A 47-year-old man, restorer of religious art, presents a three week history of asthenia, myalgia, dry cough and fever, coinciding with recent, unprotected exposure, to golden dust. He had fever, crackles in lung bases, hypoxemia and elevation of inflammatory markers. Imaging studies showed areas of parenchymal consolidation with air bronchograms in posterior-basal regions of both lungs, suggesting a pneumonic process. Lung function tests: mild restrictive pattern.
Bronchoalveolar lavage: lymphocytosis with low CD4/CD8 ratio. Lung biopsy: intraalveolar pneumonia with exsudative process and organization. Treatment with Prednisolone 40mg id was started with excellent response. First month follow-up CT scan showed areas of ground glass suggesting residual pneumonitis, and he resumed normal activities with excellent exercise tolerance, under appropriate protection measures.
Homem de 47 anos de idade, restaurador de arte sacra, apresenta história com 3 semanas de evolução de astenia, mialgias, tosse seca e febre, coincidindo com exposição recente e não protegida a poeiras de ouro. Encontrava-se febril, com crepitações inspiratórias nas bases pulmonares, hipoxémia e elevação dos marcadores inflamatórios. Radiologicamente: áreas de consolidação parenquimatosa com broncogramas aéreos postero-basais bilateralmente, sugerindo processo pneumónico. Provas funcionais respiratórias: padrão restritivo ligeiro. Lavado bronco-alveolar: linfocitose, baixo índice CD4/CD8. Biópsia pulmonar: pneumonia alveolar com processo exsudativo e organizativo. Iniciou terapêutica com prednisolona 40mg id com excelente resposta. TAC de controlo (1 mês): áreas de vidro-despolido sugerindo pneumonite residual. O doente retomou as suas actividades normais com excelente tolerância ao exercício, sob medidas de protecção adequadas.
Organizing pneumonia (OP) is an interstitial lung disease and a common nonspecific pathological response of the lung to injury.1
Its idiopathic form is called Cryptogenic organizing pneumonia (COP), also being known as Idiopathic bronchiolitis obliterans organizing pneumonia (or idiopathic BOOP).2 However the term cryptogenic organizing pneumonia (COP) is preferred because it conveys the essential features of the syndrome and avoids confusion with airway diseases such as constrictive bronchiolitis obliterans (which can be problematic with the term BOOP).3
The use of the generic term “organizing pneumonia” may be preferable, with modifiers as appropriate for etiology.3 Application of strict diagnosis criteria and thorough etiological investigation may drastically reduce the number of idiopathic forms.1
Considering the pulmonary effects of mineral exposure there are several papers on mining of gold mines, all relating lung lesions with exposure to silica, not gold. So, complication from gold dust exposure is a very hard to find thematic, currently existing no references on Medline about this subject.
Clinical case descriptionMale patient, 47 years old, sacred art restorer, former smoker, resorts to the Emergency room with three week evolution complaints of general malaise, muscle pain, persistent dry cough, fever and weight loss of approximately 8kg. During the same period he started an exhaustive work of restoration of gilded altars, exposing himself to a large amount of gold dust resulting from grinding and polishing the gold coating.
On clinical evaluation there was hyperthermia (38°C), no dyspnoea, hemodynamic stability, mild hypoxemia (SpO2 93%), and, on auscultation, there were sparse crackles in both lung bases.
Clinical analysis showed elevated Erythrocyte Sedimentation Rate (94mm), elevated C-reactive Protein (8,02mg/dL) and mild normocytic, normochromic anemia (11,9g/dL). Serology for infectious agents and research for autoantibodies were negative, as was the search for acid-alcohol resistant bacilli.
