Dear Editor,
Lung cancer is the most common cancer worldwide, and the leading cause of cancer-related death.1 It is considered a disease of the elderly, and octogenarians represent a rapidly growing population of patients diagnosed with this disease.2 Despite this, the evidence-based standard of care for these patients is limited. Therefore, the clinical practice in this population often poses challenges to clinicians.
The authors report the incidence, clinical characteristics, treatment and prognosis of non-small cell lung cancer (NSCLC) in octogenarian patients (80 years and over), in a tertiary academic hospital in Oporto, Portugal. We retrospectively evaluated 1292 patients newly diagnosed with lung cancer, from January 2009 to December 2014. For the purpose of analysis, only patients with NSCLC that had a follow-up in our center were included.
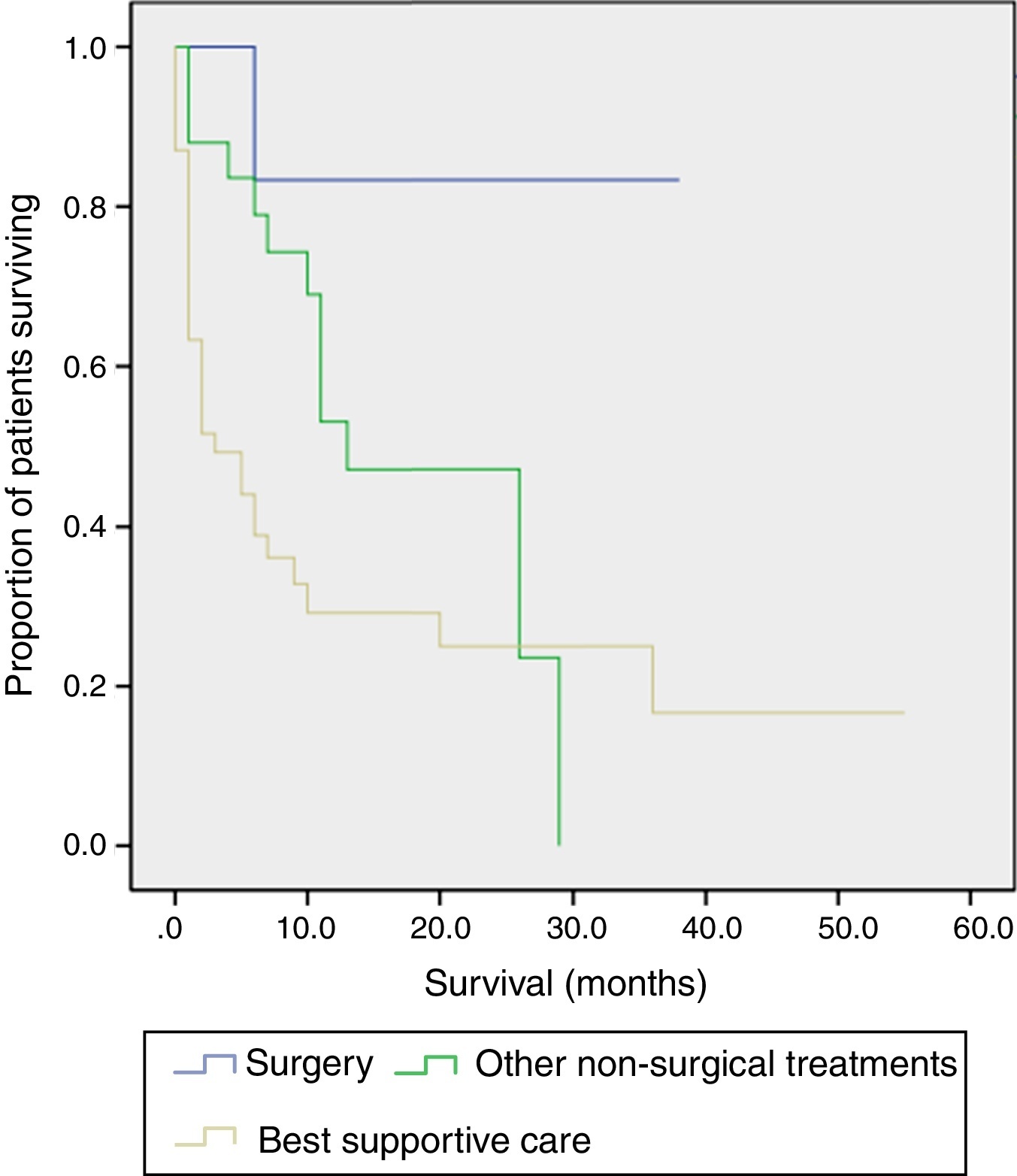
Ninety-two octogenarians were included (7.1% of total), 79.3% (n = 73) were male with a median age of 82.0 years (80–90). Smoking history was present in 65% (n = 58) of patients. The median time from symptom onset to diagnosis was 2.0 months (0–12.0). The diagnosis was obtained by bronchoscopy in 45.7% (n = 42) of patients, transthoracic biopsy guided by CT in 46.7% (n = 43) and blind pleural biopsy in 7.6% (n = 7). Adenocarcinoma was the most common histopathological type, recorded in 51.1% (n = 47) of patients, followed by squamous cell carcinoma in 41.3% (n = 38). Clinical staging revealed 23.8% (n = 22) of patients with stage I and II, 8.7% (n = 8) with III-A and 67.4% (n = 62) with III-B and IV. The initial Performance Status (PS) was 0 and 1 in 60.9% (n = 56) of patients, 2 in 16.3% (n = 15) and 3 and 4 in 22.8% (n = 21). After careful consideration, the following treatments were performed: surgery in 5.4% (n = 5), surgery followed by adjuvant chemotherapy in 1.1% (n = 1), chemotherapy only in 17.4% (n = 16), chemotherapy plus conventional radiotherapy in 8.7% (n = 8), conventional radiotherapy in 5.4% (n = 5) and stereotactic body radiation therapy (SBRT) in 2.2% (n = 2). Most patients (58.7%, n = 54) were submitted to best supportive care (BSC), two-thirds presenting PS ≥ 2. Platinum-based doublet regimens were used in one-third of patients submitted to chemotherapy. Surgery was performed on 6 patients: lobectomy and mediastinal lymph node dissection in 3, lobectomy without mediastinal lymph node dissection in 1, segmentectomy in 1 