Management of pediatric primary spontaneous pneumothorax (PSP) is based on adult literature and the best therapeutic algorithm for PSP is still debatable.1 The aim of this work was to review the approach to pediatric PSP in a tertiary care hospital.
Clinical charts of patients admitted with first episode of PSP at Hospital São João (Porto, Portugal) between January 2006 and January 2012 were reviewed and analyzed for demographic, diagnosis, treatment and follow-up.
The management of PSP followed the institution protocol: small (<20%) pneumothoraxes are treated with high output oxygen therapy; moderate to large pneumothoraxes (>20–25%) are treated with chest tube drainage or needle aspiration. Surgical indications are: second ipsilateral pneumothorax; first contralateral pneumothorax; bilateral pneumothorax or persistent air leakage (>4 days). All patients proposed for elective surgery had a computerized tomography scan (CT).
Twenty-five patients with a first episode of PSP were included, with a male predominance (80%) as described in the literature. Chest pain was the most frequent presentation (>80%) followed by dyspnea and cough. Five patients had asthma, three were active smokers and one had a family history of PSP. With a follow-up range from one to six years, there were seven recurrences.
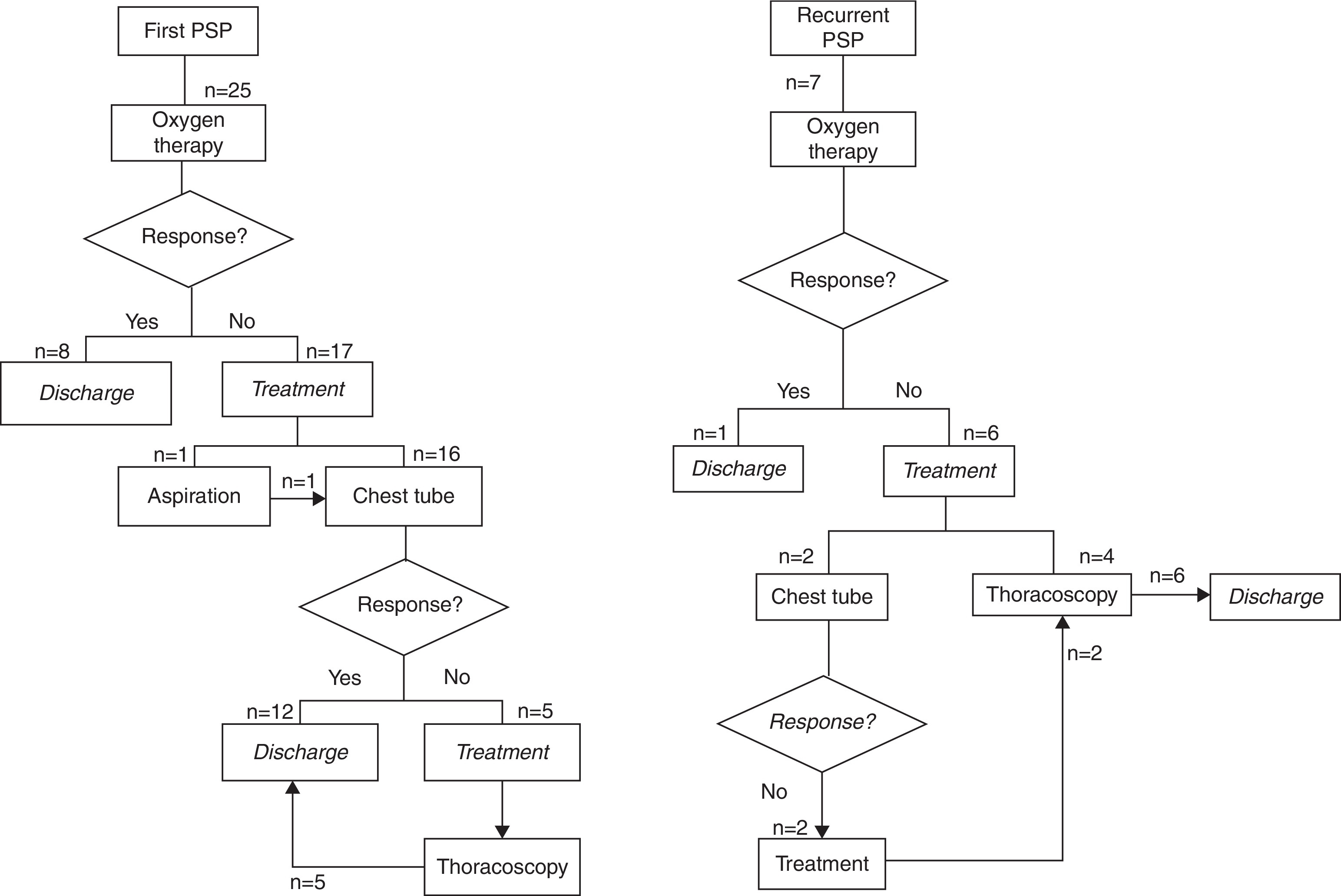
The results of the therapeutic algorithm are summarized in Figure 1. Eight of the initial episodes and 1 recurrence were successfully treated with oxygen therapy; success rate was 43% for first episodes. Chest tube was the next step and was used in 12 initial episodes with a success rate of 75%; however, chest tubes failed in all recurrent episodes. A total of 11 patients underwent thoracoscopy: 5 during the first episode and 6 during recurrence. Thoracoscopy proved to be successful in all cases, with no recurrences. In the presence of blebs, mechanical pleurodesis with bleb resection was performed, whereas in absence of blebs a mechanical pleurodesis was performed.
Figure 1. Therapeutic algorithm in the first and recurrent episodes of primary spontaneous pneumothorax.
The overall length of stay was longer for patients treated with thoracoscopy compared to patients treated with oxygen therapy or chest tube (respectively 13.4 ± 4.3, 3.8 ± 1.2, 6.2 ± 3 days, p < 0.001). However, patients were hospitalized with a mean of 8 days before surgery and if this is taken into account, there is no significant difference between treatments.
