Bronchiectasis is defined as an abnormal and irreversible dilation and distortion of the bronchi, which has numerous causes. Surgical treatment of this disease is usually reserved for focal disease and when the medical treatment is no longer effective. We report our center experience and outcomes in bronchiectasis surgery during the last 20 years.
MethodsBetween 1994 and 2014, sixty-nine patients underwent surgical resection for bronchiectasis. Patient demographics, presenting symptoms, indications for surgical treatment, type of lung resection, morbidity and mortality, as well as clinical follow-up and outcomes were analyzed.
ResultsFrom the 69 patients included, 31 (44.9%) were male and 38 (55.1%) were female. Surgery was indicated because of unsuccessful medical therapy in 33 patients (47.8%), haemoptysis in 22 patients (31.9%), nondiagnostic lung mass in 9 patients (13.0%) and lung abscess in 5 patients (7.3%). The surgical procedures were lobectomy in 45 (65.2%) patients, pneumonectomy in 10 (14.5%) patients, bilobectomy in 8 (11.6%) patients, lobectomy plus segmentectomy in 3 (4.3%) patients and only segmentectomy in 3 (4.3%) patients. Morbidity rate was 14.5% and there was no perioperative mortality. The follow-up was possible in 60 patients, with an outcome reported as excellent in 44 (73.3%) patients, as improved in 11 (18.3%) and as unchanged in 5 (8.3%).
ConclusionAlthough the number of patients with bronchiectasis referred for surgical treatment has decreased, pulmonary resection still plays a significant role. Surgical resection of localized bronchiectasis is a safe procedure with proven improvement of quality of life for the majority of patients.
Bronchiectasis, originally described in 1819 by René Laënnec,1 is a suppurative lung disease with heterogeneous phenotypic features. The characteristic features consist of abnormal and irreversible dilation and distortion of the bronchi, which has numerous causes. In the pre-antibiotic era, it occurred frequently and it was an important cause of morbidity and mortality.2,3 Nowadays, there is a general belief that its incidence is falling due to improvements in health care in recent decades, especially in developed countries, although recent literature points out that the incidence of this pathology remains largely unknown or underestimated.2–8 The incidence varies widely (3.7–52/100,000 adults) between different studies, probably due to methodology and diagnostic technology availability differences.4,5 No recent population studies have been carried out in Portugal.
Generally, the vast majority of patients can be managed with conservative treatment, with surgical treatment being reserved for focal disease and when medical treatment is no longer effective. The concept behind surgical resection for bronchiectasis is to remove permanently damaged areas of the lung, with poor antibiotic penetration, and thus serve as microbiological reservoir leading to recurrent infections. Surgery for bronchiectasis currently still plays an important role in thoracic surgical practice in several countries, including Portugal.2,3 In order to evaluate the role of surgical treatment of bronchiectasis in our center, we reviewed our surgical experience and outcomes over the last 20 years.
Material and methodsBetween January 1994 and July 2014, 69 patients with bronchiectasis underwent pulmonary resection at cardiothoracic department of Centro Hospitalar de Vila Nova de Gaia/Espinho. Preoperative assessment included their clinical history, physical examination, lung function tests, chest radiography and CT scan. Fiberoptic bronchoscopy was performed in order to rule out any intraluminal pathology. Evaluated parameters were patient demographics, presenting symptoms, indications for surgical treatment, type of lung resection, perioperative morbidity and mortality, as well as clinical follow-up and outcomes.
Most patients were referred for surgery by their pulmonologist after long term medical treatment; the final decision for surgery being reached at a weekly medico-surgical meeting. Criteria for surgery included unsuccessful medical therapy with recurrent respiratory infections, persistent sputum production, chronic cough, persistent lung abscess or haemoptysis and localized bronchiectasis. Before surgery, all the patients underwent intensive respiratory physiotherapy, microbiology exam of respiratory secretions and antibiotic prophylaxis. A posterolateral thoracotomy was performed in all patients under general anaesthetic and orotracheal intubation with double lumen tube. Surgical resection aimed at minimizing the number of resected segments without compromising the objective of elimination of disease. Lobectomy was preferred if the disease was limited to one lobe, pneumectomy if widespread and segmentectomy when the disease did not affect the whole lobe or the lung function was mediocre. All resected specimens were subjected to histopathological examination to confirm diagnosis. Postoperative care included respiratory physiotherapy and antibiotic therapy. Perioperative mortality was defined as death within 30 days after surgery or during hospital stay. A lung function reevaluation was performed 6 months after surgery to assess its effect on respiratory capacity.
