Dear Editor,
Oxygen therapy, from prescription to administration, is still poorly handled,1, 2, 3, 4, 5, 6 and until the publication of “Guideline for emergency oxygen use in adult patients” by the British Thoracic Society1 there were very little literature about oxygen therapy procedures.1, 7
Recognizing the need to improve oxygen therapy procedures, the authors conducted an audit in 2008 to identify faulty practice and plan improvement measures. Three years later, a second audit was performed in order to evaluate those measures.
A taskforce consisting of physicians and nurses was set up in 2007 to evaluate OT practice in Internal Medicine wards of Hospital de Santo António, Oporto, Portugal. Based on the BTS guidelines, and according to NICE principles for best practice in clinical audit,3 an audit was designed to evaluate the different aspects of OT: prescription, transcription, administration and monitoring.
The audit was performed in two of the four wards of the department between January 1st and March 31st 2008. All patients to whom oxygen was administered or prescribed were included in the audit, except those with non-invasive ventilation during daytime. Assessments were performed two days per week. No assessments were performed at weekends, on Mondays, public holidays or the day after holidays, nor of patients admitted to the ward in the previous 24 h, to ensure all prescriptions were performed/validated by ward physicians.
Information of the audit was obtained from clinical records, nurses’ software application or direct patient observation. Statistical analysis was performed using IBM SPSS v11.0.
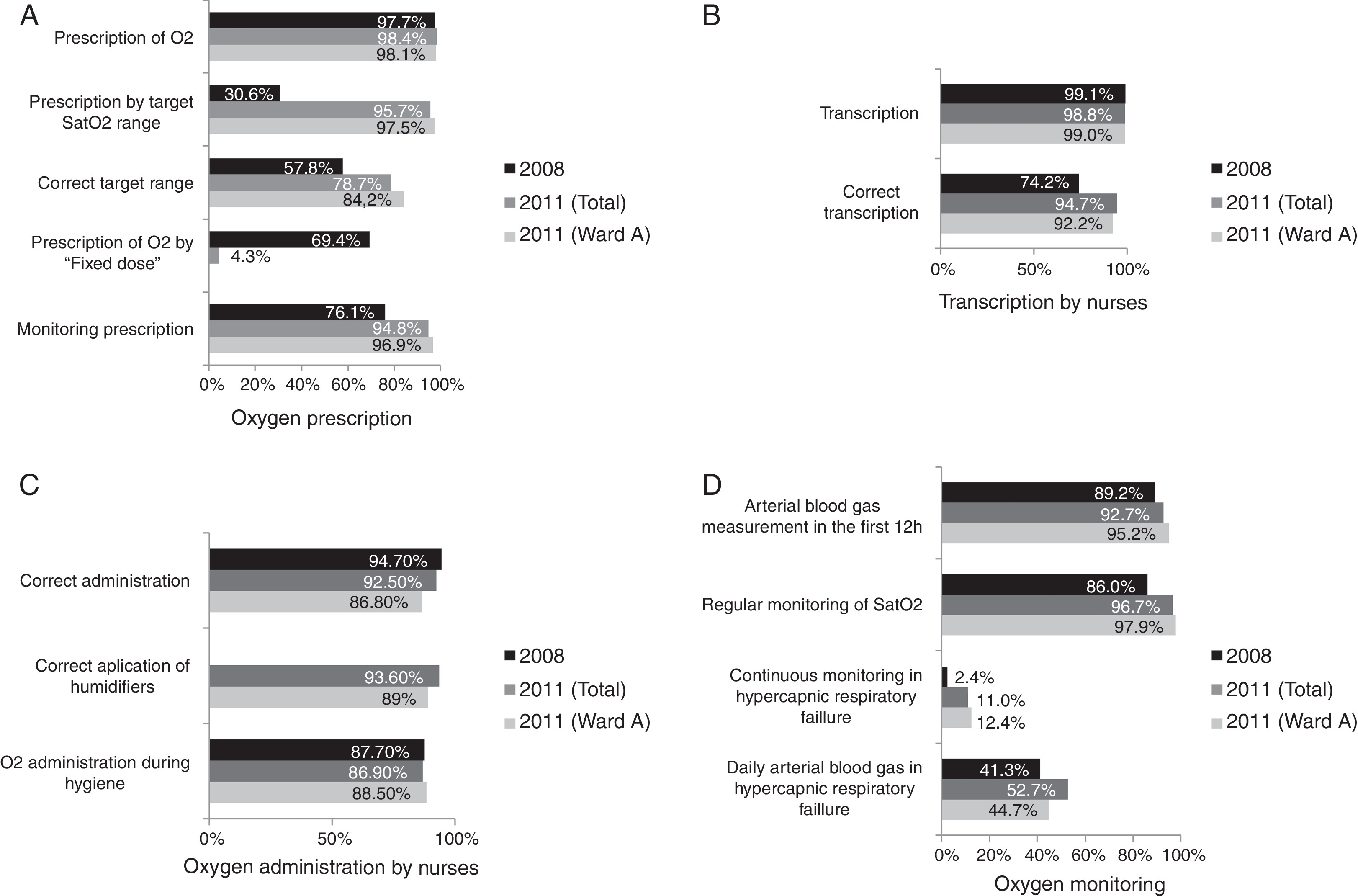
Results of the first audit are published elsewhere.5 The main findings are summarized here and presented in Figure 1A–D, in comparison with those of the second audit.
