Health inequities are differences in the health status or the distribution of health resources between different population groups, arising from the social conditions in which people are born, grow, live, work and age.1 Such inequities have high social and economic costs for individuals and societies worldwide.1 Lower socioeconomic status is among the risk factors associated with worse health outcomes and leads to a higher rate of potentially preventable hospital admissions.2 This may reflect regional differences in access to healthcare (e.g., delays in access to secondary care) and primary care quality, which have been significantly associated with avoidable emergency admissions.3-5 This is especially important for chronic conditions in which proper management may avoid exacerbations,6,7 as is the case of asthma.8 There is evidence that people with asthma living in deprived areas may have impaired asthma outcomes across all stages of patient care, leading to a higher rate of hospitalizations and risk of asthma-related deaths.9,10 As health inequities have remained insufficiently studied in Portugal, in particular regarding access to care,11 we assessed whether such inequities may occur in Portugal as well, by studying the association between the region of residence and the frequency of asthma hospitalizations.
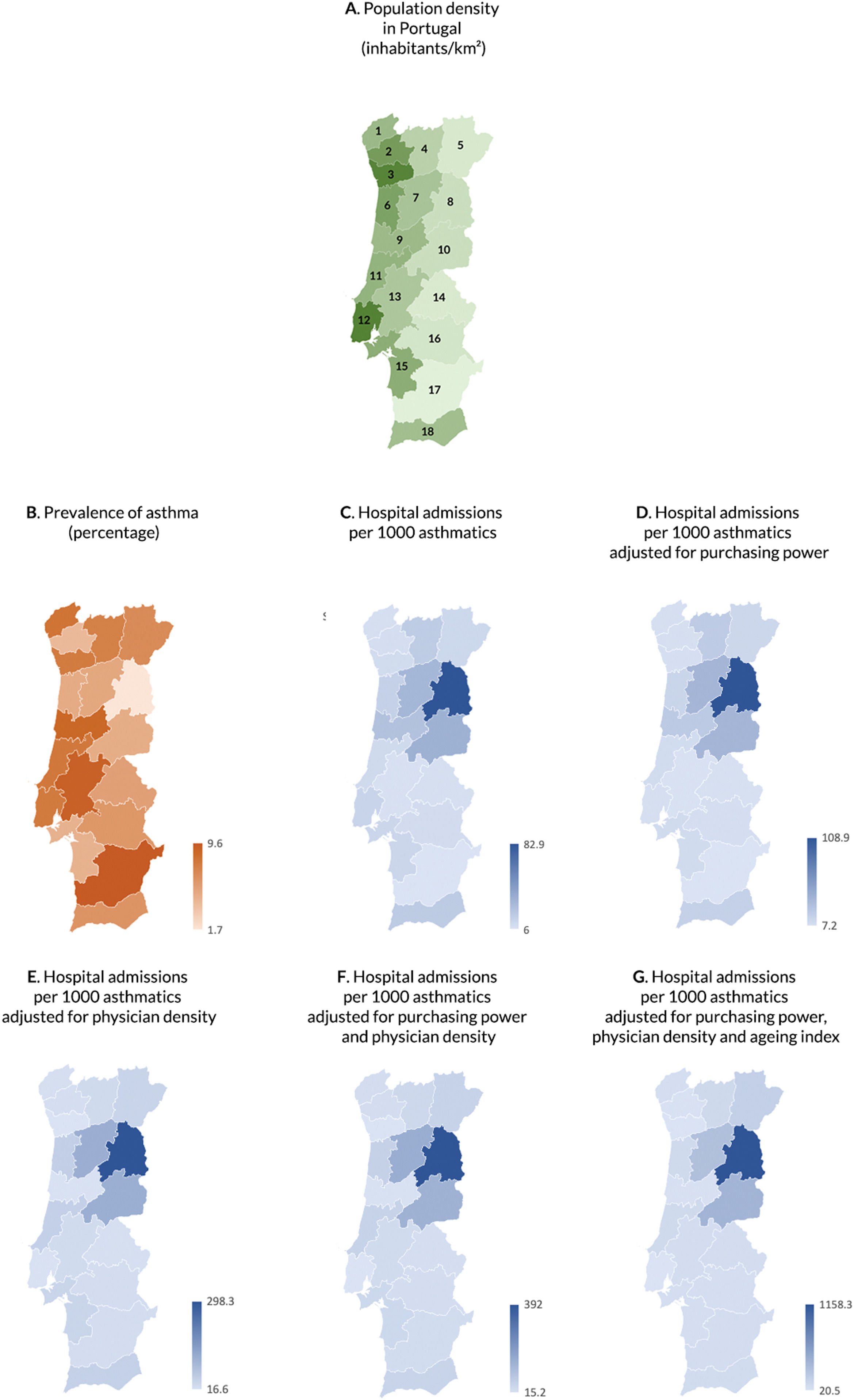
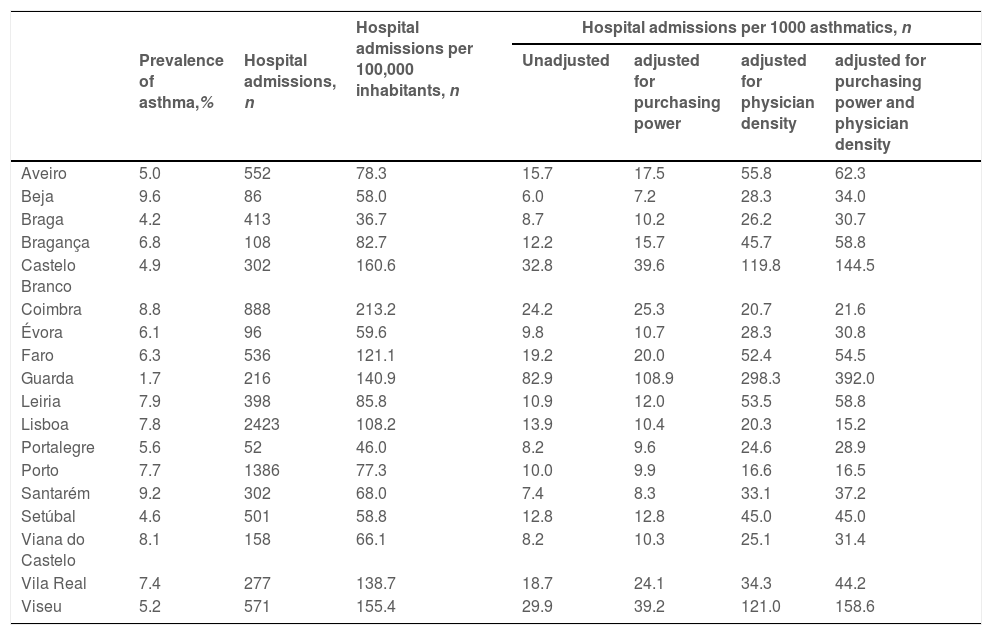
