This study carefully evaluates the association of different respiration-related events to each other and to simple nocturnal features in obstructive sleep apnea–hypopnea syndrome (OSAS). The events include apneas, hypopneas, respiratory event-related arousals and snores.
MethodsWe conducted a statistical study on 158 adults who underwent polysomnography between July 2012 and May 2014. To monitor relevance, along with linear statistical strategies like analysis of variance and bootstrapping a correlation coefficient standard error, the non-linear method of mutual information is also applied to illuminate vague results of linear techniques.
ResultsBased on normalized mutual information weights (NMIW), indices of apnea are 1.3 times more relevant to AHI values than those of hypopnea. NMIW for the number of blood oxygen desaturation below 95% is considerable (0.531). The next relevant feature is “respiratory arousals index” with NMIW of 0.501. Snore indices (0.314), and BMI (0.203) take the next place. Based on NMIW values, snoring events are nearly one-third (29.9%) more dependent to hypopneas than RERAs.
Conclusion1. The more sever the OSAS is, the more frequently the apneic events happen. 2. The association of snore with hypopnea/RERA revealed which is routinely ignored in regression-based OSAS modeling. 3. The statistical dependencies of oximetry features potentially can lead to home-based screening of OSAS. 4. Poor ESS-AHI relevance in the database under study indicates its disability for the OSA diagnosis compared to oximetry. 5. Based on poor RERA-snore/ESS relevance, detailed history of the symptoms plus polysomnography is suggested for accurate diagnosis of RERAs.
Obstructive sleep apnea–hypopnea syndrome (OSAS) is a sleep-related breathing disorder affecting 2–4% of the American adults in 1990s1 with an internationally increasing prevalence with greater obesity and aging.2,3 Frequent episodes of airway subsidence (apnea) or tapering (hypopnea) during sleep characterizes OSAS.4
Through abrupt changes in sympathetic neural activity, untreated OSAS may lead to severe cardiovascular side-effects.5–8 OSAS can also lead to type 2 diabetes,9 impaired cognition, and psychiatric symptoms.10 Therefore the early detection and treatment of OSAS is essential.
The gold standard for the OSAS diagnosis is overnight polysomnography (PSG). The PSG-driven apnea–hypopnea index (AHI) is used to characterize OSAS severity.11,12
However the contribution of other polysomnographic features to OSAS severity and symptoms is investigated in the literature. In one study the association of standard PSG features to variables reflecting disease burden and treatment outcome was examined using Spearman correlations and linear regression. These statistical tools did not show a consistent association between features in mild–moderate OSAS patients.13
In another study, the relationship between PSG features and chronic intermittent hypoxia (CIH) of OSAS patients was examined using multiple linear regression and covariance analysis. The achieved results showed “total sleep time” was the strongest predictor and may be better than AHI for evaluating CIH among OSAS patients.14
There is also a large body of literature on the relationship of bio-chemical factors to OSAS severity.14–18 In a multivariate linear regression model, AHI in rapid eye movement (REM) sleep was associated with increasing levels of hemoglobin A1c.15 Another investigation assessed OSAS severity in relation to levels of fibrinogen using the Chi-square and Wilcoxon rank-sum tests.16 In another research project the relevance of PSG-driven OSAS indices to serum thyroid hormones were examined by Mann–Whitney U test, the Pearson correlations and the regression models. These tools showed no significant difference in the level of hormones among OSAS patients. Only the mean apnea duration significantly correlated with thyroid-stimulating hormone (TSH).17
Simply acquired non-polysomnographic features are also studied. They can serve as predictors of OSAS severity before expensive and time-consuming PSG tests are requested for moderate to severe OSAS suspects. Obesity-related measures such as body fat distribution, neck circumference, and body mass index (BMI),18–20 body and trunk position,21,22 maxillary and mandibular study of oral cavity,20 and age23 are monitored.
