Adenosine deaminase (ADA) has been promoted as a quick, efficient and cost-effective method in the diagnosis of tuberculous effusions.1 However, the predictive parameters of ADA, in the diagnostic workup of tuberculous effusions, depend on the prevalence of the disease in the population2 and no such analysis has been published in Portugal, a country of intermediate tuberculosis (TB) incidence (25.9 per 100,000 in 2010).3
In response to this situation, we carried out a cross-sectional analysis over a 4-year period, beginning in January 2006, in which we evaluated pleural fluid results from all patients admitted to our department with a pleural effusion of unknown etiology. Only the results obtained from the first thoracocentesis were included and samples from empyema were excluded from our analysis. Pleural ADA was measured using Giusti's colorimetric method. Mann–Whitney test was performed to compare medians and a Receiver Operating Curve (ROC) was used to determine the predictive parameters of different cutoffs. Prism 6 from Graphpad Software was used for the statistical analysis.
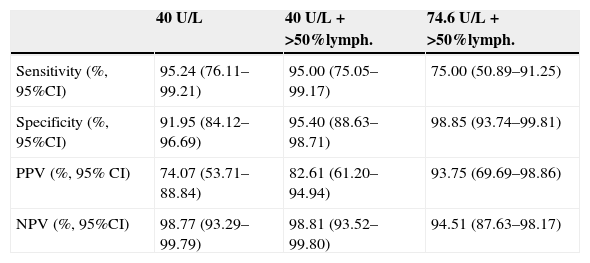
A total of 107 pleural samples were analyzed, including TB (n=20), malignant (n=54), parapneumonic (n=20) and idiopathic (n=13) effusions. Of the 107 patients, 57.9% were males, median age was 72.5 (interquartile range: 59.7; 80.2) and all the patients were of European ethnicity. TB pleural effusions were found to have the highest median ADA value (98.55U/L), which were significantly higher than malignant effusions (17.99U/L) (p<0.0001) – the group with second highest median ADA value. Using the ROC curve we found that an ADA cutoff of 40.5U/L had the best performance in the diagnosis of pleural TB (see Table 1), with a sensitivity of 95%, specificity of 91.55%, positive predictive value (PPV) of 73.08% and negative predictive value (NPV) of 98.77%. Seven nontuberculous exudates (8.0%) reached the diagnostic cutoff. Using a >50% lymphocyte count criteria in the diagnostic workup, only 4.5% nontuberculous exudates were misclassified – 2 malignant (plasmocytoma and lymphoma) and 2 parapneumonic. The association of these two criteria increased specificity (95.40%) and PPV (82.61%). Using an ADA cutoff level of 74.6U/L and the >50% lymphocyte criteria further increased specificity (98.85%) and PPV (93.75%), and only one (1.1%) nontuberculous exudate was misclassified.
Diagnostic parameters of different pleural fluid characteristics.
| 40U/L | 40U/L+>50%lymph. | 74.6U/L+>50%lymph. | |
|---|---|---|---|
| Sensitivity (%, 95%CI) | 95.24 (76.11–99.21) | 95.00 (75.05–99.17) | 75.00 (50.89–91.25) |
| Specificity (%, 95%CI) | 91.95 (84.12–96.69) | 95.40 (88.63–98.71) | 98.85 (93.74–99.81) |
| PPV (%, 95% CI) | 74.07 (53.71–88.84) | 82.61 (61.20–94.94) | 93.75 (69.69–98.86) |
| NPV (%, 95%CI) | 98.77 (93.29–99.79) | 98.81 (93.52–99.80) | 94.51 (87.63–98.17) |
PPV: positive predictive value; NPV: negative predictive value; lymph.: lymphocytes.
The diagnosis of tuberculous pleural effusion is a common diagnostic challenge due to low mycobacterial detection rates and to the frequent need for invasive, sometimes technically difficult, operator dependent techniques like the pleural biopsy or thoracoscopy.4 In this context, a rational interpretation of pleural fluid characteristics, particularly ADA level and differential leukocyte count, is essential to the diagnostic workup. In our research, an ADA level<40U/L can virtually exclude pleural TB with a NPV of 98.7%, while an ADA level>74.6U/L with >50%lymphocyte has a very high PPV of 93.75 and can thus be used to safely confirm pleural TB with a very small error rate of 1.1%. The performance of the cutoff value of 40U/L and the error rate of 4.5% (for ADA>40U/L and >50% lymphocytes) and 1.1% (for ADA<74.6U/L and >50% lymphocytes) is in line with other publications.2,5,6 In our analysis, one patient with pleural TB had an ADA level<40U/L; however, in a sample collected just 3 days later, ADA level was now 90U/L which reaffirms the diagnostic utility of ADA. Also, as we have shown, hematological malignancies are frequent causes of error, and they should be excluded by this analysis of the pleural lymphocyte populations.2,6 However, the usefulness of ADA in the diagnosis of tuberculous effusions depends on the prevalence of the disease in the population.2 If tuberculosis is highly prevalent, as in the African continent and Southeast Asia, then a high value of pleural ADA is more likely to be due to tuberculosis, thus increasing the PPV of pleural ADA in the diagnosis of pleural TB. If, however, the disease is less prevalent, the probability of a high ADA being due to other causes, such as cancer, increases, and PPV of pleural ADA is lower. This is most evident in countries with a low prevalence of tuberculosis and an aging population, as it is in old age that malignant effusions are more prevalent.
In conclusion, pleural ADA is a valuable tool in the diagnostic workup of pleural TB in Portugal and should routinely be used in the exclusion or confirmation of TB in the differential diagnosis of patients with a pleural effusion of unknown cause. Furthermore, in order to make a correct interpretation of its values, we have highlighted: potential false-positives; the usefulness of different ADA cutoffs for the exclusion or confirmation of TB; and the impact of TB prevalence on the predictive parameters of this tool.