Lung ventilation/perfusion scintigraphy with planar images (V/QS-planar) is very useful for the diagnosis and follow-up of pulmonary thromboembolism (PTE). Acquiring tomographic images (V/QS-SPECT) is a recent development with potential to increase the technique's accuracy. The purpose of this work is to evaluate the added benefits of V/QS-SPECT studies as opposed to traditional planar imaging.
Patients and methodsWe prospectively revised 53 V/QS-planar and V/QS-SPECT exams, performed according to the European Association of Nuclear Medicine guidelines. We evaluated the exams independently, by consensus of two Nuclear Medicine physicians. For both methods, we gave each lung a score expressing the dimension and extension of perfusion defects with normal ventilation. For each lung, we compared the scores with the paired Wilcoxon test, estimating the 95% confidence interval (95CI) for the respective difference.
ResultsWe performed V/QS-SPECT exams without technical difficulties. The paired Wilcoxon test estimated the score difference to be −0.75 (95CI of −1.0 to −0.5; p-value = 9.6 × 10−7), expressing a statistically significant difference of about 1 subsegmental defect between both methods, with V/QS-SPECT detecting more defects.
DiscussionThe results demonstrate that V/QS-SPECT identifies a slightly larger number of perfusion defects than V/QS-planar, suggesting a higher sensitivity of this technique. However, more studies are necessary to evaluate the clinical meaning of this fact.
ConclusionV/QS-SPECT demonstrates a higher capability to identify perfusion defects. This method looks promising, allowing for a greater role of this exam in pulmonary thromboembolism diagnosis and follow-up.
Pulmonary thromboembolism (PTE) is defined as the embolization of a blood clot to the pulmonary circulation.1 In fact, it is estimated that, in developed countries, it might be present lifelong on up to 5% of the population.2 It is also diagnosed in 1.5% of hospitalized patients and represents the third most frequent cardiovascular pathology (after myocardial infarction and cerebrovascular disease).3 Furthermore, it carries a high mortality, up to 5 to 10% of all in hospital deaths. Therefore, it is a public health problem.2
Acute PTE can present itself with very distinct signs and symptoms, ranging from haemodynamic instability, acute pulmonary hypertension, cardiac failure and systemic hypotension1 to clinically silent3 forms.
Chronic PTE is frequently a cause for cardiopulmonary disease, originating pulmonary infarction, chronic pulmonary hypertension and cor pulmonale.1
Despite the mentioned clinical relevance, PTE diagnosis is not always straightforward.3 Therefore, for greater diagnostic accuracy, imaging procedures are frequently needed.3
The imaging procedures used to diagnose PTE can be divided into anatomical and functional methods. As for the former, conventional pulmonary angiography was first described, which has been superseded by computerized tomography pulmonary angiography.3, 4 Recently, magnetic resonance pulmonary angiography has begun to be investigated.5
Functional methods have been represented by pulmonary ventilation and perfusion scintigraphy (V/QS), traditionally using planar imaging (V/QS-planar).3 V/QS-planar consists in obtaining two sets of scintigraphic images of the lungs: one representing pulmonary ventilation (by means of a radiopharmaceutical with alveolar air distribution) and another exhibiting pulmonary perfusion (with a radiopharmaceutical captured in the pulmonary capillaries). The scintigraphic diagnosis of PTE is based on the identification of pulmonary segments with a perfusion defect and preserved ventilation, consisting on a mismatch pattern. In planar imaging, the acquired images represent a projection of the totality of pulmonary ventilation and perfusion in different orientations: anterior, posterior, anterior oblique and posterior oblique, more frequently.