The unpaired Student's t-test,18,23 the Mann–Whitney U test19 or the Wilcoxon signed-rank test21 was used to compare groups’ mean and the Pearson correlation plus multiple linear regression to examine relationships.18–21,23
Though most of the linear models were adjusted for multiple predictors, no association was found between sleep disordered breathing (SDB) and hypertension in those aged <60 years. Many of the calculated Pearson correlations were statistically significant, however, none had high values.23
In another attempt only the frequency of occurrence is reported for the defined position-dependent OSAS based on head and trunk position sensors and AHI.22
The observed controversy among the reported studies (i.e. some have reported a significant relationship in a very specific category of subjects under investigation23 and some failed to find a consistent association13) is mainly because all these studies considered only linear statistics such as comparison of means, correlation and regression. In regression, it is assumed that the predictable mean of outcome is dependent on one or more statistically independent predictors.24 The strong assumption of independency might not be true for many of the biological features.
To address this issue we have changed our statistical tool and compared the results with the conventional correlation method. Out of the previously researched factors we mentioned BMI which is an important risk factor and is included in STOP-BANG questionnaire as well. In other published papers the authors report on the relationship of OSA with the clinical symptoms.10 The purpose of this study is to get and overview of the relationship of each respiratory event (apnea, hypopnea, RERA and snoring) on AHI and their mutual relations using the strong method of mutual information (MI). To the best of our knowledge, such a study has not been conducted. MI checks dependency of all orders (not just the linear dependency or correlation). Based on the results more accurate OSAS prediction is possible by weighting the non-PSG driven features with their degree of dependency to AHI. OSAS prediction means initial OSAS screening based on simple nocturnal measures to refer only the medium or severe OSAS suspects to sleep laboratories.
Materials and methodsWe conducted this cross-sectional study at the sleep laboratory of Ibn-e-Sina Hospital, Mashhad, Iran, from July 2012 to May 2014. The study was approved by the ethics committee overseeing the research proposal (permission no. 92/620792, date 2014/03/07). We were allowed to use clinical data only, with no deviation from AASM protocol. The PSG (model: Alice LE, part no. 1002387, Philips Respironics) recordings were conducted in baseline montage with 16 channels on the 158 referred patients. Out of all participants, 134 subjects were diagnosed with OSAS and 24 ones were healthy according to International Classification of Sleep Disorders II (ICSD-II).11 The information regarding age, gender, weight, height, and medical history of the patients was gathered. The Epworth Sleepiness Scale (ESS)25 was calculated to assess daytime sleepiness and the BMI26 to evaluate obesity. Detailed history of the presenting symptoms was also requested. We ascertained sleep apneas as ≥10s of air flow pauses and hypopnea as a ≥3% of oxygen desaturation/or arousal proceeded by a 50% decrement in the amplitude of baseline airflow. We determined the severity of OSAS by AHI (AHI; mean number of apnea+hypopnea per hour of sleep). In this study, AHI was classified as mild (5–15), moderate (15–30), and severe (>30).11
The analyzed features are BMI, number of blood oxygen de-saturation levels below 95%, 90%, 80%, 75% in total sleep time, minimum and mean level of SpO2 (%) in total sleep time, minimum and maximum heart rates during sleep and non-REM (NREM) phase of sleep, ESS, indices of arousals (spontaneous, respiratory and snore arousals), total snore index, and indices of apnea, hypopnea and RERA.
Statistical analysisWe conducted a statistical study employing RapidMiner Studio (version 6.0.008) and MATLAB (version 10.0.49; R2010a) software.
All variables were tested for normal distribution preceding the analysis. Normality was considered by passing both the Lilliefors, and combined skewness and kurtosis tests. The adjustable non-normally distributed variables were log-transformed (AHI, min SpO2). Comparison between features’ means in four OSAS severity groups (healthy subjects, mild, moderate and severe OSAS patients) was performed using N-way analysis of variance, and multi-comparison tests.27 Differences were considered significant when p value was <0.05.
We chose the Spearman over the Pearson correlation since the assumption of normal distributions for the Pearson correlation was not met in many cases. We calculated correlations between AHI and other measures. To check if the values are accidental or not, the “bootstrapping” technique is applied. For bootstrapping, out of our 158-point data set we created a large number of “phantom” samples with random replacement to have 1000 different data sets. The sample correlation is then computed between all covariates for each data set (α=0.05), and the standard error of estimations calculated. When the numerical range of the estimated correlations does not contain zero, the correlation is non-accidental. The results are more accurate than the parametric case when the distribution behind the data is unknown.28
MI is a non-parametric measure of statistical dependency computed for our feature pairs.29 Dependence is more comprehensive than correlation and takes into account the non-linear relations of variables as well.