Follow-up information was obtained during outpatient clinic visits or by telephone interview at least one year after the surgery. The clinical outcome of surgery was assessed by asking the patients to describe their current status with respect to their preoperative status. This was classified as: excellent, complete absence of preoperative symptoms; improved, a marked reduction in preoperative symptoms; or unchanged, no improvement or worsening of preoperative symptoms.
Statistical analyses were carried out using Statistical Package for Social Sciences version 20. Functional results were compared using the paired t-test and/or Wilcoxon's rank test. A p value of less than 0.05 was considered significant.
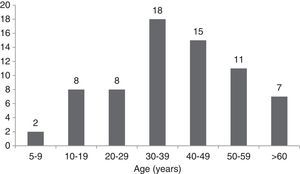
ResultsFrom the 69 patients included in our study, 51 (73.9%) were submitted to surgery during the first decade of our study (1994–2004). In terms of gender distribution, 31 (44.9%) patients were male and 38 (55.1%) patients were female. Ages ranged from 5 to 75 years, with a mean age of 38.6 years. The majority of patients were aged over 30 years old (Fig. 1). Twelve (17.4%) patients had a smoking history and sixteen (23.2%) had antecedents of pulmonary tuberculosis. Mean duration of symptoms was 4.5 year and included recurrent infections in 39 (56.5%) patients, persistent productive cough in 33 (47.8%) patients, haemoptysis in 29 (42%) patients and dyspnea on exertion in 11 (15.9%) patients. Pulmonary function tests were carried out before surgery: 7 (10.1%) patients had a restrictive defect and 3 (4.3%) patients had an obstructive defect.
Surgery was indicated because of unsuccessful medical therapy in 33 patients (47.8%), haemoptysis in 22 patients (31.9%), nondiagnostic lung mass in 9 patients (13.0%) and lung abscess in 5 patients (7.3%). The surgical procedures were lobectomy in 45 (65.2%) patients, pneumonectomy in 10 (14.5%) patients, bilobectomy in 8 (11.6%) patients, lobectomy plus segmentectomy in 3 (4.3%) patients and only segmentectomy in 3 (4.3%) patients. Complete operative details are given in Table 1. Median hospital stay was 7 days (from 4 to 40 days). Morbidity rate was 14.5%. The complications were: persistent air leak (>10 days) in 5 patients, rethoracotomy for haemorrhage in 2 patients, bronchial stump dehiscence with bronchopleural fistula, nosocomial pneumonia and atrial fibrillation in 1 patient each. There was no perioperative mortality. The results of postoperative respiratory function reevaluation are shown in Table 2. There were no significant differences between pre and postoperative data.
Patient surgical procedures.
| Procedure | n (%) |
|---|---|
| Pneumonectomy | |
| Left | 4 (5.8) |
| Right | 6 (8.7) |
| Lobectomy | |
| Right upper lobe | 9 (13.0) |
| Middle lobe | 9 (13.0) |
| Right lower lobe | 9 (13.0) |
| Left upper lobe | 4 (5.8) |
| Left lower lobe | 14 (20.3) |
| Bilobectomy | |
| Superior (Right upper lobe+middle lobe) | 3 (4.3) |
| Inferior (Right lower lobe+middle lobe) | 5 (7.2) |
| Lobectomy+segmentectomy | 3 (4.3) |
| Segmentectomy | 3 (4.3) |
Follow-up was possible in 60 (87%) patients. The clinical outcome was reported as excellent in 44 (73.3%) patients, as improved in 11 (18.3%) patients and as unchanged in 5 (8.3%) patients.