This procedure has been systematically improved in both sensitivity and specificity. In fact, since the demonstration of diagnostic accuracy of V/QS-planar in the PIOPED study,6, 7 different ways of enhancing the original technique have been investigated. Of note are the combination with results from other methods, namely simple chest X-ray,8, 9 and the introduction of new ventilation radiopharmaceuticals, such as radioaerossols, which allow the acquisition of ventilation studies with better diagnostic quality.10
A significant advantage of scintigraphic imaging, as opposed to the anatomical methods, is a lower radiological exposure.11 This is especially relevant when considering female patients subject to multiple exams for follow-up, given the high radiological sensitivity of breast tissue, which is especially exposed to radiation in anatomical thorax procedures.12 Also in pregnant patients, V/QS allows the reduction of radiological exposure not only to the breast, but also the foetus, in contrast to anatomical methods.13 Another VQ/S advantage is that it does not require the administration of iodinated contrast media, therefore presenting a more favourable pharmacological safety profile.
Finally, V/QS-planar is also the method of choice in chronic PTE suspicion as an aetiology for pulmonary hypertension, identifying those patients that benefit the most from directed therapy.14
The most recent development in V/QS was the introduction of pulmonary ventilation and perfusion tomographic imaging (V/QS-SPECT).15, 16 V/QS-SPECT has the same conceptual basis of V/QS-planar, the only difference being that in V/QS-SPECT tomographic reconstructions of pulmonary ventilation and perfusion are acquired, allowing the evaluation of axial, coronal and sagittal planes. This technique has a solid experimental support,17 appears to have higher diagnostic sensitivity than V/QS-planar18, 19 and does not seem to imply additional resource consumption.20 Besides, it compares favourably to computerized tomography pulmonary angiography.21, 22, 23 Its role in clinical decision making is beginning to be evaluated.24 V/QS-SPECT also seems to have a role in pulmonary physiology investigation.25
The purpose of this work is to evaluate the added benefits of V/QS-SPECT studies regarding the detection of perfusion defects compatible with PTE as opposed to traditional planar imaging.
Patients and methodsParticipantsWe studied prospectively V/QS exams performed on the same patient with both techniques under evaluation (V/QS-planar and V/QS-SPECT), in order to compare results.
The study population were the patients referred to the authors’ department to perform a V/QS for diagnosis or follow-up of PTE from September 2010 to September 2011. The patients were referred by the authors’ Institution outpatient clinics, hospital wards and emergency department, according to their physician's clinical judgement. We included in the study, by consecutive sampling, all patients who agreed to perform of both techniques. Inability or refusal by the patient to perform any of the modalities were the exclusion criteria.
MethodsWe compared V/QS-SPECT to V/QS-planar, since the latter is an established technique, available in every Nuclear Medicine Department.
We performed the exams following the appropriate European Association of Nuclear Medicine guidelines.26, 27 The exams were undertaken by an experienced Nuclear Medicine team (Nuclear Medicine physicians, technicians and nurses trained in radiopharmaceutical administration).
For the ventilation study, the radiopharmaceutical used was carbon radioaerossols marked with technetium-99m (Technegas, Cyclomedica); and for the perfusion study, albumin macroaggregates marked with technetium-99m (Macrotec, GE Healthcare). Both were administered with the patient in the supine position.
Both planar and tomographic images were acquired in a dual head gamma-camera (Millenium MG, GE Healthcare). Acquisition was sequential: first the ventilation study, with planar imaging followed by tomography, then the perfusion study, with tomography followed by planar imaging. This way we could minimize patient movement between both tomographic studies. We processed planar images in a general nuclear medicine workstation (Xeleris, GE Healthcare) and the tomographic study with a specific software package (LungSPECT, Segami).
According to the aforementioned guidelines, we considered an exam positive for PTE if it demonstrated at least one segmental perfusion defect with preserved, or less compromised, ventilation (mismatch pattern). For each exam and technique, we scored each lung for the number of pulmonary segments with a mismatch pattern. We considered subsegmental defects as fractions of segmental defects, giving each of them a score of 0.5. The scoring was done by two Nuclear Medicine physicians, who had no knowledge of the patient clinical data or the clinical report produced by the physician in charge of the exam. In those cases where the initial opinions were divergent, final consensus was reached after discussion between them.