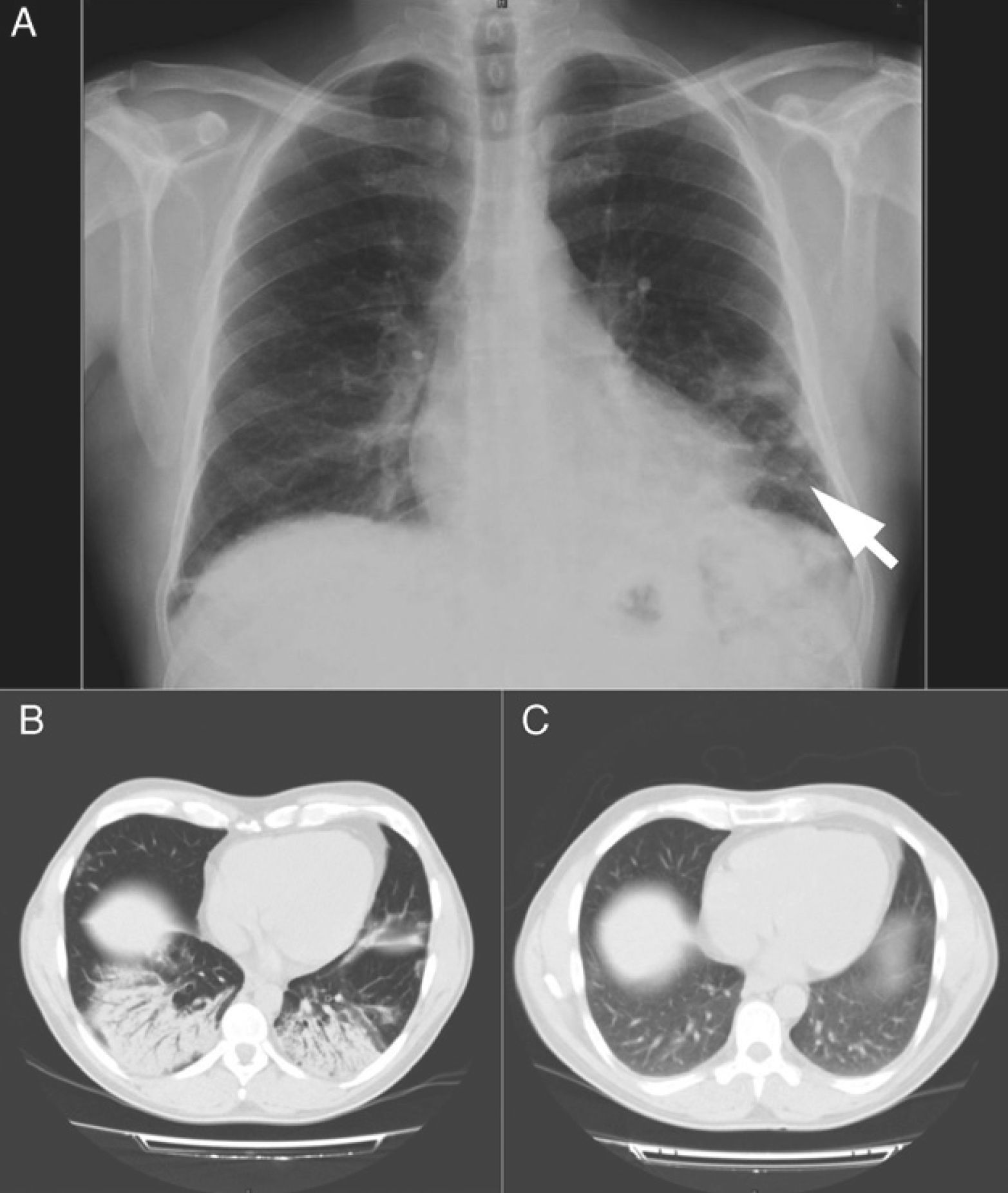
On chest x-ray there were clear interstitial nodular opacities at both bases, more evident on the left side (Fig. 1A).
Image 1A - Chest x-ray: interstitial nodular opacities at both bases, but more evident on the left side (arrow). Image 1B - High resolution CT scan: bilateral areas of parenchymal consolidation with air bronchograms in posterior-basal regions and the lingula strongly suggesting a pneumonic process. Image 1C - ground glass opacity in the lung bases and no evidence of parenchymal consolidation (1 month follow-up).
The high-resolution chest CT scan revealed that “(...) areas of parenchymal consolidation with air bronchograms in posterior-basal regions of both lungs and in the lingula, strongly suggestive of pneumonic process (…)” (Fig. 1B).