In mainland Portugal, between 2011 and 2015, there were 9161 asthma hospitalizations in adults, according to data from the national administrative database containing all hospitalizations in public hospitals from mainland Portugal (ICD-9-CM code 493.x). Therefore, there was an average of 92.6 hospital admissions per 100,000 inhabitants and 13.5 hospital admissions per 1000 inhabitants with asthma. Mainland Portugal is composed of 18 districts (Fig. 1A). The districts with the highest rates of asthma hospital admissions per 100,000 inhabitants were Coimbra (213.2 hospitalizations per 100,000 inhabitants), Castelo Branco (160.6/100,000), Viseu (155.4/100,000) and Guarda (140.9/100,000), all of which are in the center region of Portugal and are (except for Coimbra) inland districts. Taking into account the prevalence data from the most recent Portuguese epidemiological survey carried out in 201012 (Fig. 1B), the three districts with the most prevalence-adjusted asthma hospital admissions were Guarda (82.9 hospitalisations per 1000 inhabitants with asthma), Castelo Branco (32.8/1000), and Viseu (29.9/1000). All these three districts have a low urban coverage. Importantly, Coimbra, an urban district in coastal Portugal, is not among the districts with the highest rate of prevalence-adjusted hospital admissions, despite being among the districts displaying the highest crude hospitalization rate for asthma.
