Central airway obstruction develops in a significant proportion of lung cancer patients and many other cancers through metastasis.1 Tumors that cause obstruction of the trachea and the main bronchi are often inoperable.2 Airway stenting is a therapeutic option for malignant central airway obstructions (MCAO) and is indicated for both intraluminal and extraluminal obstructions.3,4 There are several types of stents available and there is a progressive and improved experience of professionals regarding their management.3 Stenting is associated with immediate symptom relief and improved quality of life.5 Palliative and therapeutic benefits are well established, however, complications related to several types of metal and silicone stents are also reported. We report 5 years’ experience with stent placement in patients with MCAO, using rigid bronchoscopy (RB), between January 2015 and December 2019, at Centro Hospitalar Universitário São João.
Fifty-six stents were placed in patients with MCAO, 57.1% for lung cancer, regional extension by other malignancies including esophageal cancer (30.4%), head and neck (3.6%) and lung metastases (3 colorectal, 1 tongue sarcomaand 1 unknown primary). Baseline characteristics of the population and the characteristics of the obstruction observed by bronchoscopy are summarized in Table 1. Most patients had a single lesion, trachea (33.9%), right main bronchus (8.9%), bronchus intermedius (5.4%), left main bronchus (17.9%) and 33.9% of patients had an extended lesion. The severity of airway obstruction was determined using the Myer-Cotton grading system and forty-one patients (73.2%) had ≥ 71% airway lumen obstruction (Grade III or IV). In 10 cases tracheoesophageal fistula was detected.
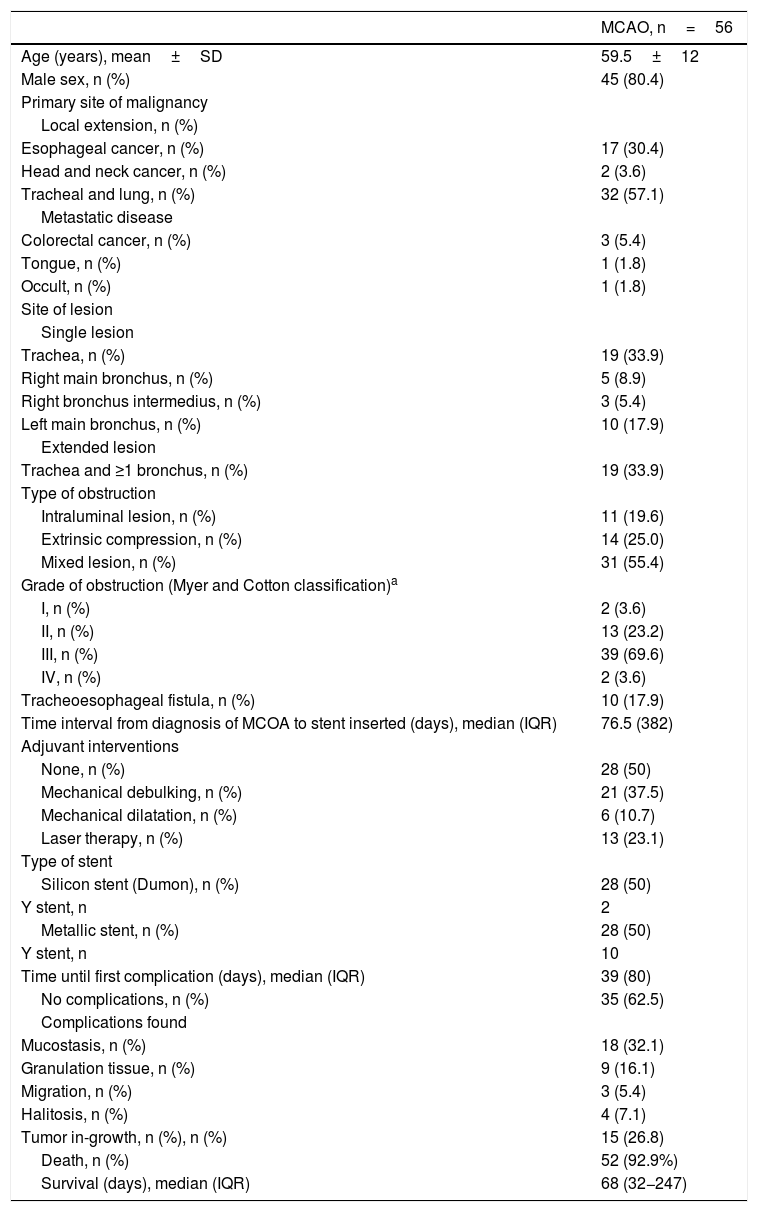
Baseline characteristics.