Lung function tests were also performed, revealing mild restrictive pattern and normal CO diffusion.
Optic bronchoscopy with bronchoalveolar lavage revealed increased cellularity with lymphocytic dominance (52%), and a low CD4/CD8 ratio (<1).
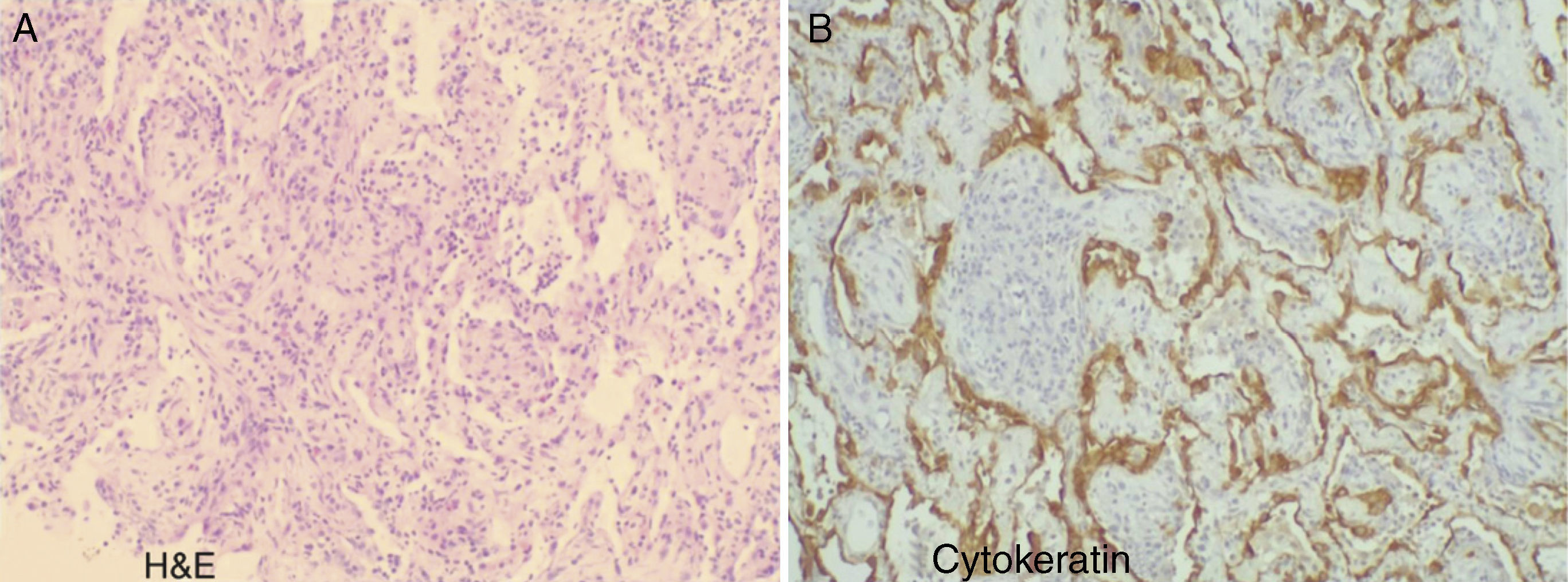
A transthoracic CT-guided biopsy was performed, with 2 tissue samples being retrieved. Histology revealed the existence of an organizational and exsudative intra-alveolar pneumonia process. (Fig. 2)
Lung histology (A – H&E, B – Cytokeratin): diffuse parenchymal lung changes; marked enlargement of the alveolar septa, foci of edema and mild to moderate lymphocytic infiltrate with rare neutrophils and some eosinophils. Frequent intra-alveolar myofibroblast proliferation with small nodules present. These are partially coated with highly reactive pneumocytes. No granulomas, vascular thrombi or neoplastic proliferation are identified. These aspects are indicative of a process of organizational and exsudative interstitial pneumonia.
In light of the clinical history and clinical and laboratory findings the diagnosis of Organizing pneumonia induced by chemical agent aggression was assumed. The patient started treatment with prednisolone 40mg id, with immediate apyrexia and gradual respiratory function improvement. Individual protection measures were also advised.
