Pulmonary aspergilloma is the most common presentation, in our Pulmonology department, of pulmonary involvement of aspergillosis and is usually seen as a fungus ball that colonizes and grows into a pre-existing lung cavity, in the majority of cases secondary to pulmonary tuberculosis (PT). Other forms of pulmonary aspergilosis are allergic bronchopulmonary aspergillosis, chronic necrotizing aspergillosis,1 invasive aspergillosis and some authors even describe a semi-invasive form of aspergillosis.2 The diagnosis of pulmonary aspergilloma is usually easy on a plain-film imaging or by computed tomography of the chest. But an endobronchial aspergilloma (EBA) is a rare disease, and another, but unusual, presentation of aspergillosis,3 characterized by the growth of Aspergillus species into the bronchial lumen. These two different presentations of aspergillosis can co-exist in the same patient. The endobronchial aspergilloma is a non invasive form of aspergillosis, and in many cases incidentally diagnosed, in a patient who had undergone a bronchoscopy to investigate haemoptysis, or for another reason.
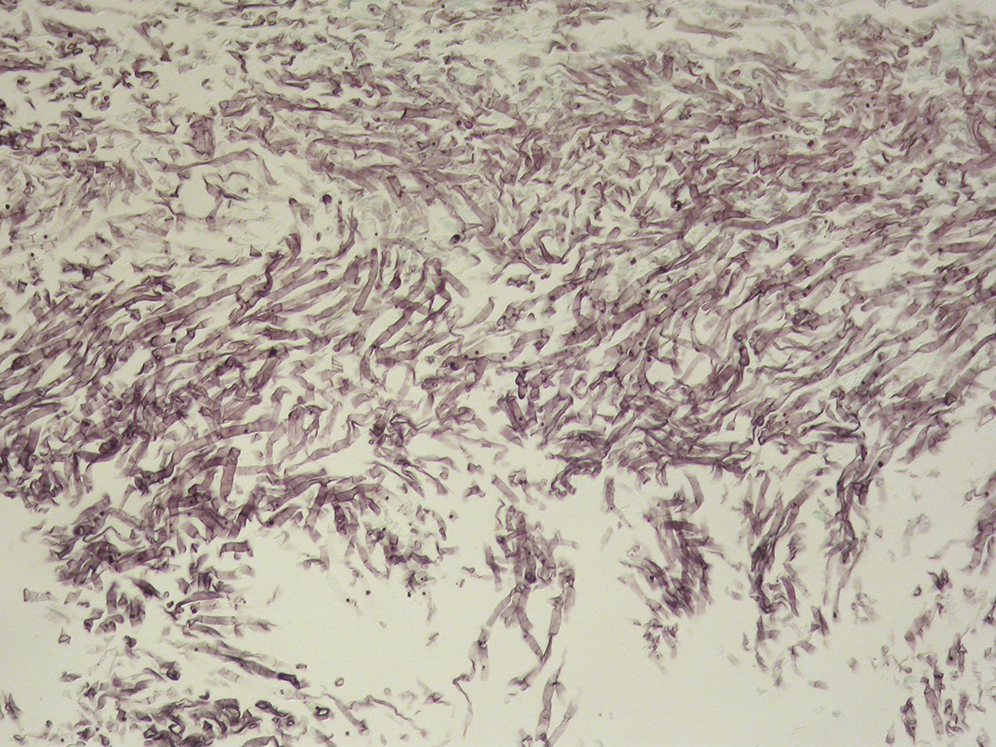
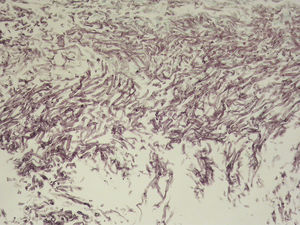
A 64-year-old male outpatient was referred for bonchoscopy because of CT findings of cavitary lesion with a suggestive image of a fungus ball, in the lingular division of the left upper lobe (LUL), at that time without respiratory complaints. He had a background of congestive heart failure, rheumatoid arthritis treated with methotrexate and high-dose of prednisolone, and a diagnosis of pulmonary tuberculosis 6 months before, still under treatment, with a cavitary lesion in the lingular division. When diagnostic video-bronchoscopy was perfomed, we found a large yellowish hard mass (Figure 1) with almost complete obstruction of the lower segment of the lingular division of the LUL, and Aspergillus was confirmed by histological examination: small plugs constituted by fungal structures of Aspergillus species after dyeing with PAS and Grocott (Figure 2). At the time of diagnosis, the patient, who was immunocompromised, was on treatment for PT, and began treatment with voriconazole, but he died a few months later, from congestive heart failure.
Figure 1. Video-bronchoscopy showing a yellowish mass in the lingular division of the LUL.
Figure 2. Histological examination showing small plugs constituted by fungal structures of Aspergillus species.
The endobronchial aspergilloma is a rare entity and was first described by Denning et al. in three patients with AIDS,4 and is usually incidentally detected as a necrotic mass causing bronchial obstruction. It is easily diagnosed by histopathologic examination of the endoscopic biopsies, and should be considered in the differential diagnosis of an endobronchial necrotic lesion,5 in some cases mimicking endobronchial lung cancer. In other cases, superimposed aspergillosis can mask a lung cancer or an endobronchial carcinoid6 and it can be hard to differentiate true EBA with colonization of Aspergillus of an underlying cancer.7 There are also descriptions of endobronchial aspergilloma associated with a foreign body8 or causing a bronchomediastinal fistula.9 An EBA can occur in immunocompetent patients, with or without underlying lung disease, and because the optimal treatment or duration of therapy has not yet been established, the EBA requires close medical watch. In our case we describe two forms of aspergilloma in the same patient, an EBA and a pulmonary aspergilloma, and in the course of a treatment for PT. This case is more than just a bronchoscopic curiosity, as it helps us to understand the wide variety of pulmonary aspergillosis.
Conflicts of interestThe authors have no conflicts of interest to declare.
Corresponding author. duartearaujodr@sapo.pt