Lung cancer is the leading cause of cancer death, making up almost 25 % of all cancer deaths. Unfortunately, most lung cancer patients initially present with locally advanced or metastatic disease.1 Up to 24 % of patients with non-small cell lung cancer present with an additional pulmonary nodule, and up to 8 % of lung cancer patients present with two or more anatomically separate lung nodules.2 In patients with more than one lung lesion, tissue diagnosis may allow differentiation between intrapulmonary metastasis (whether ipsilateral or contralateral) and synchronous second lung primary cancer.3 The initial management of lung cancer patients who present with more than one lung lesion remains a diagnostic challenge and can significantly delay treatment decisions and initiation of therapy. To the best of our knowledge there are no previous descriptions of multiple percutaneous lung biopsies during a single interventional session, except for one single study that only described ipsilateral (i.e., within the same lung) biopsies.4 We present a previously undescribed technique consisting of the performance in a single interventional procedure of a bilateral computed tomography (CT)-guided core-needle biopsy in a lung cancer patient who presented with 2 lung lesions.
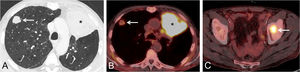
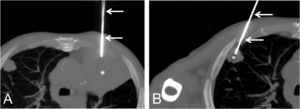
A 67-year-old patient with hemoptysis was found to have 2 lung lesions on CT: a larger pulmonary mass in the left upper lobe and a smaller lung nodule in the right upper lobe (Fig. 1A). An 18F-fluorodeoxyglucose (FDG) positron emission tomography/CT (PET/CT) ruled out mediastinal involvement and showed that the FDG-avidity of the bilateral lung lesions was markedly different (maximum standardized uptake value [SUVmax] of left upper lobe mass: 9.4; SUVmax of right upper lobe nodule: 2.9), suggesting the possibility that the 2 lung lesions corresponded to synchronous primary lung tumor (Fig. 1B). PET/CT also confirmed a single bone metastasis in the left acetabular roof (Fig. 1C) showing intense FDG uptake (SUVmax; 10.2). The tumor board discussed these findings and finally agreed that the patient most likely had 2 primary lung tumors: one in the left upper lobe (cT4N0M1b with a single bone metastasis) and one in the right upper lobe (cT1bN0M0). The multidisciplinary decision was made to percutaneously biopsy the two pulmonary lesions. Since the patient was taking antiplatelet therapy, the interventional thoracic radiologist proposed performing a “double” CT-guided core needle biopsy in one single session with the intention not to discontinue twice his antiplatelet medication, thus avoiding risks related to the suspension of this drug. The “double” CT-guided biopsy procedure was performed under local anesthesia sequentially during the same interventional session: first, the lung lesion with the lowest anticipated risk of pneumothorax was biopsied (the left upper lobe mass) and, afterwards (once pneumothorax was ruled out following the first lung biopsy), the contralateral lung lesion (the right upper lobe nodule) was biopsied (Fig. 2A, B). Both pulmonary lesions were biopsied using an 18 G cutting needle (different coaxial biopsy system for each lesion) under CT guidance, and 3 tissue samples were obtained from the left upper lobe lung mass whereas 2 tissue samples were obtained from the right upper lobe lung nodule. The “double” lung biopsy was uneventful (no pneumothorax or lung hemorrhage occurred) and the patient was discharged 6 h later, once a chest X-ray performed 3 h after the biopsy ruled out a delayed pneumothorax. The pathological diagnosis initially confirmed that these 2 lung lesions represented 2 malignant primary lung tumors (two squamous cell carcinomas with different immunohistochemical profile). Comprehensive next-generation sequencing (NGS) was not performed on the specimens obtained from both lung lesions. The patient started treatment with a combination of chemotherapy and immunotherapy; in addition, it was decided to treat with stereotactic radiotherapy both the single bone metastasis and the right upper lobe lung nodule.
(A) Axial thoracic contrast-enhanced CT image (lung window) shows a large left upper lobe mass (asterisk) and a smaller right upper lobe nodule (arrow). (B) Axial fused PET/CT image demonstrates intense FDG uptake by the left upper lobe mass (asterisk) but mild FDG avidity by the right upper lobe nodule (arrow), suggesting two synchronous primary lung tumors. (C) Axial fused PET/TC image shows an FDG-avid bone lesion involving the left acetabulum (arrow).
“Double” lung biopsy performed during one single session. (A) Axial thoracic MIP (maximum intensity projection) CT image (lung window) shows the needle (arrows) targeting the left upper lobe mass (asterisk). (B) Axial thoracic MIP CT image shows the needle (arrows) targeting the right upper lobe nodule (asterisk).
The initial management of lung cancer patients presenting with more than one lung lesion remains a diagnostic challenge and can significantly delay treatment decisions and initiation of therapy. In patients with more than one lung lesion, tissue diagnosis may allow differentiation between intrapulmonary metastasis and synchronous second lung primary cancer.5 It should also be taken into account that the time elapsed between the clinical suspicion of lung cancer and its histological diagnosis is inversely related to overall survival, so it is essential to expedite the diagnostic process of obtaining biological samples for optimal processing.6 Barnett et al. reported a series of ipsilateral dual-site, same-sitting lung biopsies in 10 patients, with a pneumothorax rate of 60 % (although only 2 patients required drainage).4 Their relatively high incidence of pneumothorax is probably related to their particular definition of biopsy-induced pneumothorax. We believe that our sequential technique of starting the “double” biopsy procedure with the lung lesion with the lowest anticipated risk of pneumothorax in lung cancer patients with more than one lung lesion might minimize the risk of pneumothorax. Unlike conventional staged-biopsy procedures in patients with more than one lung lesion (in which patients return following a convalescent period for the second or subsequent biopsy), our single-session technique may expedite the histological diagnosis and may alter the staging and management of lung cancer patients. The final decision to classify two pulmonary lesions as synchronous primary cancers or two foci of a single lung cancer should be based on the judgment of the lung cancer multidisciplinary tumor board, by incorporating all patient information (clinical data, imaging findings, histopathological and immunohistochemical results, and genetic analysis). Among the limitations of performing a double lung biopsy in a single procedure are: 1) a longer duration of the biopsy procedure; 2) an increased risk of pneumothorax; and 3) the radiologist performing the biopsy should be trained to place pleural drainages to treat any significant pneumothorax.
To the best of our knowledge, there are no previous descriptions of a bilateral CT-guided needle core lung biopsy during a single interventional session. The case presented demonstrates that a percutaneous CT-guided bilateral lung biopsy can be safely performed in a single interventional procedure and may expedite both the pathological diagnosis and the staging process of some lung cancer patients presenting with more than one pulmonary lesion.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical considerationsWritten informed consent was obtained for use of clinical data and publication.
CRediT authorship contribution statementL. Gorospe: Conceptualization, Writing – original draft, Writing – review & editing, Validation, Methodology. M.Á. Gómez-Bermejo: Conceptualization, Writing – original draft, Writing – review & editing, Validation. S. Ventura-Díaz: Methodology. Mirambeaux-Villalona: Formal analysis. A. Caminoa-Lizarralde-Aiza: Supervision. P. Paredes-Rodríguez: Methodology.
The six authors all made substantial contributions to not only the conception and design of the manuscript, but also the drafting and critical revision of the article.