Statistical methodsWe compared the scoring of each lung with the paired Wilcoxon test, estimating the 95% confidence interval (95CI) for the difference between V/QS-SPECT and V/QS-planar. We used the R language and environment for statistical computing to perform the statistical calculations.28
ResultsParticipantsWe enrolled patients for a period of 12 months. Fifty-three patients agreed to perform both V/QS modalities, 16 male and 37 female. The median age for the male gender was 54 (min = 36, max = 80) and for the female gender was 56 (min = 18, max = 82). All enrolled patients successfully completed both procedures, none being excluded. Of the 53 patients, 34 were referred for previous PTE re-evaluation and 19 for PTE diagnosis; 43 patients performed the exams in an outpatient setting and 10 patients were either admitted to a hospital ward or the emergency department at the time. All V/QS-SPECT exams were performed with the same human, material and time resources as V/QS-planar exams.
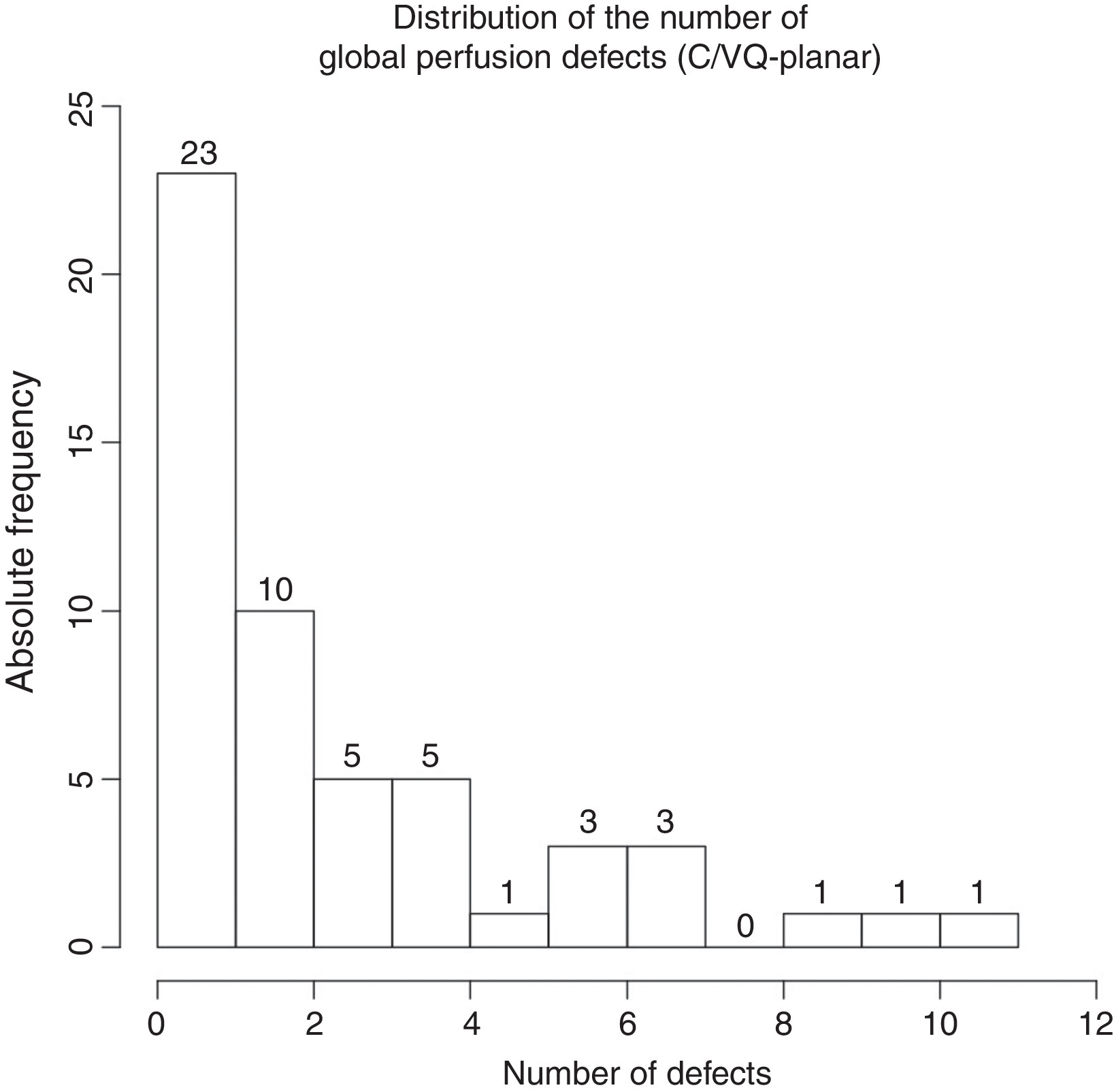
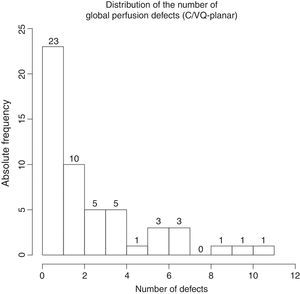
ResultsWe identified 30 exams with PTE using V/QS-planar, while the remainder 23 exams were considered normal. The distribution of the number of perfusion defects with preserved/less compromised ventilation