Sarcoidosis is a multisystemic disorder of unknown etiology. Its diagnosis is based on compatible clinical and radiological features and supported by histological demonstration of epithelioid cell noncaseating granulomas with exclusion of other causes. Endobronchial ultrasound combined with transbronchial needle aspiration (EBUS-TBNA) has been proposed as a valuable tool in obtaining suitable tissue sample.
The aim of this study was to evaluate the contribution of EBUS-TBNA to the diagnosis of stages I and II thoracic sarcoidosis in a community-based hospital.
MethodsA prospective study was conducted in patients with suspected stages I and II pulmonary sarcoidosis, based on clinical and radiological data, who were being followed in our Interstitial Lung Disorders Outpatient Clinic or sent from other hospitals to our Respiratory Endoscopy Unit for diagnostic procedures. All suitable and fit patients underwent EBUS-TBNA between March 2010 and June 2013.
We assessed demographic characteristics, radiological stages, cytological/histological examination and diagnostic techniques performed.
ResultsIn the period considered 39 patients underwent EBUS-TBNA for suspected stages I and II thoracic sarcoidosis and adequate samples were obtained in 38 (97.4%). Within this population, 33 (84.6%) patients had a definite diagnosis of sarcoidosis, of which 31 patients (93.9%) were confirmed to have epithelioid noncaseating granulomas by EBUS-TBNA. Four patients were submitted to surgical procedures (three to mediastinoscopy and one to open surgical lung biopsy).
Data analysis allowed to calculate a sensitivity, specificity, positive predictive value, negative predictive value and diagnostic accuracy of 93.9%, 100%, 100%, 75.0% and 94.8%, respectively. No complications were observed.
ConclusionsEBUS-TBNA is a valuable tool in the diagnostic workup of patients with suspected stages I and II thoracic sarcoidosis providing a substantial number of pathological confirmations and with few complications. Its high diagnostic accuracy precludes the need for more invasive procedures such as surgical biopsy.
A Sarcoidose é uma doença multissistémica de etiologia desconhecida. O seu diagnóstico baseia-se em características clínicas e radiológicas compatíveis e é apoiado pela demonstração histológica de granulomas epitelióides não caseosos, com a exclusão de outras causas. A ecoendoscopia brônquica combinada com a punção aspirativa transbrônquica (EBUS-TBNA) foi proposta como uma ferramenta valiosa na obtenção de amostras de tecido adequadas.
O objectivo deste estudo foi avaliar o contributo da EBUS-TBNA para o diagnóstico de sarcoidose torácica de estádio I e II num hospital central.
MetodologiaFoi realizado um estudo prospectivo em doentes com suspeita de sarcoidose torácica de estádio I e II, com base em dados clínicos e radiológicos, que estavam a ser seguidos na nossa Clínica Ambulatória de Doenças Pulmonares Intersticiais, ou foram enviados de outros hospitais para a nossa Unidade de Endoscopia Respiratória, para os procedimentos de diagnóstico. Todos os doentes adequados e aptos foram submetidos a EBUS-TBNA, entre Março de 2010 e Junho de 2013.
Avaliámos as características demográficas, os estádios radiológicos, exames citológicos/histológicos e técnicas de diagnóstico usados.
ResultadosNo período referido anteriormente, 39 doentes foram submetidos a EBUS-TBNA para a suspeita de sarcoidose torácica de estádio I e II, e foram obtidas amostras adequadas em 38 deles (97,4%). Nesta população, 33 (84,6%) doentes receberam um diagnóstico definitivo de sarcoidose, dos quais 31 doentes (93,9%) foram confirmados como tendo granulomas epitelioides não caseosos, pela EBUS-TBNA. Quatro doentes foram submetidos a procedimentos cirúrgicos (três a mediastinoscopia e outro a biopsia pulmonar cirúrgica aberta).
A análise dos dados permitiu calcular uma sensibilidade, especificidade, valor preditivo positivo, valor preditivo negativo e acuidade diagnóstica de 93,9%, 100%, 100%, 75,0% e 94,8%, respectivamente. Não foram observadas complicações.
ConclusõesA EBUS-TBNA é uma ferramenta valiosa na abordagem diagnóstica dos doentes com suspeita de sarcoidose torácica de estádio I e II, proporcionando um número importante de confirmações patológicas e com poucas complicações. A sua elevada acuidade diagnóstica exclui a necessidade de procedimentos mais invasivos como uma biópsia cirúrgica.
