To the Editor,
Respiratory bronchiolitis-associated interstitial lung disease (RB-ILD) is a rare interstitial pneumonia that usually affects current smokers in the fourth and fifth decades of life with a history of heavy smoking (usually more than 30 pack-years).1, 2 In most cases the symptoms of RB-ILD are subclinical and detected coincidentally or it is associated with a mild clinical presentation, usually a gradual onset of dyspnea and/or a presence of persistent cough.1, 2 Lung function tests reveal only minor restrictive or obstructive defects in most cases, often combined with hyperinflation. Additionally, carbon monoxide diffusing capacity (DLCO) is often slightly to moderately impaired.2, 3 High Resolution Chest CT-scan (HRCT) classic features are essentially ground glass centrilobular nodules located in the upper lobes which in the appropriate clinical context are normally not difficult to differentiate from other interstitial lung diseases (ILD).2, 4 Bronchoalveolar Lavage (BAL), may help in the differential diagnosis with other ILD and it is characterized by a raised total cell count induced by an increased number of intense brown pigment-laden macrophages, although a mild neutrophilia may also be present.2, 5 The evolution is unpredictable and heterogeneous regardless of smoking cessation and more data are required in order to be precise about the outcome of this disease due the conflicting data published so far.1, 2, 5
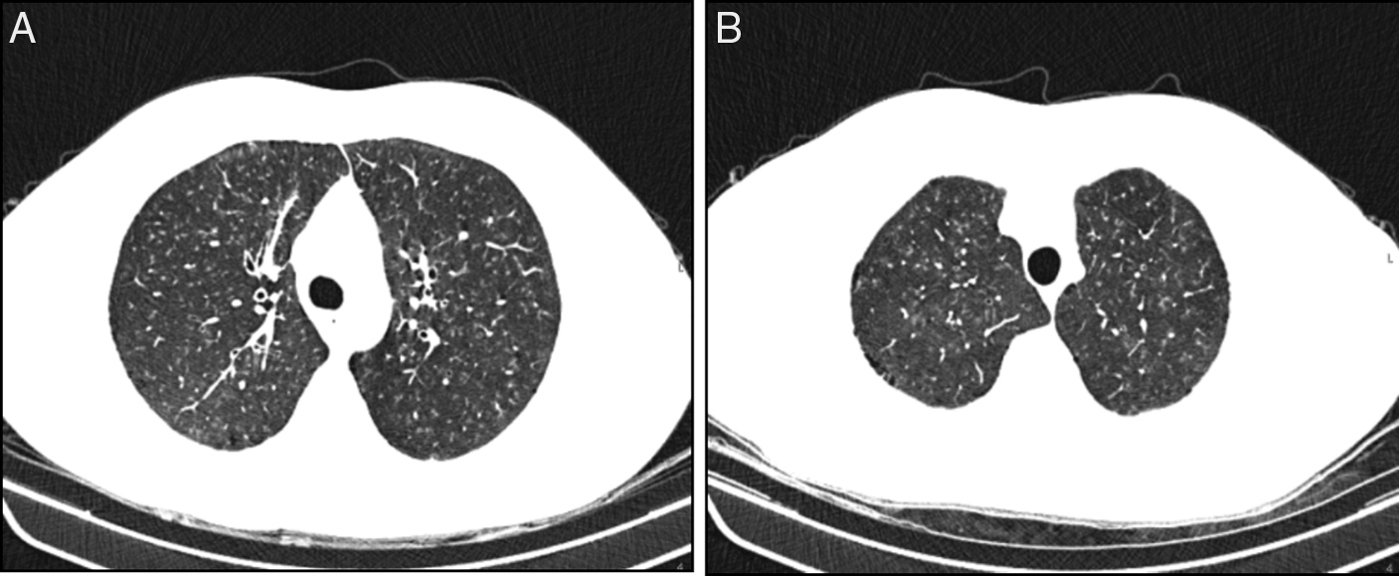
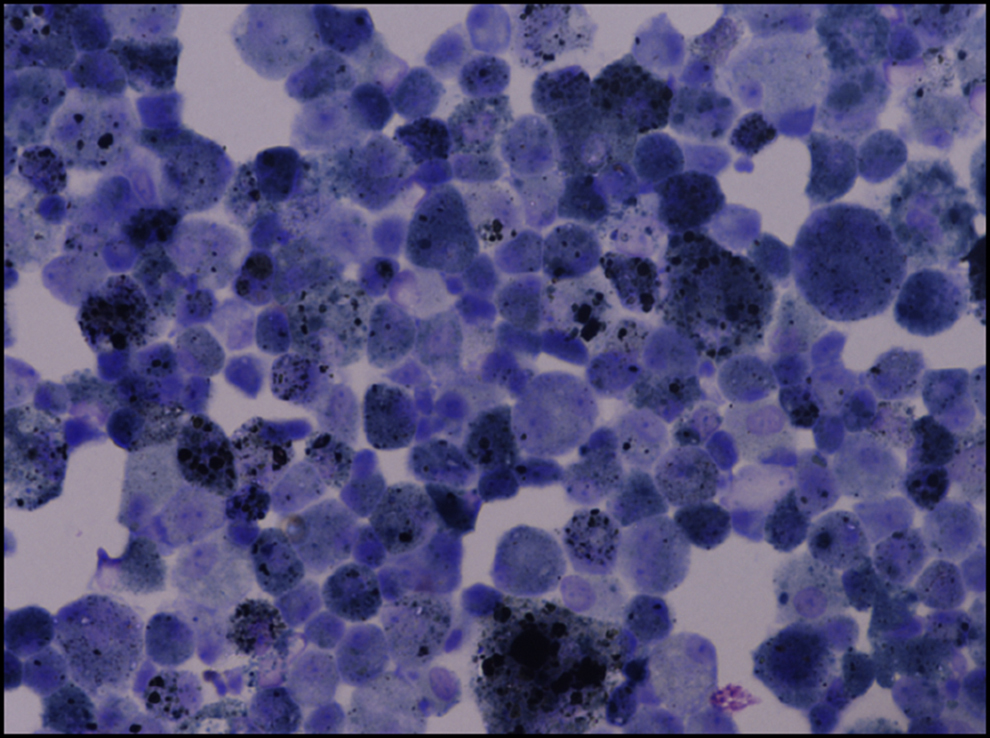
The medical records of patients diagnosed with RB-ILD during the period of January 2008 to July 2013, followed in ILD outpatient clinic at Centro Hospitalar S. João, were retrospectively reviewed. RB-ILD diagnosis was based on 2002 American Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias.6 Fifteen patients were included with a mean age of 48 (29–65) years and 13 (86.6%) were male. All of them were heavy cigarette smokers (median: 46.3 pack-year). Most patients (73.4%) have mild symptoms, dyspnea on exertion (n = 8/53.3%) and cough (n = 7/46.6%) were the only