documented per patient is presented in Figure 1. We observed that one-third of patients with PTE presents only one segmental defect or equivalent (n = 10), another third, two or three defects (n = 5 for both groups) and another third presents four or more segmental defects (the maximum being ten defects).
Figure 1. Distribution of the number of perfusion defects with preserved/less compromised ventilation documented per patient (V/QS-planar); PTE diagnosed for 1 or more defects.
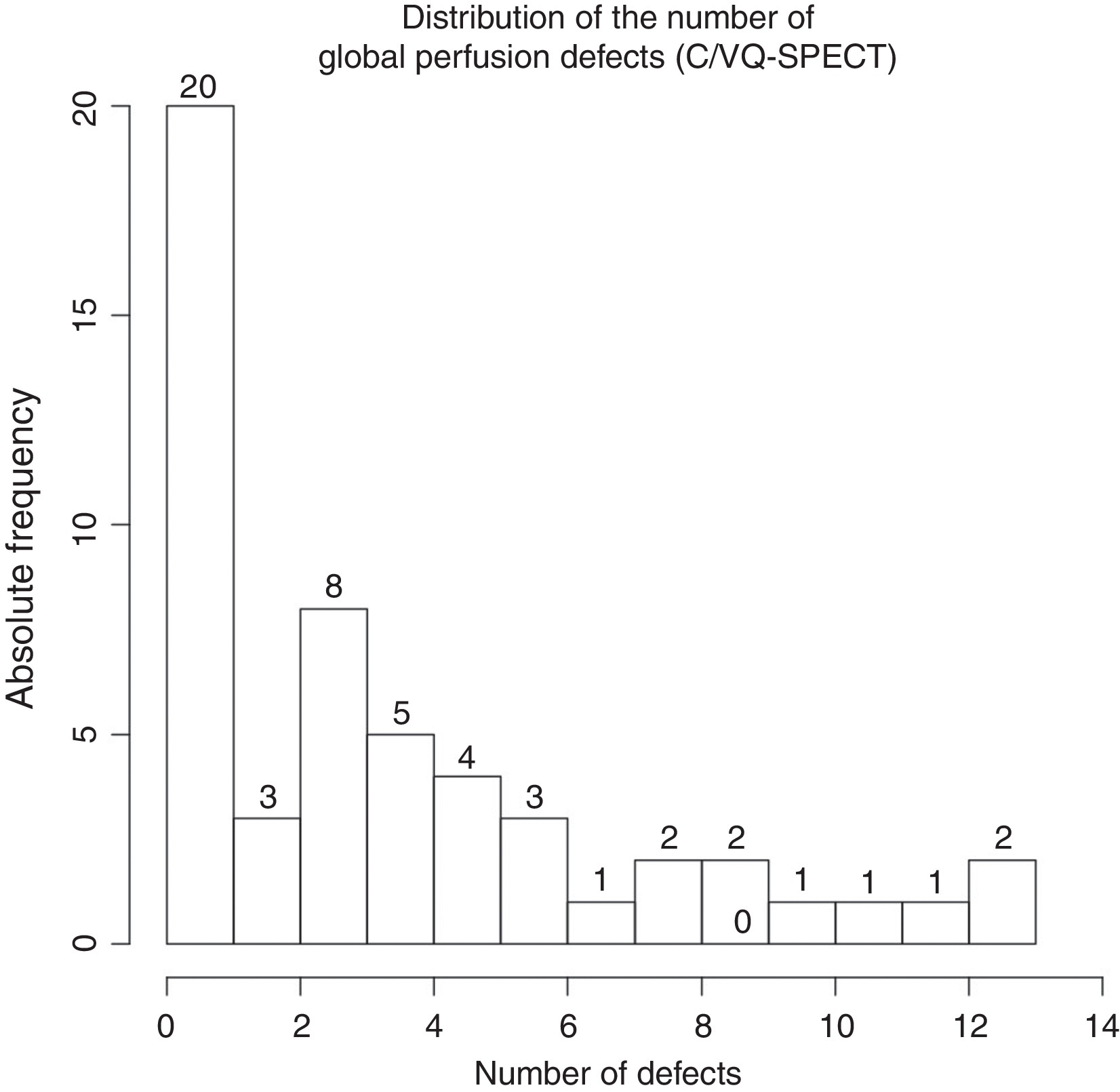
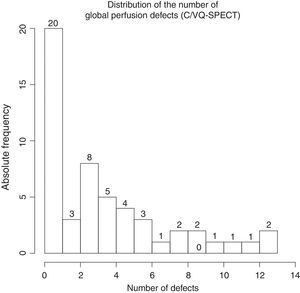
Regarding V/QS-SPECT, we identified 33 patients with PTE diagnostic criteria. The maximum number of defects observed was 13. Figure 2 presents this data distribution.
Figure 2. Distribution of the number of perfusion defects with preserved/less compromised ventilation documented per patient (V/QS-SPECT); PTE diagnosed for 1 or more defects.
In nine patients, the final conclusions of both modalities were in disagreement. In this group, six patients presented PTE diagnostic criteria only in V/QS-SPECT. The difference in the final diagnosis was due to a larger number and extension of mismatched defects identified by V/QS-SPECT versus V/QS-planar. The other three patients with different final results displayed PTE diagnostic criteria only in V/QS-planar. However, in two of these patients, V/QS-SPECT did show perfusion defects matched to ventilation defects; and on the third patient, there was a non-segmental distribution of perfusion defects. These features were not clear in V/QS-planar, given the natural overlap of lung segments and airways observed in this modality, which suggested a mismatch pattern instead.
There were no inconclusive results in both modalities, nor there were any adverse reactions recorded.
EstimatesThe paired Wilcoxon test, applied to the lung scoring, evidenced a difference of 0.75 between V/QS-SPECT and V/QS-planar (95CI of 0.45 to 1.00, p-value < 0.001).
DiscussionThe fact that all participants in the study successfully completed both modalities demonstrates that V/QS-SPECT does not present added technical difficulties in relation to V/QS-planar. It is noteworthy that 10 patients performed the exams while admitted to a hospital ward or the emergency department, settings in which difficulties in patient positioning and cooperation are usually expected. Besides, V/QS-SPECT did not demand additional resources (human, material, time) in relation to V/QS-planar. Therefore its performance presents no disadvantages to the patient or the Department and proficiency is easily achieved.
