There are barriers to providing pulmonary rehabilitation for chronic obstructive pulmonary disease (COPD) such as the high number of patients, difficult access to health facilities and high costs of programs. Pedometers can monitor and improve physical activity (PA). The aim of this study was to evaluate benefits and costs of home pedometer assisted PA, as compared to a standard outpatient supervised exercise training program in patients with COPD.
MethodsPatients were randomly assigned either to home pedometer assisted PA (Group 1), or to a six-week outpatient standard supervised exercise training program (Group 2). Patients of Group 1 had to walk at home for 6 weeks, at least 30min daily at the fastest step pace as possible, to achieve a weekly 10% increase in their average daily steps up to more than 6500. Pre and post programs we assessed: the six minute walking distance (6MWT: primary outcome), daily steps count, the Medical Research Council scale (MRC), the COPD assessment test score, and the BODE index (body-mass index, airflow obstruction, dyspnea, exercise capacity). Costs of programs were also evaluated.
ResultsOut of 40 patients, 18 in both groups (mean (standard deviation)) age: 68.3 (6.7) and 61.2 (6.7) years; FEV1: 1.1 (0.5) and 0.9 (0.4) liters in Group 1 and 2 respectively completed the study. At the end of the program 44.5% patients of Group 1 had reached the target daily steps, in 26.6 (9.5) days. Following the programs, both groups showed significant improvements in all outcome measures, except BODE. The home program was cheaper (p=0.0001), with a mean 76.3 euros saving per patient.
ConclusionHome pedometer assisted PA may be a useful and cheaper alternative to outpatient supervised exercise training programs in patients with COPD.
Total tobacco-attributable deaths including those due to chronic obstructive pulmonary disease (COPD), a leading cause of mortality and morbidity worldwide are projected to rise from 5.4 million in 2005 to 8.3 million in 2030.1–4 Prevalence and mortality rate are forecasted to increase due to the increasing number of smokers.2–6
Higher physical activity (PA) is associated with lower risk of mortality and cardiovascular events in individuals from low-, middle-, and high-income countries.7 Daily PA of patients with COPD is reduced in the early phases of disease as compared to healthy age-matched controls8 and worsen over time, with important clinical consequences.9 In these patients pulmonary rehabilitation improves symptoms, exercise capacity and health-related quality of life (HRQL),10,11 although the observed benefits do not consistently translate into enhanced PA levels.12 As a consequence guidelines for management of COPD suggest that pulmonary rehabilitation including exercise training should be provided to the vast majority of patients.1
In many countries, there are barriers to hospital based inpatient and outpatient supervised exercise training programs, such as a high number of patients, transportation, program costs, and geographical obstacles.13 A home program consisting of 3 weekly sessions for 8 weeks of aerobic leg cycling and strength exercises was a useful, equivalent alternative to outpatient rehabilitation for patients with COPD.14 Also tele-rehabilitation programs may be potentially useful to deliver and to maintain the benefits in difficult-to-reach areas.15,16
The daily steps and activity time were proven to be the most valid measurement of PA17,18 and their regular monitoring may benefit patients with COPD in achieving the effective daily PA.18 Pedometers have greatly advanced in recent years, providing daily step estimates,18 and smartphones with miniaturized accelerometre apps measuring PA are universal, widespread technologies which many patients with COPD may not use as they probably should.
We hypothesized that a home pedometer assisted program to incentivize PA might be an alternative to hospital based outpatient exercise training programs, especially in the context of regional asymmetries and difficult access to health facilities (as is the case of Indonesia with a 4.5% COPD prevalence,5 and a population of about 260 million – about 35 million living in Central Jawa, the others living on more than 17000 islands with limited access to health services19). The aim of this study was to evaluate the effect on exercise capacity, PA, dyspnea, and health status as well as costs of home pedometer assisted PA, as compared to a standard outpatient supervised exercise training program in patients with COPD.
MethodsStudy designThis was a randomized clinical trial (RCT). During the first week, all patients were taught how to use pedometers in three face to face sessions with a researcher checking patients’ ability to use the device properly. After the training week, subjects were randomly assigned to two groups: the Study Group (Group 1) received an unsupervised home pedometer assisted PA program, the Control Group (Group 2) received a hospital based outpatient supervised exercise training program. Researchers evaluating results and patients were not blind to treatment. Patients maintained their usual drug medication during the entire study.