| MCAO, n=56 | |
|---|---|
| Age (years), mean±SD | 59.5±12 |
| Male sex, n (%) | 45 (80.4) |
| Primary site of malignancy | |
| Local extension, n (%) | |
| Esophageal cancer, n (%) | 17 (30.4) |
| Head and neck cancer, n (%) | 2 (3.6) |
| Tracheal and lung, n (%) | 32 (57.1) |
| Metastatic disease | |
| Colorectal cancer, n (%) | 3 (5.4) |
| Tongue, n (%) | 1 (1.8) |
| Occult, n (%) | 1 (1.8) |
| Site of lesion | |
| Single lesion | |
| Trachea, n (%) | 19 (33.9) |
| Right main bronchus, n (%) | 5 (8.9) |
| Right bronchus intermedius, n (%) | 3 (5.4) |
| Left main bronchus, n (%) | 10 (17.9) |
| Extended lesion | |
| Trachea and ≥1 bronchus, n (%) | 19 (33.9) |
| Type of obstruction | |
| Intraluminal lesion, n (%) | 11 (19.6) |
| Extrinsic compression, n (%) | 14 (25.0) |
| Mixed lesion, n (%) | 31 (55.4) |
| Grade of obstruction (Myer and Cotton classification)a | |
| I, n (%) | 2 (3.6) |
| II, n (%) | 13 (23.2) |
| III, n (%) | 39 (69.6) |
| IV, n (%) | 2 (3.6) |
| Tracheoesophageal fistula, n (%) | 10 (17.9) |
| Time interval from diagnosis of MCOA to stent inserted (days), median (IQR) | 76.5 (382) |
| Adjuvant interventions | |
| None, n (%) | 28 (50) |
| Mechanical debulking, n (%) | 21 (37.5) |
| Mechanical dilatation, n (%) | 6 (10.7) |
| Laser therapy, n (%) | 13 (23.1) |
| Type of stent | |
| Silicon stent (Dumon), n (%) | 28 (50) |
| Y stent, n | 2 |
| Metallic stent, n (%) | 28 (50) |
| Y stent, n | 10 |
| Time until first complication (days), median (IQR) | 39 (80) |
| No complications, n (%) | 35 (62.5) |
| Complications found | |
| Mucostasis, n (%) | 18 (32.1) |
| Granulation tissue, n (%) | 9 (16.1) |
| Migration, n (%) | 3 (5.4) |
| Halitosis, n (%) | 4 (7.1) |
| Tumor in-growth, n (%), n (%) | 15 (26.8) |
| Death, n (%) | 52 (92.9%) |
| Survival (days), median (IQR) | 68 (32−247) |
Data are presented as frequency (n) and percentage (%) or median and interquartile range (IQR).
MACO: malignant central airways obstructions; SD: standard deviation.
An equal number of silicone (n=28) and metallic (n=28) stents were placed. In addition to stent insertion, in half of the cases, another bronchoscopy modality was performed, including mechanical dilation, tumor mechanical debulking and laser therapy.
Twenty-one (37.5%) of all stents placed were associated with ≥1 complication, such as mucostasis (in 12 patients, secretions were easily removable by flexible bronchoscopy while in 6 patients RB was needed), migration (n=3), tumor in-growth (n=15), granulation tissue (n=9) and halitosis (n=4) (Table 1). The median time until first complication was 39 (16–96) days.
The occurrence of complications was independent of the type of stent placed (p=0.78), localization of obstruction (p=0.43), type of obstruction (p=0.69), origin of the malignancy (p=0.78), tracheoesophageal fistula (p=0.48) and the extent of the obstruction (p=0.08). However, there was a statistically significant difference between the number of complications and the presence of ≥71% airway lumen obstruction (p<0.05) and in patients with a y-stent (p<0.05).