We observed, in both modalities, a large dispersion of the number of perfusion defects identified. This is in agreement with the known PTE clinical presentation spectre, which goes from sub-clinical to life-threatening.
We estimated a small, albeit statistically significant, difference of 0.75 in the scoring given to each lung between V/QS-SPECT and V/QS-planar. This value represents the V/QS-SPECT capability of identifying more perfusion defects than V/QS-planar. This is in agreement with reports of larger sensitivity for PTE diagnosis using V/QS-SPECT.18, 19 It should be noted that, in those cases presenting disagreement between both modalities, most patients presented PTE diagnostic criteria in V/QS-SPECT.
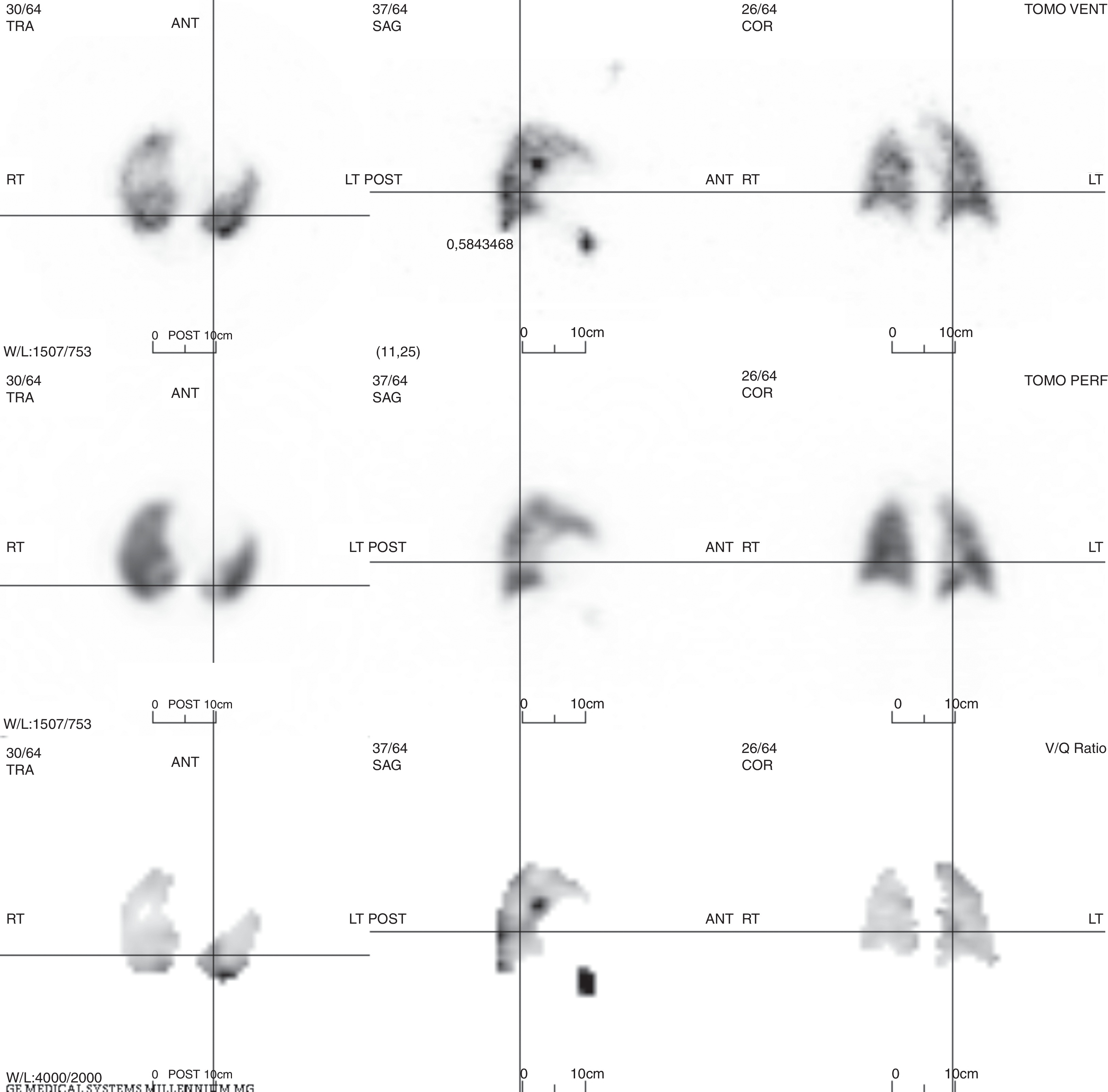
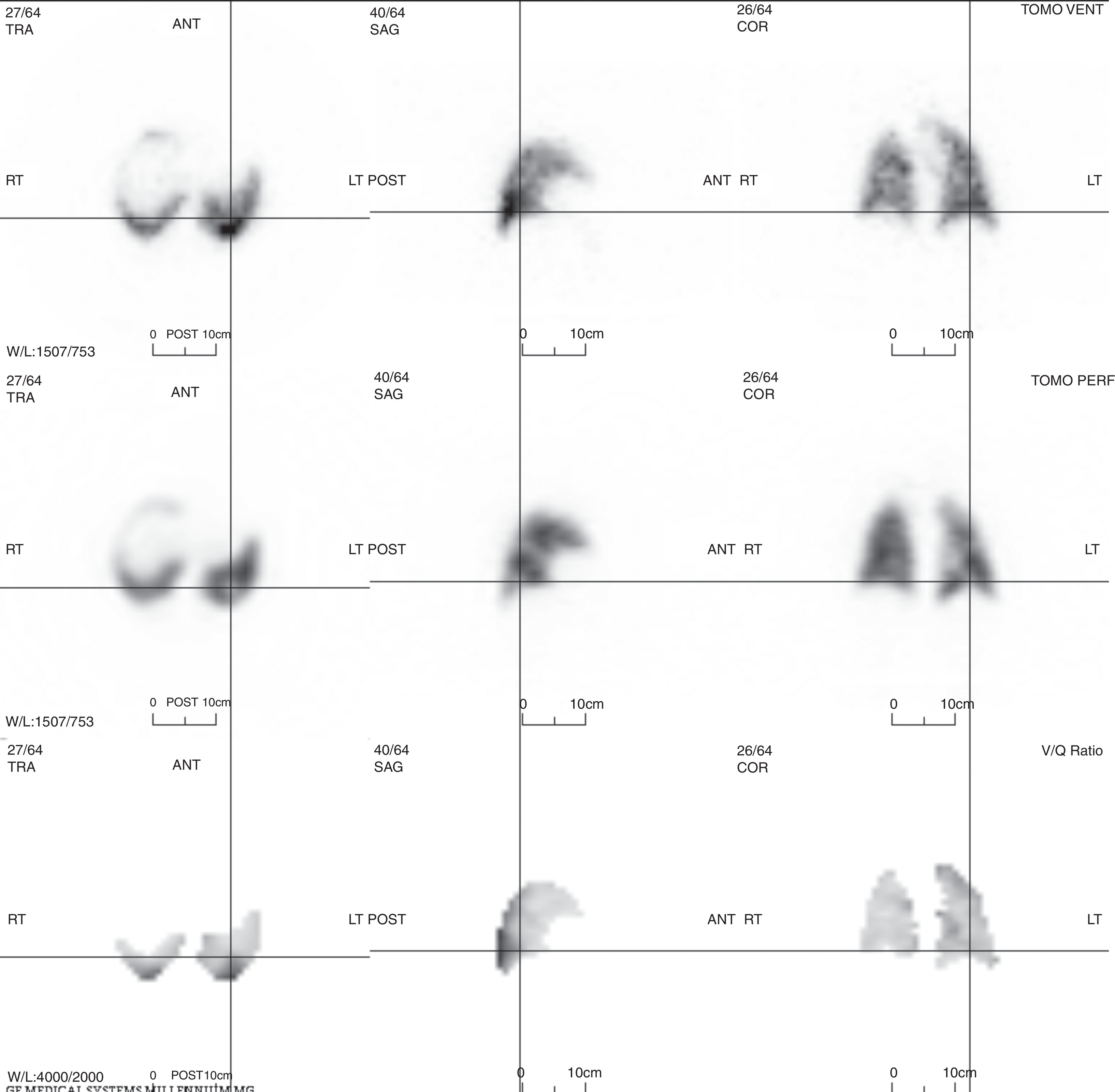
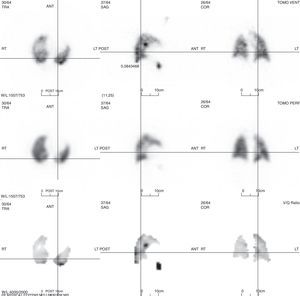
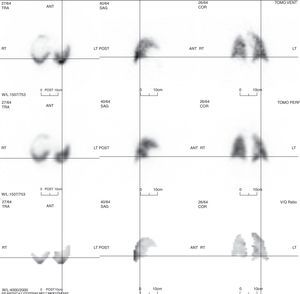
Figure 3, Figure 4, Figure 5 illustrate V/QS-SPECT larger sensitivity to detect perfusion defects. These examples demonstrate how, in one patient, V/QS-planar fails to correctly identify important perfusion defects, therefore failing to diagnose PTE, while V/QS-SPECT accurately documents them
