Pyoderma gangrenosum (PG) is an ulcerative neutrophilic dermatosis of uncertain aetiology that is generally found in the extremities. It usually presents as painful skin ulcers.
We present a case of a patient with atypical PG that was satisfactorily treated using negative pressure wound therapy (NPWT) and immunosupresor therapy.
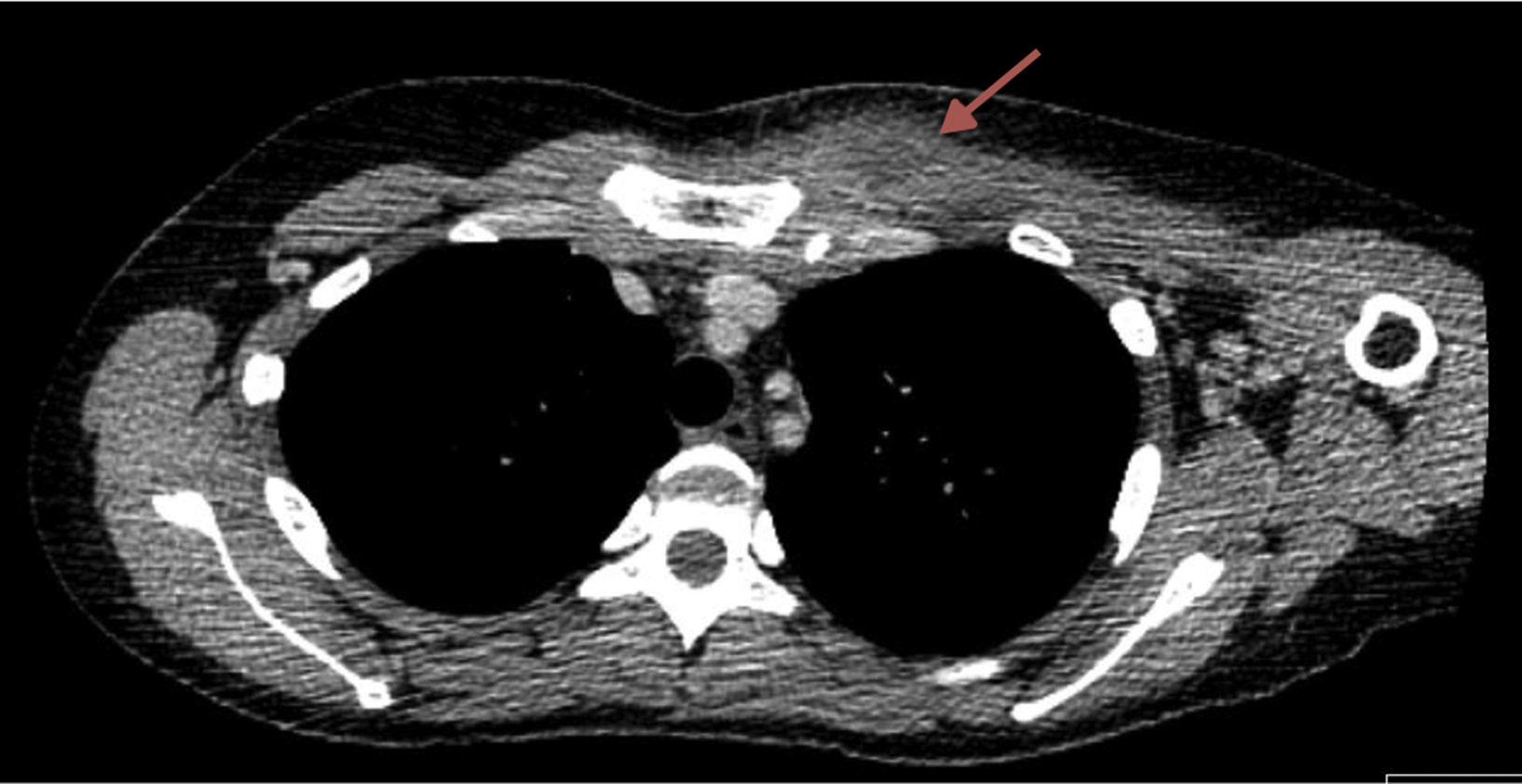
A 35-year-old female with inflammatory intestinal disease and a history of PG in lower extremities during pregnancy, was sent to our institution for pain and swelling at paraesternal level of 3 days of evolution without previous traumatism of the region. We performed a chest CT scan that revealed the presence of an erosive arthropathy of the left sternoclavicular joint; with a lesion of 30mm in the thickness of the ipsilateral pectoral musculature related to an abscess (Fig. 1). We punctured the lesion under ultrasound control. This revealed purulent material, which we later drained, before wide debridement of the abscess and starting empirical antibiotic treatment.
