The authors present a clinical case of a 35-year-old patient who was diagnosed with intercostal artery-to-pulmonary artery fistula and review the literature of systemic-to-pulmonary fistulae based on radiological findings of an exceptional case report.
Os autores apresentam um caso clínico de um doente de 35 anos a quem foi efetuado o diagnóstico de fístula arterio-arterial sistémico-pulmonar e fazem uma revisão da literatura sobre fístulas arterio-arteriais sistémico-pulmonares baseado nos achados radiológicos de um caso excecional.
Arterial systemic-pulmonary fistulae are abnormal communications between aberrant or hypertrophic systemic arteries and pulmonary artery.1 This type of arterial malformations may occur between the pulmonary artery and the intercostal arteries, or internal mammary, bronchial, pericardial or esophageal arteries.2,3
Systemic-pulmonary arterial fistulae may be acquired, secondary to inflammatory/infectious events (for example: actynomicosis, tuberculosis), surgical procedures (post cardiothoracic or chest drainage tube procedures) or neoplasic causes. However, the young age in which some of the reported cases of these fistulae were detected, suggests that these may be rare congenital anomalies, with only described 20 cases of arterio-arterial fistulae from congenital etiology.2–6 Patients with this type of anomalies may present dyspnea, hemoptysis and/or symptoms of congestive heart failure or may be asymptomatic and usually when there are no symptoms, sometimes it is the presence of a hum or murmur in the cardiopulmonary auscultation that triggers imaging and diagnostic investigation. In this context, a chest X-ray may reveal changes such as rib notching or pulmonary infiltrate.7,8,5,3 Potential consequences of this kind of vascular fistulae include heart failure from volume overload, pulmonary hypertension and infectious complications and/or severe bleeding from rupture.3
The authors present a case report of a young male who, based on imaging findings, was diagnosed with an arterial fistula between intercostal arteries and pulmonary artery.
Case reportA Caucasian male of 35 years of age, and a construction worker, was admitted in the emergency room of our hospital with sudden dyspnea. There was no history of any other symptoms or signs of respiratory tract (such as hemoptysis) or cardiac system (palpitations). The patient mentioned prior sporadic episodes of sudden dyspnea and stated he was not taking any medication. There was no relevant personal or family medical background.
The patient denied smoking, alcoholic or drug habits and there was no history of previous admissions. Clinical evaluation of the patient revealed only discrete bronchospasm after pulmonary auscultation. A chest X-ray showed unilateral inferior rib notching of the 4–7th left ribs, inferior left lung hypotransparency and prominent vasculature (Figs. 1 and 2).
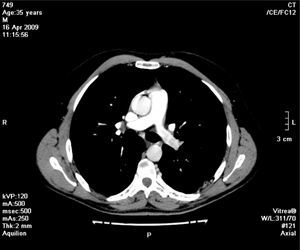
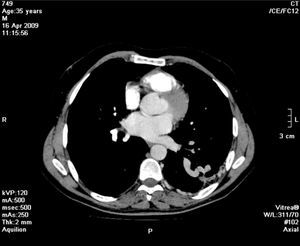
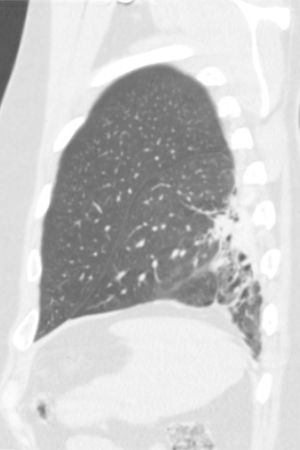
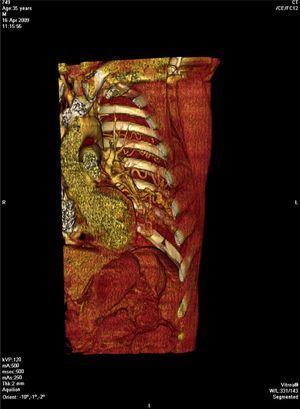
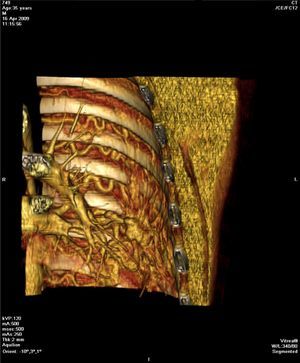
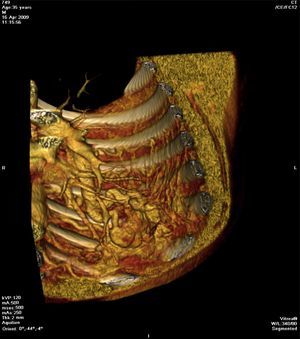
Angio-CT of the chest was performed and revealed relative reduction of enhancement of the left branch of the pulmonary artery (Fig. 3), homolateral dilatation and tortuosity of the intercostal arteries (Figs. 4, 6 and 7) with a tangle of arterial blood vessels (Fig. 8) (partially extrapleural, transpleural and intraparenchymal) draining to the left pulmonary artery. Adjacent lung parenchymal changes as traction bronchiectasis were also observed (Fig. 5). No CT signs of pulmonary hypertension were present and the caliber of the bronchial arteries was normal.