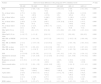
ResultsTable 1 presents the demographic details of the subjects under study. The results of multiple comparison tests are summarized in Table 2. The interval of difference between the estimated means of group pairs is the output of this test. When at least one of the intervals lacks zero (indicated by the shaded cells in Table 1) the corresponding P value is less than 0.05 and means are statistically significant. The features hypopnea index, BMI, number of blood oxygen de-saturation levels below 95% and 90%, and total snore index have the most distinctive means for the four specified groups and can differentiate between 4 and 5 group pairs out of all possible six pairs in Table 2.
Demographic details of the subject population.
| AHI range | No. of females | No. of males | AHI | Sleep (h) | Age (years) | BMI (kg/m2) | ESS |
|---|---|---|---|---|---|---|---|
| AHI<5 (hlt) | 9 | 15 | 2.5±1.5 | 5.8±1.4 | 34.3±11.2 | 23.8±3.9 | 10.3±9.8 |
| 5≤AHI≤15 (mld) | 12 | 20 | 9.4±2.7 | 5.6±1.2 | 42.6±11.7 | 27.6±5.2 | 9.3±5.6 |
| 15<AHI≤30 (mdrt) | 4 | 33 | 21.7±4.6 | 5.2±1.3 | 44.8±13.3 | 29.2±4.5 | 9.3±5.6 |
| AHI>30 (svr) | 9 | 56 | 63.4±26.8 | 3.7±1.5 | 49.3±11.7 | 31.5±6.1 | 11.7±5.6 |
Data are presented as mean±standard deviation. BMI: body mass index; AHI: apnea–hypopnea index; hlt: healthy; mld: mild OSAS; mdrt: moderate OSAS; svr: severe OSAS.
Unbalanced analysis of variance and multi-comparison tests of means.
| Feature | Interval of mean difference in the group pair (95% confidence level) | P value | |||||
|---|---|---|---|---|---|---|---|
| hlt–mld | hlt–mdrt | hlt–svr | mld–mdrt | mld–svr | mdrt–svr | ||
| BMI | [−7.4, −0.1] | [−8.9, −1.8] | [−10.9, −4.5] | [−4.9, 1.7] | [−6.9, −1.0] | [−5.1, 0.5] | 0.000 |
| No. of desat. below 95% | [−73.3, 3.4] | [−104, −29.5] | [−185, −117.2] | [−66.1, 2.5] | [−146.8, −85.4] | [−113.6, −55.1] | 0.000 |
| No. of desat. below 90% | [−62.9, 16.8] | [−85.2, −7.9] | [−166.5, −96] | [−59.1, 12.1] | [−140.1, −76.4] | [−115.1, −54.4] | 0.000 |
| No. of desat. below 80% | [−28.8, 26.9] | [−31.0, 23.1] | [−64.7, −15.4] | [−28, 21.9] | [−61.4, −16.8] | [−57.3, −14.8] | 0.000 |
| No. of desat. below <75% | [−22.8, 22.1] | [−23.4, 20.2] | [−46.7, −7] | [−21.3, 18.8] | [−44.4, −8.5] | [−42.3, −8.1] | 0.000 |
| Min. SpO2 (%) in sleep | [−2.5, 11.2] | [0.4, 13.7] | [5.9, 18] | [−3.4, 8.8] | [2.1, 13.0] | [−0.3, 10.1] | 0.000 |
| Mean SpO2 (%) in sleep | [−1.6, 5.7] | [−1.1, 6] | [2.6, 9.1] | [−2.8, 3.7] | [0.9, 6.8] | [0.6, 6.2] | 0.000 |