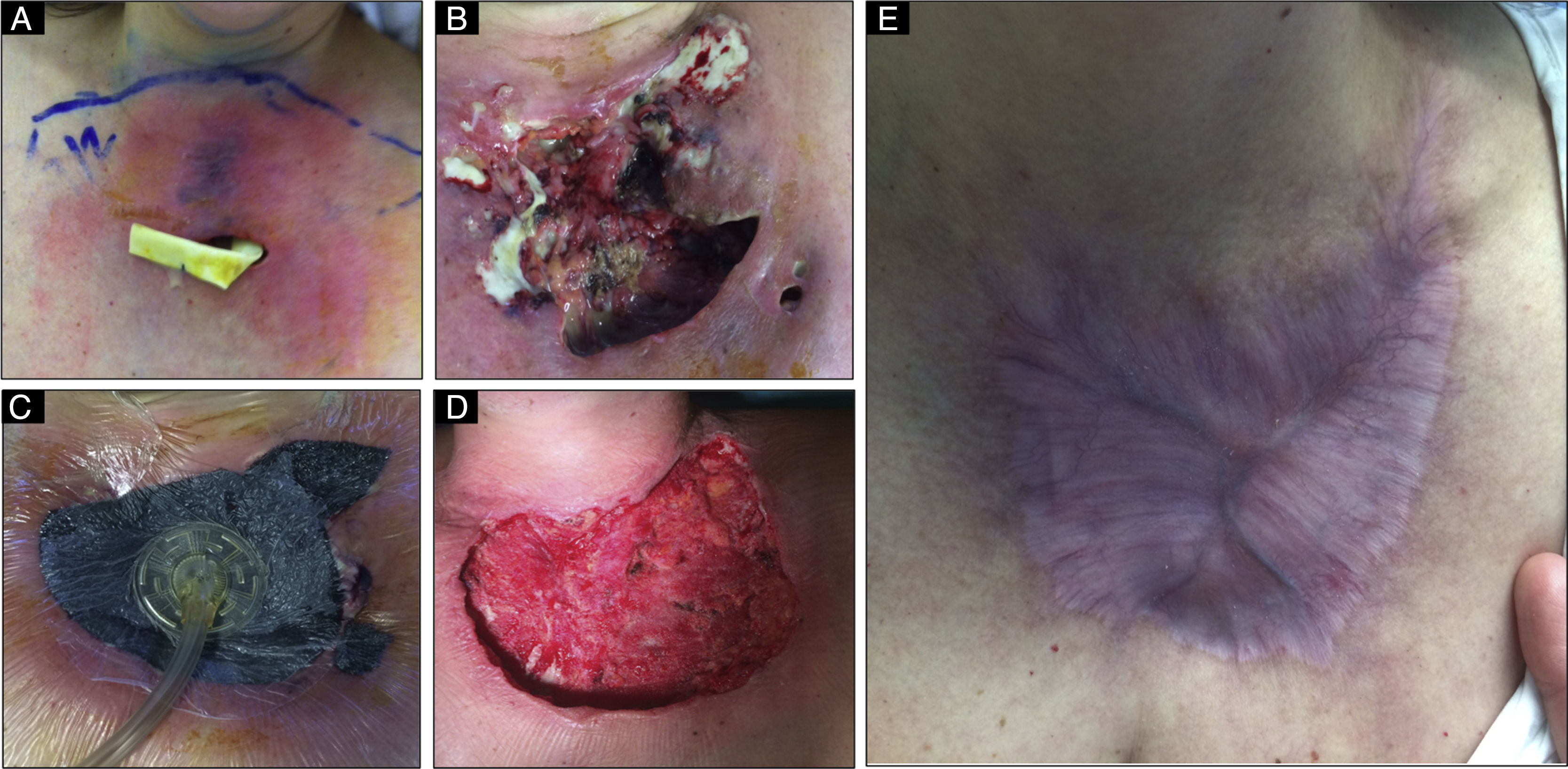
Over the days following the drainage, the patient's evolution was negative with a large increase in purulent exudate from the wound, fever and signs of sepsis with progression of the ulcer (Fig. 2A and B).