The study was performed according to the Helsinki Declaration and approved by the Ethics Committee of Dr. Moewardi Hospital, Surakarta, Central Jawa, Indonesia (Reference: 799/IX/HREC/2016). Written informed consent to participate was obtained from all participants.
Study participantsStable patients suffering from COPD as defined by the Global Initiative for Chronic Obstructive Pulmonary Disease (GOLD) guidelines,1 40–75 years old, were consecutively recruited from the outpatient clinic of Dr. Moewardi Hospital, Surakarta, Central Jawa, Indonesia, between October 2016 and January 2017. Patients were enrolled if in a stable clinical condition (no exacerbation in the 4 weeks prior to study). The exclusion criteria were refusal to participate, participation in a pulmonary rehabilitation program during the previous 6 months, and severe concomitant comorbidities such as ischemic cardiac disease, chronic heart failure, orthopedic and/or neuromuscular diseases interfering with their ability to walk.
Study proceduresPatients of Group 1 received a pedometer (Omron HJ 321, Omron Healthcare Co Ltd, Kyoto, Japan) with the task of walking at home for 6 weeks. They were instructed to record the number of daily steps in their activity log books, along with information on any change in their clinical conditions. They were also asked to walk at home at the fastest step pace as possible, for at least 30min every day, for up to 6 weeks, with the task of achieving a weekly 10% increase in their average daily steps eventually reaching more than 6500 daily steps. Doctors checked both the patients’ pedometers and activity logbooks during weekly meetings at patients’ homes and every two weeks during the meetings at outpatient clinic. On the basis of pedometer daily step count and activity logbook checks, doctors prescribed the target step count for the following week.
Group 2 patients received three 30-min weekly sessions for six weeks of supervised standard exercise training on a treadmill at outpatient clinics. Doctors and nurses supervised the sessions. Initial treadmill speed was set at 80% of their theoretical speed during the six minute walking test (6MWT) performed at admission and calculated as described below, at 0 inclination. Depending on patient tolerance, the treadmill speed could be increased by 0.1km/h at each session. Patients were also encouraged to be more active at home and to walk for at least 30min daily without any supervision. They also were instructed to fill in their activity log books which were checked by doctors every week. Also these patients were given a pedometer on the day before the first session and the day after the last session in order to record the daily steps.
MeasurementsAt admission the following data and measurements were recorded:
- •
Demographics and anthropometrics, time of first diagnosis, drug therapy.
- •
Dynamic lung volumes, assessed after bronchodilation and expressed as absolute and percent of predicted values according to the Pneumomobile Project Indonesia.20
Before and after the programs, the following parameters were assessed in all patients:
- •
Exercise tolerance by means of the 6MWT.21 The best of two consecutive performances (2-h apart) conducted in a 30-m long and 3-m wide corridor under quiet conditions and without distractive stimuli was recorded for analysis. The Minimum Clinically Important Difference (MCID) of 6MWT following exercise training in moderate to severe COPD was recently reported to be at least a 30m increase.21 The distance walked in 6MWT was also expressed as “theoretical” speed (km/h) multiplying meters×10.
- •
Physical activity was measured as daily steps, based on an average step count of 7 days obtained using the same pedometer given to patients at their baseline visit. The MCID for PA has been reported to be 600–1100 daily steps.22
- •
The subjective sensation of breathlessness was evaluated by means of the Medical Research Council (MRC) scale.23 One point change in the scale is considered the MCID for this outcome measure.24
- •
The perceived health status was assessed by the Indonesian Version of the COPD Assessment Test (CAT) score.25,26 The MCID for CAT score is reported to be 2 points.27
- •
The composite and multidimensional BODE (body-mass index, airflow obstruction, dyspnea, and exercise capacity) index was calculated for each patient.28 It has been shown that for every point increase in the BODE there is a corresponding increase in mortality.29
Costs of programs per patient were assessed according to a modified calculation proposed by Goldstein et al.30 and gathered from the hospital financial department staff. The following costs were identified: pedometer, doctor consultations and doctor/nurse supervisions during exercise training, services, and medication. Transportation costs of patients and professionals to and from the hospital were calculated as follows: bus ticket cost, multiplied by the number of patients’ hospital and professionals’ home visits. Costs of exacerbations, hospital admissions and unscheduled medical visits were not included.