After one month the patient comes for consultation asymptomatic. The follow-up thoracic CT revealed images of ground glass opacity in the lung bases, with no evidence of parenchymal consolidation (Fig. 1C), which was quite an improvement. At this time slow tapering of prednisolone (5mg / month) was started. By the 3rd. month of follow-up all normal physical activities had been resumed, with no evidence of any changes on chest films or CT scan.
Discussion and conclusionOrganizing Pneumonia (OP) has clinical features of a flulike illness with cough, fever, malaise, fatigue, weight loss and inspiratory crackles frequently present on examination.4 These findings can be easily confused with a respiratory infection and lead to the administration of antibiotics.1
The differential diagnosis includes several clinical settings, which may be associated with an OP pattern: diffuse alveolar damage, infection, airways obstruction, aspiration pneumonia, drug reactions, fume and toxic exposures, collagen vascular disease, hypersensitivity pneumonitis, eosinophilic lung disease, inflammatory bowel disease, a secondary reaction in chronic bronchiolitis, and a reparative reaction around other processes (including abscesses, Wegener's granulomatosis, and neoplasms).3
To consider OP as cryptogenic, first any cause or associated disorder must be ruled out. So, a thorough investigation must be made in order to establish a possible cause for OP. In a recent case-series report from Barroso et al, only 17% of patients with an OP diagnosis presented a cryptogenic form.1
The clinical context, time of the disease and radiologic findings, selective serologic testing, bronchoscopy (including bronchoalveolar lavage) and lung biopsy are important for diagnosis. Correlation between histopathologic findings, the clinical context and radiologic findings is essential.5
In the presented case, the recent exposure to dust arising from the use of a gold microparticle polish product for the restoration of gilded altars became essential in guiding the etiological diagnosis.
Typical radiological changes were found either on Chest x-ray or high resolution Chest CT scan. Pulmonary function tests, although non-specific, showed a restrictive pattern and hypoxemia, also compatible with OP.
The bronchoalveolar lavage (BAL) cytology was consistent with organizing pneumonia. Although BAL cellular components may suggest a specific disease, these findings are not diagnostic. Unfortunately the delay between admission and the BAL execution did not allow for the identification of the causative gold microparticles.
Surgical lung biopsy is the standard for diagnosis.1-6 It is the most effective method for confirming the diagnosis and assessing disease activity.4 Biopsies from 2 separate sites are usually preferred, but a generous specimen from a site that is representative of the underlying process may suffice.5 An accurate diagnosis is important because it identifies patients most likely to benefit from therapy.6
Recent studies also showed that CT-guided transthoracic lung biopsy (a common procedure in our hospital) may prove to be a reasonable alternative to more invasive procedures (transbronchial and open surgical biopsies).7,8
The OP pattern is a patchy process characterized primarily by organizing pneumonia involving alveolar ducts and alveoli with or without bronchiolar intraluminal polyps, and buds of loose connective tissue and inflammatory cells filling alveoli and distal bronchioles.6
Case biopsy demonstrated an organizing pneumonia process. Since other causes were ruled out, the potential lung aggression from an inhaled chemical compound (containing mineral gold) was considered to be the etiological factor.
Glucocorticoid therapy - Prednisolone 1.0 to 1.5mg/kg/day - has good response and induces clinical remission within 4 weeks for two thirds6 of patients. At this time, if response is good, tapering is done to 0.5 to 1.0mg/kg/day. Therapy duration is around 6 months and prognosis is generally good, with full recovery observed in 2/3 of patients.2
This became a fact with our patient. After 4 weeks of therapy full clinical remission and radiological improvement were noticed (chest CT showed some remaining areas of ground glass). Normal physical activities were also resumed. Despite corticosteroid therapy, eviction of the causative agent is mandatory, in this case with the use of chemical protective masks.
Please cite this article as: Ribeiro PA, et al. Uma doença professional valiosa e abençoada — pneumonia organizativa devido a poeira de ouro. Rev Port Pneumol. 2011; 17: 182–185.