Figure 3. V/QS-planar study; there is some heterogeneity in the perfusion of the left lung's lower lobe (white arrow), however it does not fulfil PTE diagnostic criteria and was disregarded as such.
Figure 4. V/QS-SPECT study, same patient as before; it is clear that there is a perfusion defect in the superior segment of the left lung's lower lobe (cross-hairs) fulfilling PTE diagnostic criteria.
Figure 5. V/QS-SPECT study, same patient as before; another perfusion defect fulfilling PTE diagnostic criteria, this time in the lateral basal segment of the left lung's lower lobe (cross-hairs).
This V/QS-SPECT advantage results from the technique's ability to study each lung segment separately. In contrast, V/QS-planar generates images where different structures overlap, a limitation that might hide some defects or wrongly characterize others.
This study did not evaluate V/QS-SPECT performance regarding specificity. However, it should be noted that three patients presented PTE criteria in V/QS-planar and not in V/QS-SPECT, due to a better definition of ventilation and perfusion defects by the latter modality. This fact seems to support the idea that V/QS-SPECT might also present gains in specificity, as opposed to V/QS-planar, as reported by other authors.18
As such, V/QS-SPECT is poised to become a method of choice in the diagnosis and follow-up of PTE, namely in young female patients or in a pregnancy setting,29, 30 as well as in patients which cannot be submitted to anatomical methods (mostly due to renal impairment, known allergy to radiological contrast media or incapacity to collaborate with the imaging protocol).
ConclusionsWe observed that V/QS-SPECT demonstrates a higher capability to identify perfusion defects. This study is in agreement with other works finding that V/QS-SPECT appears to present a slight increase in sensitivity and, possibly, in specificity for PTE diagnosis, as opposed to V/QS-planar. These features need further evaluation in new studies, better characterizing its role on pulmonary thromboembolism diagnosis and follow-up.
It is possible to easily introduce V/QS-SPECT into the clinical practice of a Nuclear Medicine department experienced in V/QS-planar performance. The new technique does not imply additional consumption of resources.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Acknowledgements
The authors thank the Department's Nuclear Medicine technician and nursing teams for collaborating in the acquisition of the exams.
Received 23 February 2015
Accepted 27 June 2015
Corresponding author. foss.jakomo@gmail.com