Statistical analysisThe primary outcome measure was the 6MWT. Results are shown as mean (Standard Deviation: SD) for continuous and as numbers (percentage frequency) for discrete variables. MRC and BODE are shown as median (interquartile range), whereas the number of steps are presented as mean (SD) as normally distributed.
To determine the sample size, an earlier study31 showed a post-program 70.4 (18.3) meter mean increase in 6MWT. The study hypothesis was therefore to observe a 30m post-PRP change in both groups. To obtain a 90% study power and an alpha error less than 5%, a minimum sample size of 12 patients completing the study was required in each Group. To obtain this result we estimated an allocation sample size of 40 patients, considering a 20% drop out rate.
Unpaired t test, Kruskall–Wallis H test, and χ2 analyses for dichotomous variables were used when appropriate for comparison between groups to test any baseline difference. The two-way repeated measures ANOVA was carried out to compare the improvements of both groups. Chi-square test was used to compare continuous and categorical variables. A p value less than 0.05 was considered as statistically significant.
Analyses were performed using a specific package (SPSS for Windows latest version, Chicago, Illinois, USA).
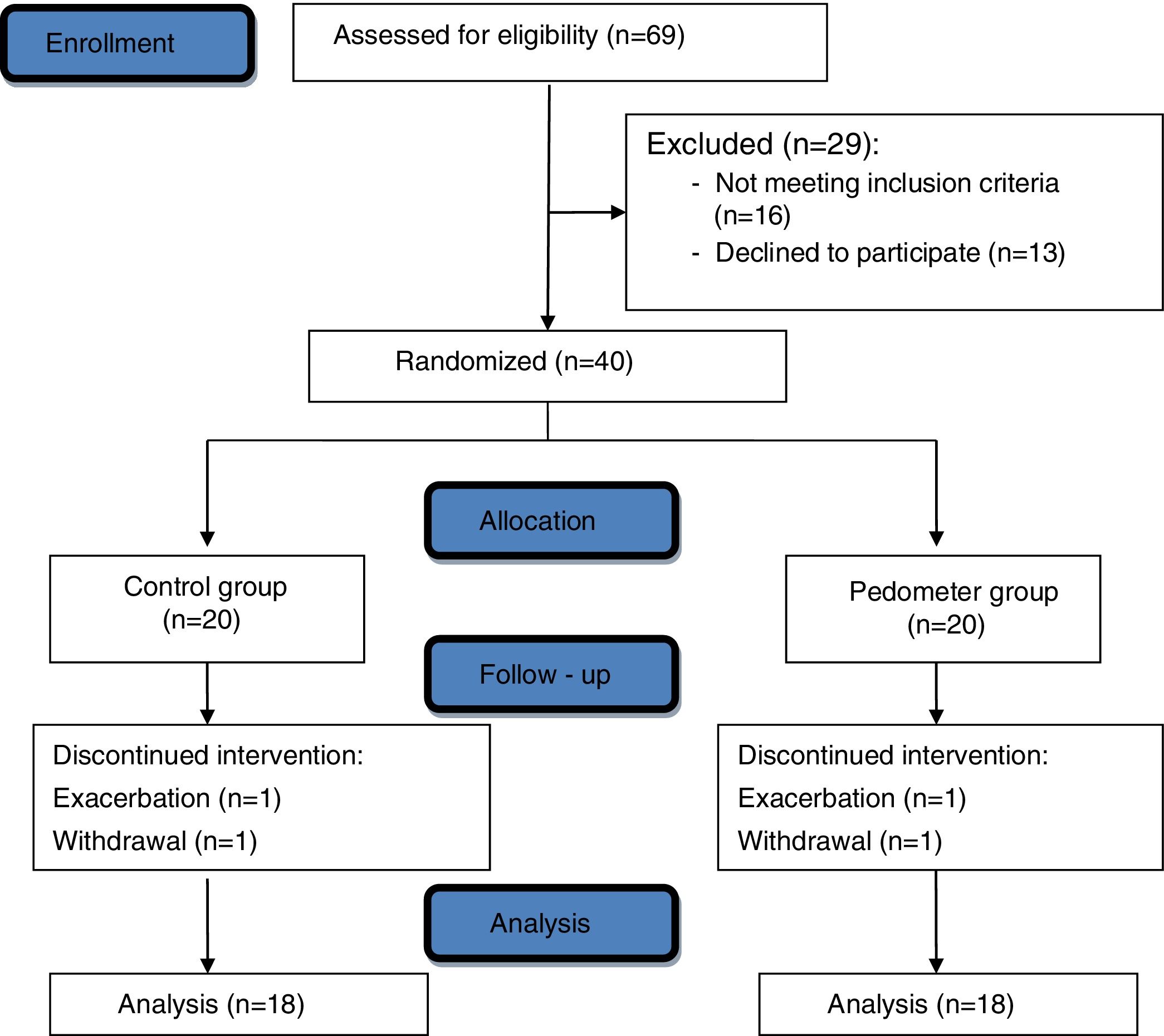
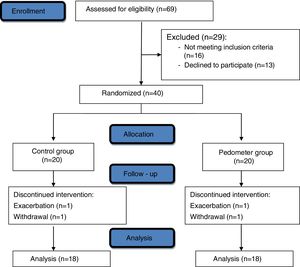
ResultsFig. 1 shows the Consolidated Standards of Reporting Tables (CONSORT) diagram of the study. Out of 40 patients recruited, 18 patients in each group completed the study. Two patients were excluded due to an exacerbation, one patient withdrew his consent, and one patient dropped out due to a motorcycle crash.
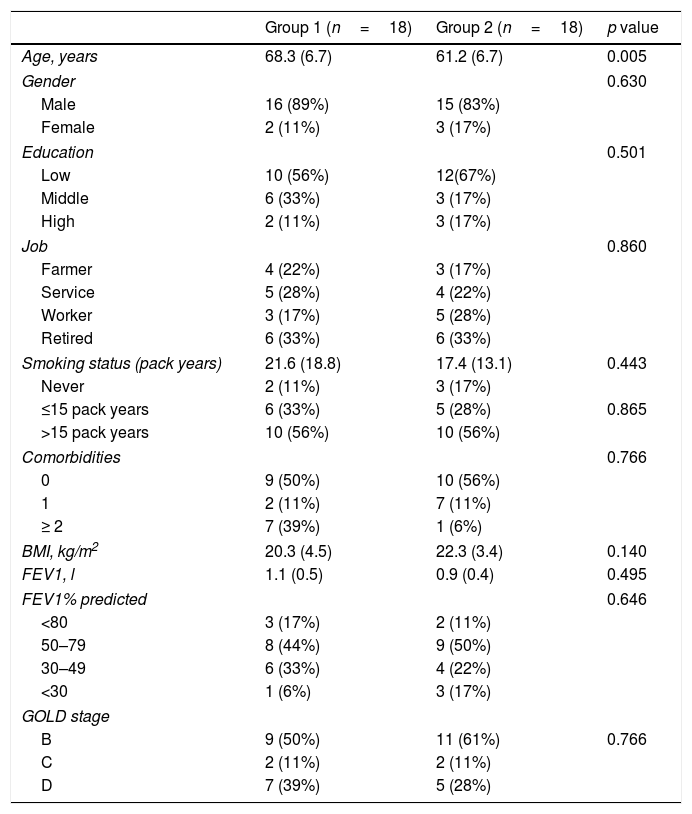
Table 1 shows the demographic, anthropometric, physiological and clinical characteristics of the patients. The two groups were not different for any characteristic except for the older age in Group 1 patients.
Demographic, antropometric, physiological and clinical characteristics.