Sarcoidosis is a multisystemic disorder of unknown cause. It commonly affects young and middle-aged adults and frequently presents with bilateral hilar lymphadenopathy, pulmonary infiltrates, ocular and skin lesions, but virtually all organs may be involved. The course and prognosis were found to correlate with the clinical onset and the extent of the disease. An acute onset with erythema nodosum or asymptomatic bilateral hilar lymphadenopathy usually heralds a self-limiting course whereas an insidious onset, especially with multiple extra-pulmonary manifestations, may be followed by relentless progressive fibrosis of the lungs and other organs.1 The heterogeneity in prevalence, disease presentation and severity is significant among different ethnic and racial groups and in various countries. The prevalence ranges from less than one case to 40 cases per 100,000.2
The diagnosis of sarcoidosis is based on a compatible clinical and radiological picture, histological evidence of noncaseating granulomas and exclusion of other diseases capable of producing a similar histological or clinical picture.3,4
The development of endobronchial ultrasound (EBUS), which enables real-time visualization of mediastinal and hilar structures combined with transbronchial needle aspiration (EBUS-TBNA), currently allows safe and effective functioning of mediastinal and hilar lymph nodes. EBUS-TBNA is widely recognized as being very useful in the diagnosis and staging of lung cancer. However, its importance in the diagnosis of benign pathology of the chest, including sarcoidosis, is progressively increasing.
Pathological confirmation has been most commonly achieved by flexible bronchoscopy with standard bronchoscopic techniques (transbronchial lung biopsy and bronchial biopsy), which has a yield of approximately 53–70% in patients with pulmonary sarcoidosis.5,6 EBUS-TBNA is gaining momentum as an important new technique for the diagnosis of enlarged lymph nodes due to sarcoidosis. Recent data from randomized trials have demonstrated its superiority to conventional TBNA with a 19-G needle7 and bronchial and transbronchial biopsies6 for the diagnosis of pulmonary sarcoidosis.
The Granuloma Trial presented a diagnostic yield for detection of granulomas of 80% with EBUS-TBNA in patients with suspected sarcoidosis.6
In a recent editorial, Culver and Costabel stated that although there is consolidated evidence of the advantages of EBUS-TBNA over other techniques, a most appropriate way to study the usefulness of EBUS-TBNA would be to evaluate consecutive subjects for whom sarcoidosis is in the diferential diagnosis, this would mirror the population that physicians encounter in their regular practice.8
Materials and methodsA prospective study was conducted in patients with suspected stages I and II pulmonary sarcoidosis based on clinical and radiological data followed in our Interstitial Lung Disorders Outpatient Clinic or sent from other hospitals to our Respiratory Endoscopy Unit for diagnostic procedures. All patients with clinical and radiological suspicion of stages I and II pulmonary sarcoidosis underwent EBUS-TBNA for diagnostic purposes in our hospital between March 2010 and June 2013. Exclusion criteria were: obvious organ involvement of sarcoidosis where there was the possibility of confirming the diagnosis with a minimally invasive diagnostic procedure, Löfgren syndrome and inability to undergo or consent to the procedure.
We assessed demographic characteristics, chest radiography stages, nodal stations punctured, cytological and/or histological examination, other diagnostic techniques [bronchoalveolar lavage (BAL), bronchial biopsy, transbronchial lung biopsy (TBLB) or biopsies from other sites] and follow-up including the need for surgical biopsy (mediastinoscopy/video-assisted thoracic surgery (VATS)/thoracotomy).
Other exams were performed concurrently according to, clinical decisions related to ROSE results, endoscopic findings and technical and anesthetic limitations.
BAL was performed when technically possible and if not performed previously and if available from the processing external laboratory.
Sarcoidosis was diagnosed based upon a compatible clinical and radiological picture and where epithelioid noncaseating granulomas could be demonstrated with exclusion of other known causes.4
EBUS-TBNA was performed under general anesthesia through a rigid scope (KARL STORZ GmbH & Co. KG, Tuttlingen, Germany) using a dedicated bronchoscope equipped with a distal 7.5-MHz curved linear ultrasound transducer probe (BF-UC180F, Olympus Ltd, Tokyo, Japan) and ultrasound image processor (EU-ME1; Olympus Ltd, Tokyo, Japan). A 22-G cytology needle (MA-201SX4022, Olympus Ltd, Tokyo, Japan) was used to obtain specimens.
Cytological samples were prepared, stained (hematoxylin/eosin) and evaluated on site whenever a pathologist was available – rapid on site evaluation (ROSE). When ROSE was not possible a minimum of 4 nodal aspirates was obtained.
Blood clot cores obtained from the EBUS-TBNA aspirates were sent in formalin for histological examination.