symptoms identified. Typical centrilobular ground-glass nodules predominantly in the upper lobes were the overall pattern on the HRCT (Figure 1). Concomitant upper lobe centrilobular emphysema was identified in 5 (33.3%) patients. Pulmonary function tests showed a slight obstructive impairment (median FEV1 – 76%) associated with a normal median value in the diffusion capacity (median DLCO – 76%), although there was a minor decrease (DLCO – 61–75%) in six patients. BAL was performed in 12 patients and besides the increased cellularity associated with the intense brown pigment-laden macrophages (Figure 2), two (16.6%) had mild neutrophilia and another two mild eosinophilia. Three patients were submitted to surgical lung biopsy, two of them performed during the context of cardiothoracic surgeries not related with RB-ILD and the other one during a video-assisted thoracoscopic surgery for pneumothorax with a persistent air-leak. All patients were referred to smoking cessation programs but only three gave up, the remainder just reduced the amount of tobacco consumption. None of them had any additional therapeutic interventions besides inhaled bronchodilators prescribed to those patients that were more symptomatic. Regardless of whether they maintained smoking habits, after a mean follow-up of 49 (12–72) months, all the patients included remained clinically stable, with similar functional (mean FEV1 – 74% and DLCO – 75%) and radiological features.
Figure 1. Axial CT images show ill-defined centrilobular ground glass nodules with predominant upper lobe distribution. Areas of paraseptal emphysema are present.
Figure 2. BAL from a patient with RB-ILD with an increased number of intense brown pigment-laden macrophages.
This group of RB-ILD patients had the usual characteristic clinical presentation described previously in other series. Additionally, they showed a favorable clinical course, even those who continued to smoke, which confirms a good prognosis associated with this disease.
Conflict of interestThe authors declare no conflict of interest.
Corresponding author. manuelsvaz@gmail.com