Data on (A) population density per district in mainland Portugal (1 — Viana do Castelo, 2 — Braga, 3 — Porto, 4 — Vila Real, 5 — Bragança, 6 — Aveiro, 7 — Viseu, 8 — Guarda, 9 — Coimbra, 10 — Castelo Branco, 11 — Leiria, 12 — Lisboa, 13 — Santarém, 14 — Portalegre, 15 — Setúbal, 16 — Évora, 17 — Beja, 18 — Faro); (B) asthma prevalence in mainland Portugal (percentage), and on asthma hospital admissions in mainland Portugal (C) per 1000 patients with asthma; (D) per 1000 patients with asthma and adjusted for a purchasing power of 100% per capita; (E) per 1000 patients with asthma and adjusted for a standard population with 1000 physicians per 100,000 inhabitants; (F) per 1000 patients with asthma and adjusted for a purchasing power of 100% per capita and a standard population with 1000 physicians per 100,000 inhabitants; and (G) per 1000 patients with asthma and adjusted for a purchasing power of 100% per capita and a standard population with 1000 physicians per 100,000 inhabitants and an aging index of 100.
The inland regions of Portugal are, on average, less urbanized than its coastal regions,13 and Guarda, Viseu and Castelo Branco are among the districts with the least purchasing power (according to data from the National Institute of Statistics14 and defined according to its published definition15), so it is possible that such results could be partially explained by socioeconomic disadvantage. It is also known that the population in inland Portugal is, on average, older than its coastal counterpart. Guarda and Castelo Branco are in the top three districts with the highest aging index (proportion of inhabitants aged 65 years or older relative to those younger than 15 years older) in Portugal.16 Several comorbidities are associated with asthma in the elderly, which may complicate asthma management in these patients.17 Older age is also associated with lower literacy, which may hinder adherence to treatment in chronic diseases in elderly people.18 As a result, differences in age distribution between districts in mainland Portugal may partially explain the differences in hospital admissions for asthma. Additionally, according to data from the Portuguese Medical Association, districts in inland Portugal, especially Guarda and Castelo Branco, are also among those with fewer registered physicians per 100,000 inhabitants.19
Nevertheless, even when adjusting for purchasing power, aging index and density of registered physicians in Portuguese districts, these three districts still showed the highest number of prevalence-adjusted asthma hospital admissions (Fig. 1D-F; Table 1). This suggests potential regional health inequities that are not solely explained by factors such as age and purchasing power and may reflect the ongoing asthma management available/provided in different regions. This suggests that inequities in access to healthcare services may hinder asthma management in these inland districts. The results of this study may be a model to be implemented in other underserved populations in Europe and globally.
Prevalence of asthma and hospital admissions for asthma per district of mainland Portugal.
Early asthma diagnosis and vigilant control are crucial to prevent asthma exacerbations and reduce the healthcare burden. Initiatives in Finland, Poland and Brazil have shown that prioritizing asthma care and placing primary care at the center of asthma care reduce both asthma morbidity and mortality.20,21 However, the Global Initiative for Asthma (GINA) guidelines have primarily been developed and tailored by tertiary care physicians and may be challenging to implement in primary care, particularly when physicians’ density is low.22-24 More easy-to-implement and patient-centered care pathways for asthma, including all health care professionals, are needed. Additionally, as medication adherence in asthma tends to be poor,25 tailored, integrated and transdisciplinary approaches to raise asthma literacy in disfavored regions could increase adherence to medication by patients. Moreover, digital solutions may be of use to improve asthma care, especially for regions with suboptimal access to healthcare services. Telemedicine may facilitate access to asthma clinical reviews and allow for remote patient monitoring, thus preventing exacerbations.26 Emerging technologies, such as monitoring devices and mobile apps, may further improve asthma care. The potential of mobile apps for patient-centered care has been previously shown for allergic rhinitis27, and there are reasons to believe such may apply to asthma care as well.28 Apps may therefore provide information on asthma-related triggers, such as pollen season and pollution, and feedback from mobile apps may be used by the patient and the physician to improve asthma management.29
In conclusion, our results suggest the existence of health inequities in asthma management in mainland Portugal and an urgent call for action from policy makers. This issue is surmounted as depopulation and aging are increasing in rural areas of Europe.30 Complementary to the traditional Health Service approaches, in these regions, digitally-enabled, patient-centered care may contribute to reducing asthma burden and hospitalizations, as well as health inequities in this population.
Funding sourcesThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
None.