Samples were also sent for mycobacteriological tests given the intermediate incidence of tuberculosis in Portugal.
Cytological samples were considered adequate when the sample contained at least 40 benign-appearing lymphocytes in a high-power field in the areas of highest cellularity of the smear, there was identification of large numbers of anthracotic pigment and macrophages or large clusters of admixed lymphocytes and pigmented macrophages or malignancy or granulomatous disease was seen with small numbers of lymphocytes, as commonly accepted.9 Histological samples were considered representative when nodal tissue, granulomas or other pathological finding was observed.
Follow up data was obtained for all patients including clinical and radiological evolution and subsequent exams performed.
Descriptive statistical measures of the studied variables included mean and standard deviation for continuous variables, and absolute frequency and percentage for each category of a categorical variable. Diagnostic sensitivity, specificity, positive predictive value, negative predictive value and accuracy for EBUS-TBNA were calculated.
This study has been approved by our hospital's Ethics Committee.
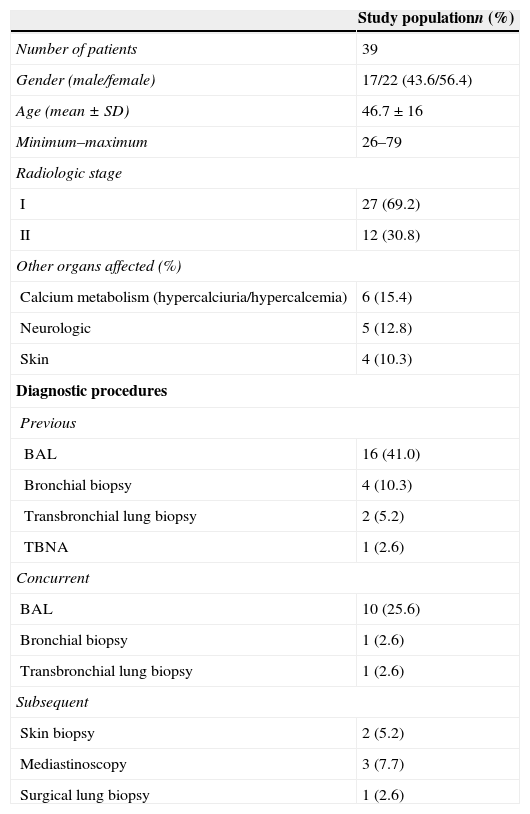
ResultsDuring the study period 39 patients underwent EBUS-TBNA for suspected pulmonary sarcoidosis and its characteristics are described in Table 1.
Population characteristics.
| Study populationn (%) | |
|---|---|
| Number of patients | 39 |
| Gender (male/female) | 17/22 (43.6/56.4) |
| Age (mean±SD) | 46.7±16 |
| Minimum–maximum | 26–79 |
| Radiologic stage | |
| I | 27 (69.2) |
| II | 12 (30.8) |
| Other organs affected (%) | |
| Calcium metabolism (hypercalciuria/hypercalcemia) | 6 (15.4) |
| Neurologic | 5 (12.8) |
| Skin | 4 (10.3) |
| Diagnostic procedures | |
| Previous | |
| BAL | 16 (41.0) |
| Bronchial biopsy | 4 (10.3) |
| Transbronchial lung biopsy | 2 (5.2) |
| TBNA | 1 (2.6) |
| Concurrent | |
| BAL | 10 (25.6) |
| Bronchial biopsy | 1 (2.6) |
| Transbronchial lung biopsy | 1 (2.6) |
| Subsequent | |
| Skin biopsy | 2 (5.2) |
| Mediastinoscopy | 3 (7.7) |
| Surgical lung biopsy | 1 (2.6) |
The majority of patients were female (22/56.4%) with an average age of 46.7±16 years. Suspected radiological stage I pulmonary sarcoidosis was most frequently observed (27/69.2%).
The most common extrapulmonary manifestations were abnormalities in calcium metabolism – hypercalciuria and/or hypercalcemia (6/15.4%), neurological (5/12.8%) and skin (4/10.3%) involvement. Skin involvement was not apparent at diagnosis in 3 patients and was not typical in one patient leading to biopsy for differential diagnosis in 2 of these patients. Biopsies were performed after diagnosis and dermatologist evaluation.
