There are approximately 1,5 million smokers in Portugal, which represents 14,2% of the population.1 Having a smoking parent/caregiver increases the risk of a child or adolescent becoming a smoker from 8 to 25%.2
Brief intervention in smoking cessation generally takes between 5 and 15 min, including five sequential steps: “Ask, Advise, Assess, Assist and Arrange – The 5A's Model”.3 In primary care, the efficacy of brief intervention in an appointment is approximately 15% in terms of abstinence at 30 days.4 Data from the USA in 2016 showed that only 7% of pediatricians had training in smoking cessation and only 25% counselled parents to stop smoking. The main obstacles to intervention were lack of time, resources and training, associated with low acceptance from patients.5
In this study, we aimed to assess opinions, practices, obstacles, and knowledge in smoking cessation intervention in pediatricians regarding adolescents and parents/caregivers. To the best of our knowledge, this was the first Portuguese study assessing pediatricians’ behaviors towards smoking cessation intervention.
This was a cross-sectional study through an electronic anonymous questionnaire sent to all doctors enrolled in the Portuguese Paediatric Society in 2021. The questionnaire was elaborated according to the 5A's model. Respondents were asked separately about how they approached parents/caregivers and children/adolescents. The answers were structured using a 4-point Likert scale. The TabacoPed study was approved by Centro Hospitalar Universitário Lisboa Norte Ethics Committee.
We obtained 189 complete answers from a population of approximately 2300 pediatricians (response rate: 8,2%). The majority (79%, n = 149) were specialists, and 21% (n = 40) were residents. The average age was 39 years old (SD 9,5 years) and 83% (n = 156) were female. The majority (80%, n = 151) were non-smokers, 12% (n = 23) were ex-smokers and 8% (n = 15) were active smokers.
As for questioning smoking habits in children/adolescents, most pediatricians (87%, n = 164) mentioned doing it at least at the first appointment, and 25% (n = 47) question them at every appointment. Average age from which they ask about smoking firsthand is 14 years old (SD 1,6 years). The majority (74%, n = 140) ask while alone with the patient and 26% (n = 49) in the presence of a caregiver.
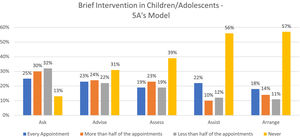
As for brief intervention in smoking cessation for children and adolescents in pediatric appointments, as we progress on the 5A's model, the number of doctors using brief intervention diminishes (Fig. 1). More than half (56%, n = 105) reported they never provide their patients counselling and/or pharmacotherapy (“Assist”) at any appointment.
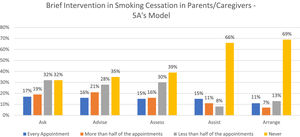
Regarding brief intervention in smoking cessation for caregivers, 68% (n = 129) of doctors ask about smoking habits at least during the first appointment. Two-thirds (66%, n = 125) of the respondents mentioned they never provide counselling and/or pharmacotherapy (“Assist”) (Fig. 2).
The majority (66%, n = 125) of pediatricians claim they are unaware of what brief intervention in smoking cessation is. Most (89%, n = 168) of the respondents had never had any training in smoking cessation programs and the vast majority (96%, n = 181) would be interested in doing such training, mostly through online courses, with an average duration of 10 h (SD 4,6 h).
The perceived main obstacles to intervention are patients’ lack of motivation (61%, n = 116), reduced time in appointments (59%, n = 112) and difficulty of referral to a smoking cessation clinic (42%, n = 80).
The results from our study show that brief intervention on smoking cessation is not widely used by pediatricians in Portugal, neither regarding adolescents nor parents/caregivers. Most pediatricians question adolescents and caregivers on their tobacco consumption habits during their first appointments. These percentages are similar to other medical specialties, like oncology, as depicted by Lina M, et al.6 However, the intervention remains a challenge specifically the final two steps of the 5A's model: providing counselling/pharmacotherapy (“Assist”) and scheduling follow-up contacts (“Arrange”).
Lack of training could be one of the contributing factors to the decline of intervention as we progress on the 5A's model, since only a minority of the respondents (11%) reported having had training in smoking cessation. These small numbers have also been described in Italy (6%) by Lina M, et al.6 and in Louisiana, USA, (7%) by Hall et al.5
Although two-thirds of respondents claimed unfamiliarity with brief intervention, nearly all were interested in having more training. The majority showed a preference for single-day online courses. This training could be offered either as part of postgraduate programs or pediatric residency. Concerning adolescents, specific strategies such as individual counselling, psychological support, nicotine replacement therapy and pharmacotherapy should also be included in the referred training programs.7
Acknowledging these gaps will facilitate the implementation of specific strategies adapted to pediatricians to improve their skills in brief intervention in smoking cessation, thus reducing secondhand smoke, and shaping a smoke-free generation.
DisclosuresAll authors have seen and approved the final version of the manuscript being submitted. All warrant that the article is the authors' original work, hasn't received prior publication and isn't under consideration for publication elsewhere.
Ethical considerationsThis study was approved by CHULN / Lisbon Academic Medical Centre's Ethical Committee on 24/07/2021.
To the Portuguese Paediatric Society for publicizing the study questionnaire to their associates.