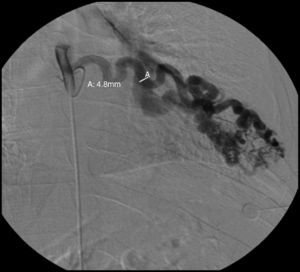
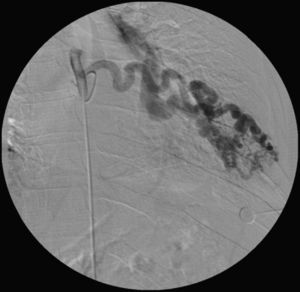
Selective arterial angiography of the 4–7th intercostal arteries was performed to confirm that the diagnosed vascular malformation was exclusively arterial (Figs. 9 and 10), demonstrating dilated intercostal arteries and an exclusive arterial fistula between left systemic and pulmonary arteries through a tangle of arterial blood vessels (Figs. 10 and 11). Bronchial arteries were not evaluated.
Image of the selective angiography of the 7th left intercostal artery demonstrating, besides the increased caliber and tortuositiy of the intercostal artery, an exclusive arterial fistulous connection between the systemic arterial circulation, via intercostal artery, and the left pulmonary artery.
During this evaluation time, the patient remained asymptomatic and a therapeutic approach (embolization versus surgical approach) has not yet been defined.
DiscussionClinical manifestations of the systemic-pulmonary arterial fistulae may be misinterpreted as patency of the ductus arterious or arterio-venous malformations and the symptoms depend, in part, on the functional repercussion that is proportional to the vessel size involved in the abnormal vascular anastomosis and heart distance.2,8 Chest X-ray in this type of vascular malformations demonstrates unilateral inferior rib notching and lung hypotransparency, suggesting pulmonary infiltrates and/or increased blood vessels (as in our case report).3
In the case reports described in the literature, systemic pulmonary arterial anastomosis typically are multiple and arterio-venous malformations may be present with cardiovascular consequences.3 In our case report, there is no radiological sign of cardiovascular consequence since ICT (cardiothoracic ratio) and the caliber of the common pulmonary artery are normal and the fistula is exclusively arterial, a finding that was angiographically confirmed by showing the arterial anastomosis between left intercostals arteries and left pulmonary artery.
As far as systemic-pulmonary arterial anastomosis is concerned, this case report represents an exceptional case, regarding the exuberance of the shunt, drainage pattern (exclusively arterial) and with no known functional consequences. Transcatheter arterial embolization or surgical resection may be considered as therapeutic approaches in this type of vascular malformations, however recurrences have been described in post-embolization procedure.1,3,6
ConclusionArterial systemic-pulmonary fistulae may present themselves via symptoms or may be asymptomatic and can be acquired or congenital. The authors describe an exceptional case of arterio-arterial fistula, remarkable for its radiological exuberance, type of malformation that is an exclusive arterial fistula between intercostal systemic arteries and pulmonary artery with no pulmonary arteriovenous communication. In our case, the presence of parenchymal abnormalities, such as bronchiectasis adjacent to the tangle of blood vessels, may suggest a history of previous inflammatory/infectious etiology.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Please cite this article as: Morais F, Almeida T, Campos P. Fístula arterio-arterial entre a artéria pulmonar e artérias intercostais – a propósito de um caso clínico de «unilateral rib notching». Rev Port Pneumol. 2014;20:167–171.