| Group 1 (n=18) | Group 2 (n=18) | p value | |
|---|---|---|---|
| Age, years | 68.3 (6.7) | 61.2 (6.7) | 0.005 |
| Gender | 0.630 | ||
| Male | 16 (89%) | 15 (83%) | |
| Female | 2 (11%) | 3 (17%) | |
| Education | 0.501 | ||
| Low | 10 (56%) | 12(67%) | |
| Middle | 6 (33%) | 3 (17%) | |
| High | 2 (11%) | 3 (17%) | |
| Job | 0.860 | ||
| Farmer | 4 (22%) | 3 (17%) | |
| Service | 5 (28%) | 4 (22%) | |
| Worker | 3 (17%) | 5 (28%) | |
| Retired | 6 (33%) | 6 (33%) | |
| Smoking status (pack years) | 21.6 (18.8) | 17.4 (13.1) | 0.443 |
| Never | 2 (11%) | 3 (17%) | |
| ≤15 pack years | 6 (33%) | 5 (28%) | 0.865 |
| >15 pack years | 10 (56%) | 10 (56%) | |
| Comorbidities | 0.766 | ||
| 0 | 9 (50%) | 10 (56%) | |
| 1 | 2 (11%) | 7 (11%) | |
| ≥ 2 | 7 (39%) | 1 (6%) | |
| BMI, kg/m2 | 20.3 (4.5) | 22.3 (3.4) | 0.140 |
| FEV1, l | 1.1 (0.5) | 0.9 (0.4) | 0.495 |
| FEV1% predicted | 0.646 | ||
| <80 | 3 (17%) | 2 (11%) | |
| 50–79 | 8 (44%) | 9 (50%) | |
| 30–49 | 6 (33%) | 4 (22%) | |
| <30 | 1 (6%) | 3 (17%) | |
| GOLD stage | |||
| B | 9 (50%) | 11 (61%) | 0.766 |
| C | 2 (11%) | 2 (11%) | |
| D | 7 (39%) | 5 (28%) | |
Data are presented as mean (SD) or n (%), unless otherwise stated.
BMI, Body-mass index; FEV1, Forced Expiratory Volume at one second; GOLD, Global Initiative for Chronic Obstructive Pulmonary Disease.
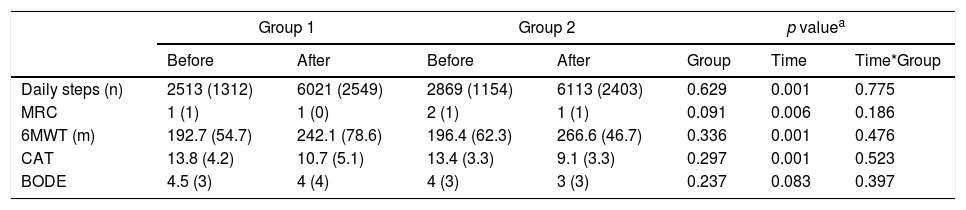
Table 2 shows the absolute values of the outcome measures before and after the programs. At the end of the program 44.5% patients of group 1 had reached the target daily steps, in 26.6 (9.5) days. Two-way ANOVA showed that following the programs both groups reported significant improvements in all measures except BODE.
Outcome measures before and after programs.
| Group 1 | Group 2 | p valuea | |||||
|---|---|---|---|---|---|---|---|
| Before | After | Before | After | Group | Time | Time*Group | |
| Daily steps (n) | 2513 (1312) | 6021 (2549) | 2869 (1154) | 6113 (2403) | 0.629 | 0.001 | 0.775 |
| MRC | 1 (1) | 1 (0) | 2 (1) | 1 (1) | 0.091 | 0.006 | 0.186 |
| 6MWT (m) | 192.7 (54.7) | 242.1 (78.6) | 196.4 (62.3) | 266.6 (46.7) | 0.336 | 0.001 | 0.476 |
| CAT | 13.8 (4.2) | 10.7 (5.1) | 13.4 (3.3) | 9.1 (3.3) | 0.297 | 0.001 | 0.523 |
| BODE | 4.5 (3) | 4 (4) | 4 (3) | 3 (3) | 0.237 | 0.083 | 0.397 |
Daily steps, 6MWT and CAT score are presented as mean (SD), MRC and BODE are shown as median (interquartile range).
MRC, Medical Research Council; 6MWT, six-minute walking test; CAT, COPD Assessment Test; BODE, Body-mass index, airflow obstruction, dyspnea, and exercise capacity index.
