiberoptic scope passed through the rigid bronchoscope.16 Excised tissue can be removed through the rigid bronchoscope and in cases of large tissue, along with the rigid bronchoscope.16
ConclusionsIn conclusion, based on our experience we recommend that when confronted with a large benign endobronchial tumor occluding the trachea or main-stem bronchus, physicians should initially employ rigid bronchoscopy, using flexible bronchoscopy techniques either in concert with rigid bronchoscope or later if more peripheral treatment is required.
Conflicts of interestThe authors have no conflicts of interest to declare.