It is well established that exercise improves physical fitness without any adverse effects on asthma control.1,2 Asthma patients present lower levels of physical fitness and cardiopulmonary conditioning than their peers.1 Low physical activity levels are associated with more symptoms, a higher risk of exacerbations and a lower health related quality of life in asthma patients.2
Physical exercise improves cardio-pulmonary fitness, muscle trophism, muscle vascularization, and muscle ability to extract/use oxygen, resulting in a lowering of respiratory rate during activity.1 With a lower respiratory rate during activity, bronchoconstriction during exercise becomes less likely.1,3 Recent studies have also identified that regular exercise resulted in a reduction of airway inflammation, which in turn improved bronchioles patency.4
Although pulmonary rehabilitation programs have a well established role in chronic obstructive pulmonary disease treatment,5,6 studies about pulmonary rehabilitation effects on asthma patients are sparse.
A retrospective study was performed in order to assess the effect of a supervised pulmonary rehabilitation program on asthma symptoms (dyspnea), functional capacity and health related quality of life in adult asthma patients.
The intervention consisted of a pulmonary rehabilitation program with medical supervision. All asthma patients admitted to the pulmonary rehabilitation program between 2010 January and 2016 July were included.
The rehabilitation program lasted 8–12 weeks and was held twice a week. Each session had a duration of 1h and included a warm up period with breathing pattern re-education exercises, aerobic training (bicycle or treadmill during 30min), muscle strengthening of the main muscle groups and stretching exercises afterwards. The aerobic training intensity was gradually increased in order to reach an exertion perceived as moderate (evaluated as 11–13 at Borg scale) and/or dyspnea perceived as moderate (evaluated as 3–4 at modified Borg scale). Muscular strengthening consisted of one set of 12 repetitions (60–70% of one-repetition maximum) in each muscular group.
The 6min walk test (6MWT) was performed to evaluate functional capacity. To assess dyspnea, modified Borg dyspnea scale after 6MWT and Medical Research Council Dyspnea Scale (MRC-Dyspnea Scale) were used. Health-related quality of life was assessed through the Saint George Respiratory Questionnaire (SGRQ) and the Euro Quality of Life 5 Dimensional Questionnaire.
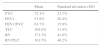
14 patients were included. 66.7% were females and the mean age was 50.8 years (SD=14.2). 14.3% of the patients were former smokers, the remaining were non-smokers. A description of pulmonary function tests is presented (Table 1).
All patients included presented severe asthma, according to the Global Initiative for Asthma (GINA) model of assessment of asthma severity in clinical practice.7 All patients presented stable controlled disease.
We did not observe any asthma exacerbation during exercise, and none of the patients needed medical intervention during rehabilitation sessions.
Prior to the intervention, patients walked on average 411.45 meters (SD=74.9m) in 6MWT. After the intervention, they walked on average 457.27 meters (SD=66.2m). Paired t-test was −1.97 (p=0.07) and a mean increase of 45m was observed. Although 45m represent an important clinical effect, the results did not reach statistical significance (p=0.07).
The asthma symptom evaluated in this study was dyspnea during activity, since that is the symptom that defines the need for asthma patients referral to pulmonary rehabilitation according to the British Thoracic Society guidelines.5 At the end of the intervention, there was a statistically significant improvement in dyspnea assessed with modified Borg dyspnea scale at 6MWT (paired t-test=2.83; p=0.017). The mean difference was minus 1.27 points.
An improvement was also observed in MRC-Dyspnea Scale, however it did not reach statistical significance (paired t-test=2.21; p=0.051). A mean difference of minus 0.55 points was observed.
Our results also presented a small improvement of 1.5 points on Euro Quality of Life 5 Dimensional Questionnaire and 3.36 points on SGRQ which did not reach statistical significance (paired t-test=2.19, p=0.053 and paired t-test 0.89, p=0.39 respectively).
This study adds to the growing evidence that supports the beneficial role of pulmonary rehabilitation in asthma patients.
The pulmonary rehabilitation program resulted in an improvement in dyspnea with statistical significance in adult asthma patients. Although a tendency toward improvement in functional capacity and health related quality of life was observed, the obtained results did not reach statistical significance.
Further studies with larger sample sizes and prospective designs are needed in order to ascertain the exact value of these findings.
Conflicts of interestThe authors have no conflicts of interest to declare.