Sixteen patients performed previous nondiagnostic flexible bronchoscopy with BAL (16), bronchial biopsy (4), transbronchial lung biopsy (2) or TBNA (1). Additionally ten patients perfomed BAL at the same time as EBUS-TBNA and one patient performed both bronchial and transbronchial lung biopsy concurrently. (Table 1)
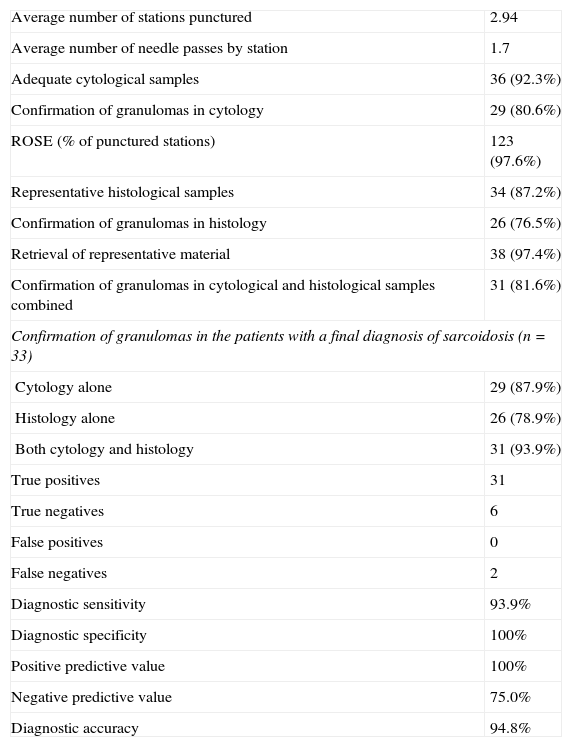
Concerning EBUS-TBNA, an average of 2.94 stations were punctured, most frequently 7, 4R, 11R, 11L and 4L, with an average size of 18.9±6.9mm and an average 1.7 needle passes per station (Table 2). Rapid on-site examination (ROSE) was performed in 123 (97.6%) of cytological samples.
Cytological and histological results and diagnostic accuracy of EBUS-TBNA.
| Average number of stations punctured | 2.94 |
| Average number of needle passes by station | 1.7 |
| Adequate cytological samples | 36 (92.3%) |
| Confirmation of granulomas in cytology | 29 (80.6%) |
| ROSE (% of punctured stations) | 123 (97.6%) |
| Representative histological samples | 34 (87.2%) |
| Confirmation of granulomas in histology | 26 (76.5%) |
| Retrieval of representative material | 38 (97.4%) |
| Confirmation of granulomas in cytological and histological samples combined | 31 (81.6%) |
| Confirmation of granulomas in the patients with a final diagnosis of sarcoidosis (n=33) | |
| Cytology alone | 29 (87.9%) |
| Histology alone | 26 (78.9%) |
| Both cytology and histology | 31 (93.9%) |
| True positives | 31 |
| True negatives | 6 |
| False positives | 0 |
| False negatives | 2 |
| Diagnostic sensitivity | 93.9% |
| Diagnostic specificity | 100% |
| Positive predictive value | 100% |
| Negative predictive value | 75.0% |
| Diagnostic accuracy | 94.8% |
With EBUS-TBNA it was possible to obtain adequate cytological samples in 36 patients (92.3%), histological adequate samples in 34 patients (87.2%) and in 38 patients (97.4%) combining both. There was evidence of epithelioid noncaseating granulomas in 29 (80.6%) of patients in cytological examination, 26 (76.5%) in histological examination and 31 (81.6%) combining cytological and histological examinations (Table 2).
There were no observed procedural complications.
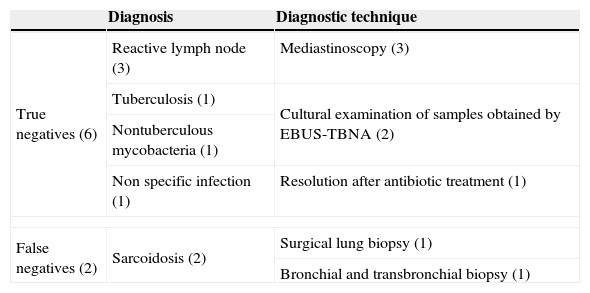
Out of the eight patients with suspected sarcoidosis that did not show presence of granulomas on EBUS-TBNA, two patients had confirmation of non-caseating epitheloid cell granulomas with other exams – one patient presented on both bronchial and transbronchial lung biopsies and one patient underwent an open lung biopsy revealing non-caseating epitheloid cell granulomas (Table 3). Both of these patients were stage II sarcoidosis.