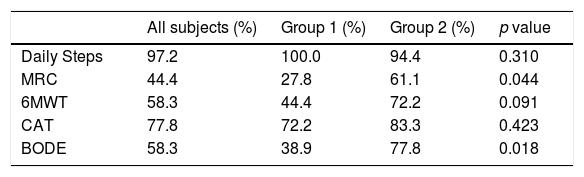
Table 3 shows the proportion of patients reaching the MCID in the post PRP evaluation. There was a significant difference in proportion of patients reaching the MCID only for the BODE and MRC which were more in Group 2 than in Group 1. The proportion of patients reaching the MCID in all outcome measures was greater than 60% only in Group 2.
Proportion of patients reaching the MCID in the post PRP evaluation.
| All subjects (%) | Group 1 (%) | Group 2 (%) | p value | |
|---|---|---|---|---|
| Daily Steps | 97.2 | 100.0 | 94.4 | 0.310 |
| MRC | 44.4 | 27.8 | 61.1 | 0.044 |
| 6MWT | 58.3 | 44.4 | 72.2 | 0.091 |
| CAT | 77.8 | 72.2 | 83.3 | 0.423 |
| BODE | 58.3 | 38.9 | 77.8 | 0.018 |
p values refer to between group comparison.
MRC, Medical Research Council; 6MWT, six-minute walking test; CAT, COPD Assessment Test; BODE, Body-mass index, airflow obstruction, dyspnea, and exercise capacity index.
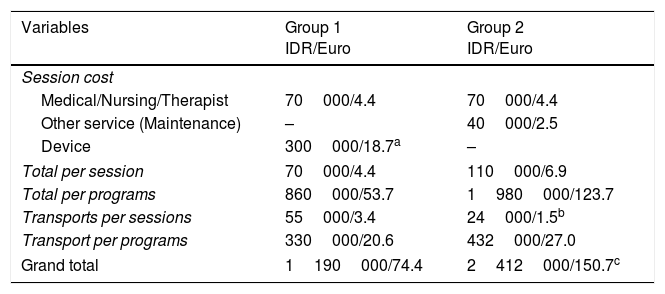
Table 4 shows the detailed costs of programs per individual patient. Despite the pedometer cost, the home program was cheaper with a mean 76.3 euros saving per patient. The median (interquartile range) for grand total cost was 932000 (36000) Indonesian Rupias (IDR) or 58.2 (2.2) euros versus 2124000 for (108000) IDR or 132.7 (6.7) euros for Group 1 and 2 respectively (p=0.0001). The difference was mainly due to the sessions involving professionals, the costs of doctors consultations and doctors/nurse supervisions of outpatient exercise training, and the costs of daily transportations of patients to and from the hospital required by Group 2 patients.
The costs per program per single patient.
| Variables | Group 1 IDR/Euro | Group 2 IDR/Euro |
|---|---|---|
| Session cost | ||
| Medical/Nursing/Therapist | 70000/4.4 | 70000/4.4 |
| Other service (Maintenance) | – | 40000/2.5 |
| Device | 300000/18.7a | – |
| Total per session | 70000/4.4 | 110000/6.9 |
| Total per programs | 860000/53.7 | 1980000/123.7 |
| Transports per sessions | 55000/3.4 | 24000/1.5b |
| Transport per programs | 330000/20.6 | 432000/27.0 |
| Grand total | 1190000/74.4 | 2412000/150.7c |
IDR, Indonesian rupiah.
A home pedometer assisted program to incentivize PA was cheaper than and as effective as a standard outpatient supervised exercise training program.