and atypical lung resection in 1. Using Charlson Comorbidity Index, all patients scored high, even the potential surgical candidates, reducing the number of surgeries performed. One postoperative death was the major complication encountered. During the follow-up period, 38% (n = 35) of octogenarians are still alive, 53.5% (n = 49) died and 8.7% (n = 8) were lost to follow-up. In Kaplan–Meier analyses, the median survival rate was about 2.5 months in the BSC group and 12.5 months for those submitted to other non-surgical treatments. More than 80.0% of patients who had surgery are still alive (Figure 1).
Figure 1. Kaplan–Meier survival curves according to treatment performed (surgery, other non-surgical treatments and best supportive care).
With social and medical evolutions, and consequently global aging, it is expected that more elderly will be affected by lung cancer. For clinicians, it will be increasingly a challenge to manage these patients because they usually have a high burden of comorbidities, a high risk of complications and shorter life expectancy.3, 4 Thus, some clinicians are reluctant to propose anticancer treatments (including surgery) to octogenarians. Nevertheless, surgery is the best chance of a cure,4 and should not be denied based on older age alone. Furthermore, the mortality rates associated to surgery have reached acceptable levels.5 In our study, we found that more than 40% of patients were submitted to some form of anticancer treatment. Only a minority of octogenarians presented in surgical staging, and only just over a quarter of them were submitted to surgery, with acceptable outcomes. The presence of significant comorbidities was a major reason for excluding surgery. In patients with contraindications to surgery, SBRT has emerged as an attractive treatment option.6 Two of our patients had SBRT, without significant morbidity. Chemotherapy was also performed in about a quarter of patients. In a recent study, octogenarians with NSCLC treated with chemotherapy showed prolonged survival compared with those submitted to BSC.7
Our results suggest that selected octogenarians with NSCLC, regardless of age, may benefit from specific anticancer treatment. Thus, a multidisciplinary assessment is recommended. Further studies are warranted to provide an optimal treatment approach for octogenarians.
Conflicts of interestThe authors have no conflicts of interest to declare.
Corresponding author. hansdabo@yahoo.com.br