Figure 1. Comparison of results between the 2008 and the 2011 audits. (A) Oxygen prescription; (B) transcription by nurses; (C) oxygen administration by nurses (D) oxygen monitoring.
The authors considered that good practice was met whenever the rate of compliance was ≥90%. Based on this threshold, several criteria were identified as needing improvement. In relation to prescription, lack of a specific period of oxygen therapy institution and monitoring were the main problems. Prescription to target SatO2 range was observed in <50% of the patients. Transcription by nurses was incorrect in 26.8% of the patients. A significant number of patients on oxygen therapy had been correctly administered oxygen, but not during hygiene. In patients with acute hypercapnic respiratory failure, monitoring of oxygen administration was far from appropriate.
Several improvement measures were implemented: educational material was given to health professionals and patients; BTS guidelines were made accessible on all computers; training sessions were held in all wards of the department; an alert for hypercapnic respiratory failure was created on the prescription system; patients at risk of hypercapnic respiratory failure or in need of humidifiers were identified with bedside signs.
A re-audit was performed in all four wards between February 1st and April 31st 2011, using a similar methodology. Results were compared to those of the first audit; a separate comparison was also made between results in the wards audited in 2008 (A and D) and the corresponding ward in 2011 (Ward A – fusion of A and D).
This audit's results were better than those of other studies,2 including one multicentric study on OT performed in 24 Portuguese hospitals,8 where only prescription and administration were evaluated.
A significant increase of oxygen prescription to target SatO2 range was achieved (Figure 1A). Prescription by “fixed dose” OT was residual in 2011. A correct target range was observed in <90%, an acceptable value since some patients may benefit from specifically tailored ranges.1
There was a substantial improvement in the prescription of OT monitoring. There was also a clear improvement in the quality and accuracy of transcription (Figure 1B). Use of humidifiers cannot be compared to 2008 given no clear guidelines, regarding their use had existed at the time. Very good results were observed in 2011, with scarce (17.5%) but appropriate use (Figure 1C), in keeping with BTS guidelines.
There was no improvement in oxygen administration during hygiene (Figure 1C). An improvement in arterial blood gas measurement before or in the first 12 h of OT was achieved (Figure 1D). In patients with acute hypercapnic respiratory failure, monitoring is still far from appropriate (Figure 1D).
This study confirms the value of clinical audits in improving quality of care. A combined strategy of education, protocol implementation, universal use of target SatO2 range1 and software applications with safety alarms can improve OT in a hospital setting.
Conflicts of interestThe authors have no conflicts of interest to declare.
Acknowledgments
Besides the authors, the audit team included: Maria Barbosa, Cristiana Sousa, Sílvia Ramos, Paula Pereira, Joana Ramalho, Ana Oliveira Gomes, Carina Ribeiro, Joel Almeida, Margarida Carneiro, Bruno Pinto, Nelson Rocha, Alfredo Martins.
The authors would like to thank all other professionals from the Department of Internal Medicine who collaborated in data collection.
Corresponding author. sanpnunes@gmail.com