The baseline daily step count and 6MWT of our patients were lower than in other studies. In the study by Vorrink et al.,32 the mean daily step count and 6MWT in their intervention group were 5824 steps and 465m as compared to 2513 steps and 193m respectively, in our study. However the airway obstruction of our patients was more severe as shown by a mean FEV1 of 1.1 in our patients as compared to 1.7l in that study.32
Our results showed significant improvements in 6MWT and daily steps in both groups. However the mean improvement in 6MWT of Group 2 was slightly greater, albeit nonsignificantly, than in Group 1, whereas the change in daily steps was similar in both groups. This difference indicates the need to specifically assess both exercise capacity and PA, when evaluating the effects of pulmonary rehabilitation. Our results are similar to those of Mendoza et al.33: in that randomized study patients with COPD underwent either a standard program of PA encouragement alone, or a pedometer-based program. Their pedometer group gained significant improvements in PA (by 3080 daily steps) and CAT score (−3.5), similar to our results, and in 6MWT (by 12.4m), less than in our patients.33 An earlier study in Indonesian COPD patients31 showed after a 5-week program a mean 44m increase in 6MWT, a result similar to that observed in Group 1 of our study. The post-program improvement in exercise tolerance and in PA observed in our study translated into an improvement in health status as assessed by the CAT score and dyspnea as assessed by MRC in both groups. Previous studies found that MRC, due to its limited number of levels, was not sensitive enough to detect small changes after programs.34
In our study the perceived health status was assessed by the CAT score. A specific HRQL questionnaire such as the Saint George Respiratory Questionnaire (SGRQ) was not available at our Institution. Although CAT is correlated to SGRQ in terms of discriminating health status, there is evidence that the SGRQ shows a greater responsiveness in patients with COPD undergoing pulmonary rehabilitation.35
The main findings of our study suggest that independently of the setting, whether home pedometer assisted or standard outpatient program, our COPD patients gained similar mean improvements in assessed outcome measures, except the BODE index. However, from a clinical point of view, it is important to note that the proportion of patients reaching the MCID in all outcome measures was greater than 60% only in Group 2. Other studies have reported conflicting results. A 6-week online-supported pulmonary rehabilitation program was non-inferior to a conventional program in terms of effects on 6MWT, and symptom scores; furthermore it was safe and well tolerated.36 A home maintenance pulmonary rehabilitation program was equally as effective as an outpatient hospital, maintenance program in reducing the risk for acute COPD exacerbations and hospitalizations.16 Physical activity could be significantly increased in patients with COPD using a 12-week intervention including a step counter and a smartphone app.37 A home pulmonary rehabilitation program, delivered with minimal resources, produced short-term clinical outcomes similar to a center-based program.38
A recent simulation study39 has reported that pulmonary rehabilitation was cost-effective in every setting in the comprehensive management of patients with COPD. In the programs of our study as a whole the cost per patient of Group 1 was about half than that of Group 2. In the frame of Indonesian economy the mean 76.3 euros saving per patient obtained in Group 1, is not negligible. The cost analysis in our study involved direct costs and transportation as the only indirect cost. We were unable to calculate other indirect costs, such as time spent by relatives to transport patients to and from the hospital, or costs of exacerbations, hospital admissions or unscheduled visits. Previous studies reported a reduction in health service usage in rehabilitated outpatients. Griffiths et al.,40 reported that outpatient pulmonary rehabilitation produced cost per quality adjusted life years (QALYs) ratios within bounds considered to be cost effective. In a retrospective case-control study,41 a short-term, inpatient pulmonary rehabilitation program induced a short-term improvement in exercise tolerance, similar to a longer, outpatient program. The duration of program and the need for daily transportation significantly influenced the total costs of the outpatient pulmonary rehabilitation.41 In a RCT including an economic evaluation, outpatient pulmonary rehabilitation appeared highly cost-effective in comparison with a program incorporating a substantial period of inpatient care.30,42 Comparisons of cost-effectiveness between programs performed in different countries, institutions and health-care systems are difficult because of differences in case-mix, outcome measures, and the time-points when outcomes are measured. Therefore, the application of our results to other health-care systems must be considered with caution.
Our study has some limitations. We have compared home pedometer assisted PA with outpatient supervised exercise training. Stimulated PA and supervised exercise training are only two of the components of pulmonary rehabilitation which, according to the ATS/ERS statement,10 should also include other multidisciplinary interventions such as education, and behavior change. Whether a more comprehensive intervention also including other components as defined by that statement10 would have obtained different results, remain to be evaluated. We have also compared two groups performing a different number of exercise sessions. On the other hand our results may indicate also the effectiveness of our supervised hospital based outpatient program achieving the same benefits as an unsupervised program despite less exercise sessions. The use of pedometers by the home program might have introduced some bias to the study, as standard hospital based programs do not routinely offer this device. Patients and researchers were not blind to allocation. However, this bias probably would have favored results of Group 1 which in fact did not show any superiority over Group 2.
In conclusion with these limitations this preliminary RCT showed that, at least in our health-care system and for our patients with COPD, a home pedometer assisted program to incentivize PA may be a useful and cheaper alternative to outpatient supervised exercise training programs.
Conflicts of interestThe authors have no conflicts of interest to declare.