In case of oxygen therapy failure, symptomatic or large PSP, American College of Chest Physicians favors chest tube, while British Thoracic Society (BTS) prefers needle aspiration; both have similar efficiency and recurrence rates.2, 3 Robinson et al. have recently reported the implementation of the BTS guidelines in Australia and New Zealand with a large multicenter series, addressing the efficacy of needle aspiration. Although they do not separate the recurrent from the initial episodes of PSP, they report an identical success rate (46%) for expectant treatment independently of oxygen use. As in our study, when intervention was needed, chest tube was still the first-line (used in 79%); needle aspiration was used in only 21% of patients, with a success rate of 52%.4 In recurrent episodes, the efficiency falls after non-operative treatment, with described success rates as low as 52% in the second episode and 15% in the third.5 Thoracoscopy may be more aggressive, but it has the lowest reported recurrence rate (5–75%); in our study, thoracoscopy was always successful and there were no recurrences.4, 6, 7 In adult population, thoracoscopic surgery is being proposed as an alternative to chest tube even in first episodes, with lower recurrence rate and shorter hospital stay. However, randomized studies in pediatric population still advocate conservative management for initial PSP episodes, since several patients will never need surgical intervention.6, 7
Finally, the presence of blebs in the CT scan has been suggested as an independent risk factor for recurrence, but its usefulness remains controversial. Some studies indicate that blebs may not predict recurrence and CT scan findings should not be used as a basis for prophylactic surgery.1, 6, 8 In our study, more than a half of the patients had no blebs in the CT scan (58%) but blebs were associated with higher recurrence rate (63% versus 18%, p = 0.048).
The best treatment for first PSP in pediatrics is probably conservative (oxygen therapy, needle aspiration or chest tube drainage). Nevertheless, thoracoscopy is efficient and seems to be the best option in refractory or recurrent PSP.
Conflicts of interestThe authors have no conflicts of interest to declare.
Corresponding author. rubenlms@hotmail.com