| Min. HR. in NREM sleep | [−6.2, 8.4] | [−9.4, 4.8] | [−9.7, 3.2] | [−9.9, 3.1] | [−10.2, 1.4] | [−6.6, 4.6] | 0.218 |
| Max. HR. in NREM sleep | [−13.3, 8.5] | [−15.7, 5.5] | [−12.9, 6.4] | [−12.4, 7.1] | [−9.5, 7.9] | [−6.4, 10.1] | 0.664 |
| Min. HR. in sleep | [−6.7, 7.7] | [−9.6, 4.4] | [−10.2, 2.6] | [−9.5, 3.3] | [−10, 1.5] | [−6.7, 4.3] | 0.195 |
| Max. HR. in sleep | [−12.2, 9.2] | [−13.8, 7] | [−11.7, 7.3] | [−11.5, 7.7] | [−9.2, 7.9] | [−6.9, 9.4] | 0.858 |
| ESS | [−3.3, 6.0] | [−3.0, 5.8] | [−5.1, 3.1] | [−4.1, 4.1] | [−6.1, 1.3] | [−5.8, 1.1] | 0.236 |
| Spontaneous arousals index | [−10.6, 4.8] | [−2.0, 12.9] | [−1.2, 12.6] | [1.4, 15.2] | [2.5, 14.8] | [−5.5, 6.2] | 0.001 |
| Respiratory arousals index | [−11, 6.1] | [−13.7, 2.8] | [−31.4, −16.3] | [−10.6, 4.6] | [−28.2, −14.6] | [−24.9, −11.9] | 0.000 |
| Snore arousals index | [−5.3, 1.5] | [−8.4, −1.8] | [−6.6, −0.6] | [−6.2, −0.2] | [−4.4, 1] | [−1.1, 4.1] | 0.000 |
| Snore index | [−261.6, 73.6] | [−564.8, −239.5] | [−464.7, −168.3] | [−458, −158.3] | [−356.5, −88.5] | [−42.2, 213.4] | 0.000 |
| Apnea index | [−15.6, 11.6] | [−20.3, 6.1] | [−51.3, −27.2] | [−17.2, 71] | [−48.1, −26.3] | [−42.5, −21.8] | 0.000 |
| Hypopnea index | [−11.8, 2.1] | [−18.9, −5.4] | [−27.7, −15.4] | [−13.5, −1.1] | [−22.2, −11.1] | [−14.7, −4.0] | 0.000 |
| RERA index | [−2.6, 0.5] | [−2.2, 0.7] | [−1.5, 1.1] | [−1.1, 1.6] | [−0.3, 2.1] | [−0.6, 1.7] | 0.172 |
Note: hlt=healthy; mld=mild OSAS; mdrt=moderate OSAS; svr=severe OSAS; no. of desat. below X%=number of blood oxygen de-saturation levels below X% in total sleep time; Min.=minimum; Max.=maximum; HR.=heart rate.
The results of the bootstrapped correlation analysis are summarized in Table 3. All the features in Table 2 are considered. The shaded rows of Table 3 indicate those pairs that have a non-accidental correlation. Obviously apnea/hypopnea indices have a strong positive correlation with AHI as they are directly used for its computation. However, correlation of AHI values with apnea indices is nearly two times more (0.9109 versus 0.5512) which indicates a stronger linear dependence to apnea index values. Blood oximetry parameters, BMI, and respiratory arousals are the next AHI-correlated features. A degree of non-accidental correlation is detected between the pair “AHI – number of spontaneous arousals”. According to Tables 2 and 3, maximum and minimum heart rates and ESS do not have non-accidental correlation with AHI.
Correlation analysis of features.