Different evolutionary stages of the disease. (A, B) Rapidly progressive ulcer with abundant purulent exudate. (C) Application of the system of negative aspiration (NPWT) on the ulcer bed. (D) Result after 7 days using the NPWT system and immunosuppression, where we can observe the disappearance of the exudate and the emergence of granulation tissue. (E) 6 months after onset we can observe that the lesion is fully healed.
All the microbiological cultures were negative, so as we suspected PG, a tissue sample was sent for a histopathological study.
In view of the fact that the wound was clearly worsening, combined with the impossibility of controlling the exudate we decided to place a NPWT system, combined with intensive immunosupresor therapy and broad-spectrum antibiotics (Fig. 2C).
Seven days after starting treatment with NPWT the exudate was controlled and the ulcer had stabilised, with granulated tissue appearing at the back of the wound (Fig. 2D). Thus the NPWT system was removed to prevent the growth of ulcer secondary to pathergy that could cause the NPWT system.
Finally the histopathological study of the tissue sample demonstrated central necrosis and ulceration of the epidermis and dermis surrounded by an intense acute inflammatory cell infiltrate, with a peripheral mixed to chronic inflammatory cell infiltrate. We also looked for neutrophils and fibrin in superficial vessels without histologic evidence of vasculitis. All of these findings were PG-compatible features.
The patient's evolution was finally successful, and complete healing of the ulcer achieved 4 months after onset of symptoms (Fig. 2E).
Pyoderma gangrenosum is a neutrophilic dermatosis, which was first described by Brocq in 1916 and later named by Brunsting in 1930, which is characterised by papules, pustules or vesicles in the skin that quickly transform into a painful ulcer with violet, raised and up to 20cm diameter margins.
PG has an incidence of 0.3–1/100,000 and typically affects middle-aged patients. Four clinical variants of PG have been described: the ulcerative, pustular, bullous and vegetative type. In 80–90% of patients the lesions are reported in the lower limbs, though they may be seen in any part of the human topography, as was the case of our patient who had had a first episode of PG in lower limbs and a recurrence years later in the chest.1
The diagnosis of PG, as in our case, is usually reached by exclusion, although frequently the typical morphology of the injury will lead us to suspect its presence. There is no specific treatment and PG management consists of suppression of the inflammatory activity, treatment of the underlying disease, the promotion of ulcer healing and pain control.
In 2006, Niezgoda and cols. described the use of NPWT systems in managing PG for the first time. Nevertheless, there is still currently some controversy about the use of these systems in some wounds, such as those produced by PG where any traumatic handling of the wound can lead to worsening, a phenomenon termed pathergy, especially when the treatment is performed without suitable immunosuppression of the patient.2 This controversy exists even in vitro and in vivo studies. It has been shown that NPWT applied to a wound helps the healing of the wound since it reduces oedema, favours the emergence of granulation tissue, increases tissue perfusion and cleans the exudate from the wound, thus reducing the local bacterial load. Therefore, NPWT can become a valid alternative therapy.3,4 In this way, as in our case, initial use of NPWT combined with suitable immunosuppression was a reliable system for treating PG of difficult clinical management, and produced a satisfactory evolution. Although there are few long series in the literature to prove it, NPWT could become another valid pillar in treating PG in the future.2–4
In conclusion we present a PG case with an atypical presentation simulating an abscess of the pectoral muscle, which caused a delay in diagnosis and therefore in deciding on the immunosupressive treatment. As described above, the consequence was that the ulcer got worse and it was necessary to use a NPWT system associated with corticotherapy treatment to finally obtain a satisfactory evolution.
Conflicts of interestThe authors have no conflicts of interest to declare.