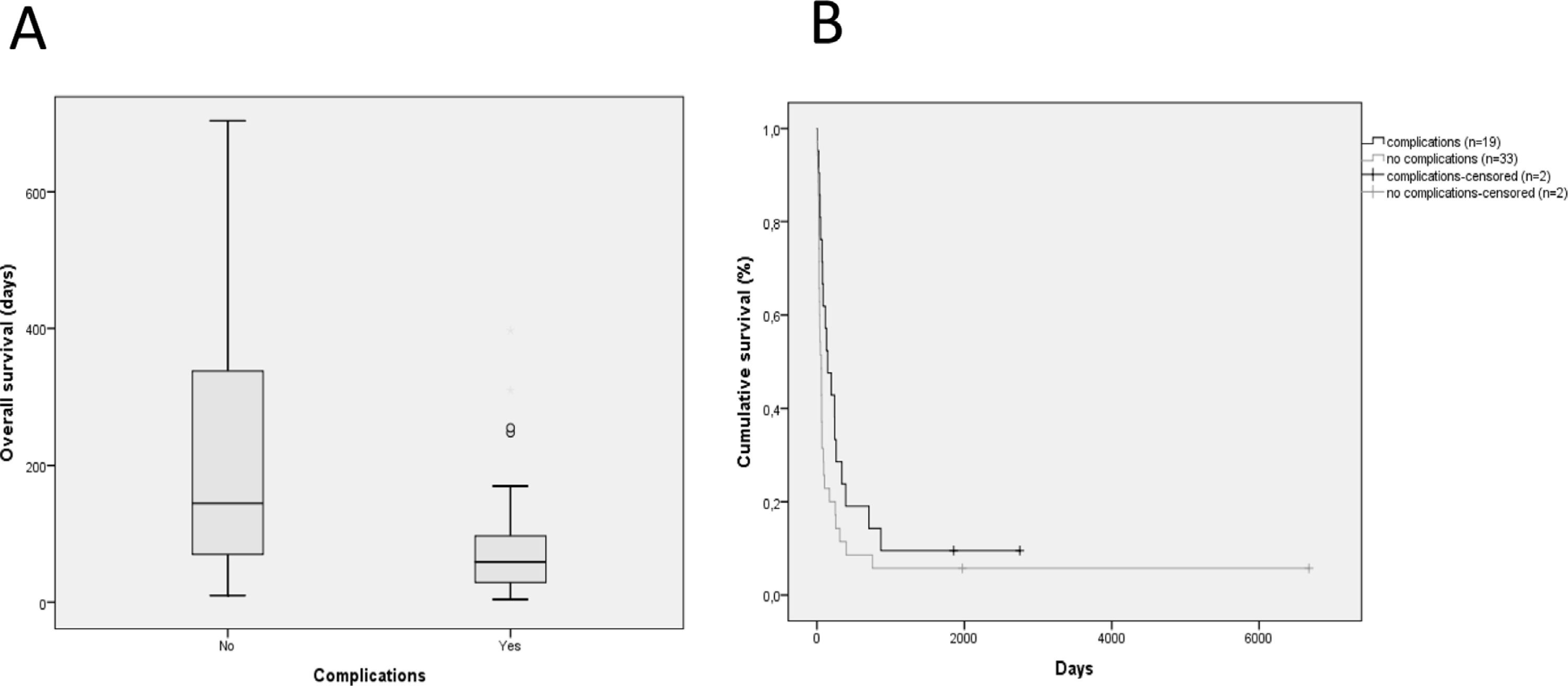
Overall, the median survival was 68 (32−247) days. The Kaplan-Meier method was used to estimate the overall survival after stent placement in relation to the origin of the neoplasia (pulmonary vs non-pulmonary), type of obstruction and occurrence of complications. According to the analysis (Fig. 1), the median time until death was 145 (70–338) days for patients with stent-related complications and 59 (28–103) days for patients without complications, this difference was the only statistically significant one (p<0.05).
(A) Box plot demonstrating survival difference (days of survival) in MCAO patients with stent-related complications versus patients without complications. (B) Kaplan–Meier curve for overall survival after stent placement in relation to the occurrence of stent-related complications (black) and the absence of stent-related complications (gray): + indicates censoring cases.
In patients with MCAO, bronchoscopic interventions can provide significant palliation of symptoms and quality of life.5 We report the experience of our bronchology department in the placement of stents in cases with MCAO. Stent placement requires a careful selection of patients and the type of stent, as well as knowledge and experience regarding the technique, follow-up and management of complications. Although several types of stents are available, the ideal type of stent for each situation is still a matter of debate.3 The main indications for stenting in MCAO are obstruction by extrinsic compression, endobronchial tumor with residual obstruction/malacia after bronchoscopic resection and malignant tracheoesophageal fistula.2 Prior to stent placement, it is important that the obstructive lesion is dilated and removed to facilitate stent deployment and obtain the best possible benefit, which is maintaining long-term airway patency.3
Stent-related complications are not uncommon3–5 and appear to be related to the median time of stenting.6 Mucostasis, tumor in-growth and granulation tissue were the most common stent-related complications in our patients. The median survival found in our study was 68 days, which is close to that estimated in other series,7,8 and the patients with longer survival after stent placement may be more likely to have ≥1 complication.
In conclusion, although this treatment potentially improves patients' symptoms and quality of life, we highlight the importance of regular and close monitoring to promptly diagnose complications in long cancer survivors.