| Feature pair | Crr cff | P value | Es err | [min., max.] |
|---|---|---|---|---|
| AHI & BMI | 0.4540 | 0.000 | 0.0728 | [0.1890, 0.6717] |
| AHI & No. of desat. below 95% | 0.7508 | 0.000 | 0.0398 | [0.6273, 0.8698] |
| AHI & No. of desat. below 90% | 0.7488 | 0.000 | 0.0349 | [0.6431, 0.8468] |
| AHI & No. of desat. below 80% | 0.6053 | 0.000 | 0.0557 | [0.3723, 0.7697] |
| AHI & No. of desat. below 75% | 0.5610 | 0.000 | 0.0644 | [0.3405, 0.7609] |
| AHI & Min. SpO2 (%) in sleep | −0.5098 | 0.000 | 0.0754 | [−0.7214, −0.1917] |
| AHI & Mean SpO2 (%) in sleep | −0.5747 | 0.000 | 0.0691 | [−0.7883, −0.3347] |
| AHI & Min. HR in NREM sleep | 0.2201 | 0.005 | 0.0761 | [−0.0205, 0.4321] |
| AHI & Max. HR in NREM sleep | 0.0977 | 0.2219 | 0.0773 | [−0.1087, 0.3629] |
| AHI & Min. HR in sleep | 0.2277 | 0.004 | 0.0735 | [−0.0136, 0.4409] |
| AHI & Max. HR in sleep | 0.0798 | 0.3189 | 0.0748 | [−0.0865, 0.3743] |
| AHI & ESS | 0.0358 | 0.5121 | 0.0752 | [−0.0975, 0.3834] |
| AHI & spontaneous arousals index | −0.2454 | 0.002 | 0.0602 | [−0.4945, −0.1683] |
| AHI & respiratory arousals index | 0.7442 | 0.000 | 0.0452 | [0.5819, 0.8810] |
| AHI & snore arousals index | 0.1329 | 0.096 | 0.0818 | [−0.0582, 0.4463] |
| AHI & snore index | 0.3446 | 0.000 | 0.0638 | [0.1597, 0.5547] |
| AHI & apnea index | 0.9109 | 0.000 | 0.0138 | [0.8555, 0.9465] |
| AHI & hypopnea index | 0.5512 | 0.000 | 0.0829 | [0.2806, 0.7716] |
| AHI & RERA index | −0.1201 | 0.133 | 0.0840 | [−0.3107, 0.2026] |
| Snore index & hypopnea index | 0.3314 | 0.000 | 0.0675 | [0.1052, 0.5688] |
| Snore index & RERA index | −0.0453 | 0.572 | 0.0809 | [−0.2899, 0.2147] |
| ESS & RERA index | 0.0155 | 0.071 | 0.0750 | [−0.1202, 0.1137] |
Correlation coefficient: Crr cff; bootstrapped standard error: Es err; range of estimated correlation coefficient: [minimum value, maximum value].
The correlations of hypopnea with snoring and RERA with ESS/snore are also investigated. The results are tabulated in the last three rows of Table 3; there is a non-accidental correlation between snoring and hypopnea, but not between snoring and RERA. ESS also is not significantly correlated with RERA.
To compare the correlation coefficients (Table 3) with results of MI analysis, the calculated MI values are normalized between 0 and 1 and called normalized mutual information weights (NMIW).
Table 4 consists of the NMIWs of the same features pairs as those of Table 3. According to Table 4, NMIW of “AHI and hypopnea index” is 1.3 times more than that of “AHI and apnea index” (0.572 versus 0.44). This result is concordant with that of correlation analysis. The NMIW for “AHI and number of blood oxygen desaturations below 95%” has a considerable value of 0.531. “Respiratory arousals index” (NMIW: 0.501), snore index (NMIW: 0.314), and BMI (NMIW: 0.203) are next relevant measures to AHI. Maximum and minimum heart rates and ESS do not have significant MI with AHI (NMWI range: 0.03–0.194).
The normalized mutual information weights.
| Feature pairs | NMIW |
|---|---|
| AHI & BMI | 0.203 |
| AHI & No. of desat. below 95% | 0.531 |
| AHI & No. of desat. below 90% | 0.456 |
| AHI & No. of desat. below 80% | 0.296 |
| AHI & No. of desat. below 75% | 0.169 |
| AHI & Min. SpO2 (%) in sleep | 0.214 |
| AHI & Mean SpO2 (%) in sleep | 0.271 |
| AHI & Min. HR in NREM sleep | 0.137 |
| AHI & Max. HR in NREM sleep | 0.194 |
| AHI & Min. HR in sleep | 0.137 |
| AHI & Max. HR in sleep | 0.194 |
| AHI & ESS | 0.03 |
| AHI & spontaneous arousals index | 0.121 |
| AHI & respiratory arousals index | 0.501 |
| AHI & snore arousals index | 0.238 |
| AHI & snore index | 0.314 |
| AHI & apnea index | 0.572 |
| AHI & hypopnea index | 0.44 |
| AHI & RERA index | 0.046 |
| Snore index & hypopnea index | 0.818 |
| Snore index & RERA index | 0.573 |
| ESS & RERA index | 0.02 |
The last three rows of Table 4 indicate interesting information about the degree of dependence between snoring and hypopneas/RERAs. Correlation analysis denies any considerable non-random correlation between snoring and RERAs, but NMIW values show a degree of high-order dependence between them; snoring events however, are 29.9% more dependent to hypopneas than RERAs. The NMIW between ESS and RERA is the least reported value (0.02) which indicates a non-considerable relation.
