Osteonecrosis of the jaw (ONJ) can occur as a complication of bisphosphonate therapy. This condition has been described in cancer patients and its development has been associated with prolonged exposure to high doses of bisphosphonates. Bad dental hygiene, a history of prosthesis or dental extraction, chemotherapy, corticosteroids, and radiation therapy of the head and neck are reported risk factors. In the initial stages it may be asymptomatic, but the patient subsequently develops severe pain and progressive exposed bone. The authors describe three cases of ONJ in lung cancer patients after prolonged exposure to bisphosphonates and there were known risk factors. ONJ can seriously affect the quality of life of cancer patients. An early diagnosis may reduce or avoid the consequences of progressive bone lesion.
A osteonecrose da mandíbula (ONM) pode surgir como complicação do tratamento com bifosfonatos. Esta patologia tem sido descrita em doentes com cancro e o seu desenvolvimento associado a exposição prolongada a altas doses de bifosfonatos. Má higiene dentária, história de uso de próteses ou extração dentária, quimioterapia, corticosteroides e radioterapia da cabeça e pescoço são fatores de risco reportados. Nas fases iniciais pode ser assintomática, contudo, o doente posteriormente desenvolve dor significativa e exposição óssea progressiva. Os autores descrevem 3 casos de ONM em doentes com cancro do pulmão após exposição prolongada a bifosfonatos e na presença de fatores de risco conhecidos. A ONM pode atingir seriamente a qualidade de vida dos doentes com cancro. O diagnóstico precoce poderá reduzir ou mesmo evitar as consequências da lesão óssea progressiva.
Bone metastization in patients with lung cancer is a frequent finding at presentation or during disease progression. Bisphosphonate therapy has demonstrated efficacy in this setting.1–5
Since the first reports in 2003, an association between bisphosphonates and osteonecrosis of the jaw (ONJ) has been described.6–11 The pathophysiologic mechanism underlying ONJ still needs to be clarified, but it seems to involve impaired blood supply and secondary microorganism spread.12–14
ONJ occurs mainly in patients with prolonged exposure to high doses of IV bisphosphonates when risk factors are present. 6–11 In cancer patients the development of ONJ associated with bisphosphonates is most commonly seen in multiple myeloma and breast, prostate, and lung cancers.15–17
In the initial stages of ONJ the patient may be asymptomatic, but subsequently develops severe pain and progressive exposed bone.18,19
Case reportsCase 1A 49-year-old man with stage IV lung adenocarcinoma (M1 lung, brain, and bone) diagnosed in May 2010 was submitted to two lines of chemotherapy, brain radiotherapy (30Gy, 12 fractions), and 12 treatments with intravenous (IV) zolendronic acid 4mg, every 3/3 weeks. During the course of the disease, chronic corticotherapy was prescribed. He had a previous history of tooth extraction with poor healing two months before starting bisphosphonates.
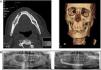
In March 2011, after 10 months of exposure to IV zolendronic acid, the patient experienced trismus with pain and soft-tissue swelling in the right jaw. At that time he was taking erlotinib 150mg/day as a third-line treatment. Computed tomography (CT) of the face showed a marked change in the bone trabeculation of the right jaw, and orthopantomography confirmed alterations consistent with osteonecrosis (Fig. 1).
He was initially treated with multiple courses of antibiotics and analgesics, but because he maintained progressive bone exposure with associated bleeding, surgical treatment was proposed. In January 2012, he underwent maxillofacial surgery eight months after discontinuation of zolendronate. Long-term evaluation confirmed good recovery. The histopathological examination of bone tissue revealed no signs of metastasis.
Case 2A 59-year-old man with stage IV non-small cell lung carcinoma (M1 bone) diagnosed in January 2008 received two lines of chemotherapy, thoracic radiotherapy (30Gy, 12 fractions), 35 treatments with IV pamidronate 90mg, and subsequently oral ibandronic acid 50mg/day. Pulse corticosteroids in association with chemotherapy were also prescribed.
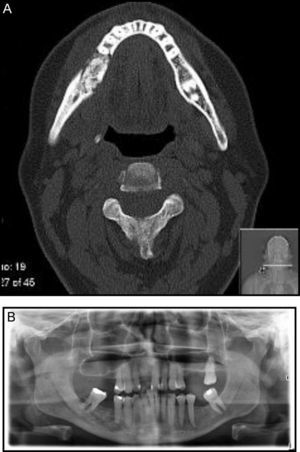
The patient had a history of denture that traumatized the alveolar ridge and bad dental hygiene. In November 2010, he experienced pain associated with bone exposure at the site of trauma. Face CT and orthopantomography confirmed the diagnosis. At that time, the patient was taking pemetrexed and had been treated for 26 months with IV pamidronate every 3/3 weeks followed by 9 months of oral ibandronic acid daily.