Nondiagnostic EBUS-TBNA results.
| Diagnosis | Diagnostic technique | |
|---|---|---|
| True negatives (6) | Reactive lymph node (3) | Mediastinoscopy (3) |
| Tuberculosis (1) | Cultural examination of samples obtained by EBUS-TBNA (2) | |
| Nontuberculous mycobacteria (1) | ||
| Non specific infection (1) | Resolution after antibiotic treatment (1) | |
| False negatives (2) | Sarcoidosis (2) | Surgical lung biopsy (1) |
| Bronchial and transbronchial biopsy (1) | ||
Out of the remaining six patients, three patients underwent mediastinoscopy (all with histology compatible with reactive lymph node in all stations) and three patients did not perform additional investigation as other diagnoses were confirmed (tuberculosis, nontuberculous mycobacteria) or clinical resolution was obtained with treatment for infection (Table 3). All the patients had clinical/radiological suspicion of stage I sarcoidosis.
This represents a calculation of true positives, true negatives, false positives and false negatives of 33, 6, 0 and 2 respectively.
Data analysis allowed to calculate, for EBUS-TBNA, a sensitivity, specificity, positive predictive value, negative predictive value and diagnostic accuracy of 93.9%, 100%, 100%, 75.0% and 94.8%, respectively.
DiscussionEBUS-TBNA is a valuable tool in the diagnostic algorithm of mediastinal and hilar lymphadenopathy. In patients with clinical and radiological features compatible with stages I and II sarcoidosis, EBUS-TBNA can confirm the diagnosis by demonstrating noncaseating granulomas and exclusion of other pathologies. Combining it with other endoscopic techniques can improve the sensitivity and specificity and avoid the need for more invasive diagnostic procedures.
A major advantage of EBUS-TBNA is that it can be done at the same time as other endoscopic techniques such as bronchoalveolar lavage or biopsy, reducing the number of procedures and anesthetic complications.
Rapid on site evaluation (ROSE) in the vast majority of cytological samples enabled us to have diagnosis on site, reducing the number of stations punctured when diagnosis was obtained or pursuing until adequate samples were retrieved. In this study we found that adequate samples were obtained in 38 out of 39 patients (97.4%).
Other studies have demonstrated the advantages of using EBUS-TBNA in patients with suspected sarcoidosis. Navani et al. described that in patients with sarcoidosis, the sensitivity of EBUS-TBNA for detection of noncaseating granulomas was 85%, compared with a sensitivity of 35% for standard bronchoscopic techniques [flexible bronchoscopy with transbronchial lung biopsy (TBLB) without fluoroscopy guidance, broncho-alveolar lavage and bronchial biopsy if endoscopic findings] (P<0.001).10
Wong et al. performed a study in 65 patients and concluded that in patients with a final diagnosis of sarcoidosis, EBUS-TBNA demonstrated noncaseating epithelioid cell granulomas in 56 (91.8%) of the patients without reported complications.7 In our study, of all the patients that had a definite diagnosis of sarcoidosis and performed EBUS-TBNA (33 patients), noncaseating granulomas were found on 31 patients.
Results from the Granuloma Trial have been published concluding that among patients with suspected stage I/II thoracic sarcoidosis undergoing tissue confirmation, the use of endosonographic nodal aspiration compared with bronchoscopic biopsy resulted in greater diagnostic yield.6
Recent studies suggest that blood clot cores obtained with EBUS-TBNA contain diagnostic material and should be sent for histopathological examination, as there is the potential to spare up to 10% of patients more invasive diagnostic biopsy procedures.11
We observed a high concordance between cytological smear and blood clot histopathological analysis with 24 patients (72.7%) demonstrating granulomas on both. Also the histopathological blood clot evaluation allowed for the diagnosis in 2 patients with no granuloma on the cytological specimen improving diagnostic capacity by 6.5%. Although this was not an end point of our study, we found that histological examination of the blood clots cores raised the diagnostic accuracy of the exam.
ConclusionsOur study shows that in selected patients with clinical and radiological features compatible with stages I and II sarcoidosis, EBUS-TBNA is a valuable asset for obtaining adequate tissue sample and confirming the diagnosis.
The high diagnostic accuracy of EBUS-TBNA prevents the need for more invasive procedures such as surgical biopsy. The results obtained suggest that, if available, EBUS-TBNA should be considered as a first line examination in the work up of hilar and mediastinal lymphadenopathy when stages I or II sarcoidosis is suspected.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
The Respiratory Endoscopy Unit would like to thank the Pathology Department (Head of Department – António Couceiro) namely doctors Agostinho Sanches, Antónia Furtado, David Tente and technician Sónia Veludo for their cooperation in ROSE during EBUS-TBNA.