DiscussionThis retrospective study observed 69 patients who underwent surgical treatment for bronchiectasis. Our results show that surgical management of bronchiectasis is highly effective in symptom-control and, therefore, in improving quality of life in these patients. It represents a curative solution associated with low mortality and morbidity rates. Although there have not been any prospective randomized trials comparing the short and long term efficacy of surgical and medical treatment,6,9 current literature clearly states that the primary therapeutic goal for bronchiectasis patients must be optimal medical treatment.4–6 Appropriate antibiotic therapy, bronchodilators, and physiotherapy must therefore be part of any form of bronchiectasis treatment. Similar to other series, the majority of our patients had had recurrent respiratory infections in the past, which emphasizes the importance of appropriate medical treatment and management of these infections.2,8,10
More than 70% of our patients were submitted to surgery during the first decade of our two decade study period (1994–2004). This difference in the number of patients submitted to surgical treatment between the two decades might be explained by the fact that it was believed that the incidence of bronchiectasis within developed countries populations had decreased2–8 and then there was the renewed interest in this pathology with the validation of new structured approaches to bronchiectasis medical treatment, as recent publication of treatment reviews and management guidelines may prove.4–7,11
Bronchiectasis was more common on the lower lobes. It was thought that bronchiectasis would be more likely to affect the left lung, due to anatomical features of the left main bronchus (smaller diameter and greater angulation) that make it more prone to obstruction than the right one.2,6,10,12 However, as reported previously in a Portuguese study,2 we found a predominance of right lung involvement (43 patients; 62.3%). This greater involvement resulted mostly from a frequent partial or total involvement of the middle lobe in 27 (62.8%) patients, which is probably related to nonobstructive forms of middle lobe syndrome.2,13,14
Bilateral resection was not performed on patients in our study because of the numerous contraindications described for this procedure.15 Pneumonectomy is reported to be a high-risk procedure especially for benign disease, but it may become necessary in rare cases of unilateral presentation with one healthy lung.8,15,16 We have performed ten pneumonectomies with satisfactory results, especially for patients with a destroyed lung. There was no mortality and one patient had a rethoracotomy for haemorrhage.
Overall perioperative morbidity ranges from 9.4% to 24.6% depending on the series6,16 and therefore our result of 14.5% is acceptable. Bronchopleural fistula occurred in only 1 patient due to a bronchial stump dehiscence after a right lower lobe lobectomy and was resolved with conservative treatment. Although rare, the development of bronchopleural fistula is a source of significant morbidity, so it is important to avoid it whenever possible through adopting preventive measures, such as appropriate preoperative antimicrobial coverage, delaying surgery until there is no apparent mucosal inflammation in preoperative bronchofibroscopy and coverage of the stump during surgery.6,15,16
A normal pattern is usually found among pulmonary function tests of patients with bronchiectasis,2,3,8,17 although, depending on the extent of lung damage, a functional impairment might be found in these patients.3,6,10 We have found functional impairment in less than one sixth of our patients. Comparison between pre and postoperative function test values showed that surgery influenced neither FVC nor FEV1, despite parenchymal resection, which was as expected since the excised segments are diseased and do not contribute to pulmonary ventilation.2,3,8,17
At follow-up, 55 (91.7%) patients were found to have improved their clinical condition. Only one patient reported worsening in symptoms after surgery and four patients showed no symptomatic improvement. This degree of symptomatic control is in line with the available literature.2,3,6,10,12
ConclusionAlthough the number of patients with bronchiectasis referred to surgical treatment has decreased, pulmonary resection still has a significant role in this pathology. Surgical resection of localized bronchiectasis is a safe procedure with acceptable perioperative morbidity and mortality rates, and proven improvement of quality of life among the majority of patients.
Author contributionsDaniel Coutinho, Pedro Fernandes and Miguel Guerra conceived the project idea. Daniel Coutinho and Pedro Fernandes collected the data and conducted the analyses. All authors interpreted and discussed the results. Daniel Coutinho and Pedro Fernandes wrote the manuscript. All authors have read and approved the final version.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.