Bisphosphonate was suspended, and conservative treatment was started. However, a pathological fracture of the right jaw later occurred, and the patient was submitted to surgical reconstruction in May 2011 (Fig. 2). The histopathological examination did not show bone tissue metastasis.
Case 3A 64-year-old man with stage IV adenocarcinoma (M1 bone) diagnosed in June 2011 was treated with two lines of chemotherapy, thoracic radiotherapy (45Gy, 18 fractions), and 18 treatments with IV zolendronic acid 4mg until June 2012. Chronic corticotherapy was also prescribed. He had a history of tooth extraction during lung cancer treatment.
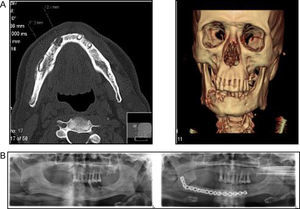
During 2nd-line chemotherapy with pemetrexed, and after being treated with IV zolendronic acid every 3/3 weeks for 12 months, the patient complained of dysesthesias of the jaw. Face CT revealed a cortical irregularity of the right jaw, and orthopantomography depicted an image consistent with osteonecrosis (Fig. 3). Bisphosphonate was discontinued, and antibiotics were started. This resulted in clinical improvement, and no complications have been detected so far.
DiscussionONJ associated with bisphosphonates may complicate treatment of cancer patients with bone metastasis. As these three clinical cases illustrate, such ONJ occurs mainly in patients with prolonged exposure to high doses of IV bisphosphonates and in the presence of risk factors.
The bisphosphonatesAlthough ONJ can occur with any kind of bisphosphonate, it seems that the risk with zolendronic acid is significantly higher compared with others.
Bamias et al. published a prospective study of 17 cancer patients who developed ONJ after treatment with bisphosphonates, showing that the cumulative hazard of developing ONJ increased over time of exposure to bisphosphonates, and the hazard risk was significantly higher in the zolendronic acid group.9 Boonyapakorn et al. also published results that confirmed the previous study; an additional important finding was that the mean induction time until bone exposure was lower in patients who received zolendronate.11 These results could explain the precocity of ONJ development seen in our two patients who received zolendronic acid, after 10 and 12 months, respectively, compared with the 35 months observed in the patient who received pamidronate later followed by ibandronate.
The risk of developing ONJ also seems to be correlated with the route of administration. In the Fleisher et al. cohort, the median onset of ONJ for patients undergoing IV bisphosphonate therapy occurred earlier than the median onset for patients undergoing oral therapy.20
Risk factorsA history of tooth removal or other surgical treatment, as well as denture use, has been implicated in the development of ONJ associated with bisphosphonates.17 Two of our patients had a history of dental procedure, and the other had a denture that caused traumatism of the alveolar ridge.
While the incidence is uncertain, a strong association with dental pathology and interventions highlights the need to pay close attention to dental health in this patient group.15,21 Most series showed that ONJ occurs mostly after oral surgical procedure, in about 50–80% of patients.11,15,16
With this in mind the American Society for Bone and Mineral Research Guidelines suggest that patients taking bisphosphonates should be encouraged to maintain good oral hygiene. Whenever possible, the patient should have a dental evaluation before and throughout the course of therapy.19 This American Task Force also recommends that treatment with bisphosphonates should only be started after dental procedures have healed, and elective dentoalveolar surgery should be avoided during therapy.19
Other risk factors mentioned were also present in the three cases reported, such as corticosteroids, chemotherapy, and head and neck radiotherapy. Because of the diversity of chemotherapy regimens and timing of administration, it is impossible to analyze the contribution of the different regimens in the development of ONJ. The same is true of corticosteroids and radiotherapy. Most of the patients who developed osteonecrosis were treated with one or more of these treatments.9,11
TreatmentThe oncologist must be aware of bisphosphonate-induced ONJ in order to make an early diagnosis. Further management should be carried out by a qualified dental specialist.22
Osteonecrosis treatment of patients receiving bisphosphonates is essentially preventive. When ONJ develops, the symptoms should be treated and pain should be managed with appropriate analgesia. If there is evidence of infection, treatment should include antibiotics.8,22–24 When infection and exposed bone persist, surgical management should be considered on a case-by-case basis.18,19
Some experts suggest stopping IV bisphosphonates in cancer patients with established ONJ depending on the clinical situation. However, there is no scientific evidence that discontinuation of therapy will promote the healing of necrotic bone tissues. The decision to discontinue bisphosphonates must be evaluated and based on risk-benefit analysis.18,19,22–25
ConclusionONJ seriously affects the quality of life of cancer patients, producing significant morbidity and leaving permanent sequelae. An early diagnosis of ONJ may reduce or avoid the consequences of progressive bone lesion. However, what is most important is to ensure a preventive approach and establish protocols between oncologist and dentist to improve patient care.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Neves I, Morais A, Magalhães A. Osteonecrose da mandíbula associada aos bifosfonatos em doentes com cancro do pulmão. Rev Port Pneumol 2013;19:228–232.