DiscussionThe contribution of different factors to OSAS severity is investigated in literature from polysomnographic features13–14 to non-polysomnographic ones.14–23 All these attempts, however, considered only linear methods which are not strong and careful enough.29 When possible, correlation analysis should be accompanied by the bootstrapping technique to consider random effects and unknown data distribution. This is generally disregarded in the previous literature. To reach more reliable results we have checked the statistical dependence of all orders, by computing MI. This aspect is completely ignored in all the previous relevant works.
We also searched for any hidden relationship of the respiratory features to each other. Conventionally the exploited predictive models are regression-based with the strong assumption of predictors’ independency. Our achievements showed this is not true for all the tested biological features. We found that dependency of hypopneas and RERAs to snoring should not be ignored and, snoring is 29.9% more dependent on hypopneas than RERAs. However, the relationship of RERA to ESS is not extensive.
The parameters related to N3 and REM phases of sleep are deliberately ignored since the protocol of PSG test is done in split night format in which the sleep is terminated and CPAP therapy and titration is started when AHI>20.11 Hence the sleep structure may lack REM and/or N3 stage of non-REM phase. We were completely aware of the fact that most of respiratory events occur during the night REM periods. Meanwhile in published references, it is asserted that the 2h-AHI and 3h-AHI correlated strongly with the full night-AHI even after adjusting for percentage of REM sleep.30 Moreover, out of 158 subjects 70 ones were certified by the sleep laboratory as having had split night PSG and we wanted to take advantage of this data as well as full night PSGs to have more statistically significant results.
Poor relation of “ESS” with AHI and RERA index states that ESS alone does not appear to be helpful for the diagnosis of SDB compared to PSG and oximetry. This fact is stated in published works of other groups as well.31
Results of MI analysis showed that AHI values are 1.3 times more relevant to apneas than hypopneas. This result is in agreement with that of correlation analysis. Hence though both apneas and hypopneas have the same quantitative weights in AHI calculation, the more severe the OSAS is, the more frequently the apneic events happen in the population under investigation.
Multi comparison and MI analysis showed obvious association of OSAS severity to features that do not need PSG test to be calculated; the measures of blood oxygen desaturation, snore index and BMI. The viability of home-based OSAS estimates by nocturnal pulse oximetry parameters is indicated in literature.31–33
Respiratory arousal index as a measure of brain response to respiratory events is the next AHI-dependant feature.
The low value of dependence for (Snore – RERA) and (ESS – RERA) suggests that snoring and ESS values are not conclusive about presence of RERAs. Detailed history of the other presenting symptoms including more informative questions on daytime sleepiness, and morning dry mouth should be taken and accompanied by PSG for accurate RERA diagnosis.
ConclusionThe NMIW values quantified the amount of statistical dependence between respiratory events; indices of apneas are 1.3 times more relevant to AHI values than those of hypopneas despite similar weights in AHI calculation. Hence in the surveyed population, the more severe the OSAS is, the more frequently the apneas happen. Also snoring events have a nearly one-third more dependent relationship with hypopneas than RERAS. Meanwhile, correlation analysis (as a conventional tool), has shown no non-accidental linear relation between RERAs and snoring.
Considerable dependence of AHI on the measures of blood oxygen desaturation confirms the viability of estimating OSAS severity by blood oximetry parameters and designing home-based OSA screening devices. The insignificant relationship between ESS and OSAS severity indicates the inability of this measure alone to diagnose OSAS. Low dependence of RERA to snoring and ESS suggests that snoring and ESS values are not conclusive about presence of RERAs. Detailed history of the other presenting symptoms plus PSG is suggested for accurate diagnosis of RERA.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors appreciate the cooperation of Ibn-e-Sina Hospital sleep laboratory at Mashhad University of Medical Sciences.