Exogenous lipoid pneumonia (ELP) is an uncommon condition resulting from aspirating or inhaling fatlike material. These substances elicit a foreign body reaction and proliferative fibrosis in the lung.
Case reportWe report a case of a 38-year-old woman with bilateral pulmonary infiltration. There were no clinical symptoms of this infiltration at diagnosis. The infiltration was found coincidentally during the pre-operation examination before surgery. A chest computed tomography scan revealed bilateral lung consolidation, particularly in the S6 area on the right side. The transthoracic lung biopsy led to suspicion of ELP. Precise anamnesis confirms the diagnosis of ELP caused by chronic improper use of baby body oil. Two years after discontinuing “baby body oil therapy”, a chest CT scan revealed partial regression of pulmonary infiltration.
ConclusionThe diagnosis of exogenous lipoid pneumonia is often difficult as symptoms, signs, and radiographic findings are all rather non-specific. We would like to emphasize the role of precise case history in better identification of ELP.
A pneumonia lipoide exógena (ELP) é uma condição incomum resultante da aspiração ou inalação de material gorduroso. Estas substâncias provocam uma reação a corpo estranho que pode resultar em fibrose pulmonar proliferativa.
Caso clínicoNeste trabalho relatamos o caso de uma doente de 38 anos com infiltrado pulmonar bilateral. Não houve sintomas resultantes desta infiltração infiltração no momento do diagnóstico. Esta alteração imagiológica foi encontrada, por acaso, durante o exame pré-operatório. A tomografia computadorizada do tórax revelou consolidação pulmonar bilateral, particularmente na área S6 do lado direito. A biópsia transtorácica pulmonar conduziu a uma suspeita de ELP. Uma análise precisa do histórico da paciente confirmou o diagnóstico de ELP provocada por uma utilização continuada e desapropriada de óleo corporal para bebés. Dois anos após a descontinuação da exposição ao óleo corporal para bebés, uma tomografia computorizada de tórax revelou uma regressão parcial do infiltrado pulmonar.
ConclusõesO diagnóstico de pneumonia lipoide exógena é muitas vezes difícil, já que os sintomas, sinais e imagens radiológicas são bastante inespecíficos. Gostaríamos de destacar a importância da análise precisa do histórico dos pacientes para uma melhor identificação de ELP.
Lipoid pneumonia can be classified as endogenous, idiopathic, or exogenous.1 Endogenous lipoid pneumonia is the least frequent and is generally observed in patients with chronic bronchial obstruction of the airways by tumors, bronchiolitis obliterans, and lipid storage diseases such as Gaucher's disease and Niemann–Pick disease. Idiopathic lipoid pneumonia is a rare disorder and has been associated with smoking in healthy individuals. Exogenous lipoid pneumonia (ELP) is an uncommon condition resulting from aspirating or inhaling fat-like material.1,2 These substances elicit a foreign body reaction and proliferative fibrosis in the lung. Symptoms can vary significantly among individuals, ranging from asymptomatic to severe, life-threatening disease. The radiological findings have variable patterns and distribution. For this reason, lipoid pneumonia may mimic many other diseases.1 The diagnosis of ELP is based on a history of exposure to oil, characteristic radiological findings, and the presence of lipid-laden macrophages in sputum or BAL analysis. There are currently no studies in literature that define the best therapeutic option; however, there is a consensus that the key measure is identifying and discontinuing exposure to the offending agent.1,2
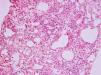
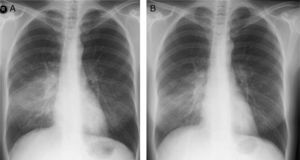
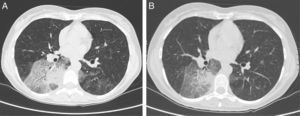
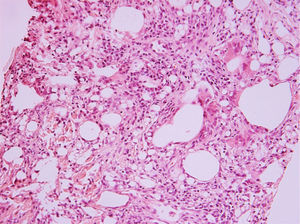
Case reportA 38-year-old woman was referred to our department for bilateral pulmonary infiltration. The infiltration was found coincidentally during the pre-operation examination before leg varices surgery. Nothing was bothering the patient. She was a non-smoker and did not take any regular medication. The pulmonary function test proved a mild impairment of diffusing capacity (61% diffusing capacity for carbon monoxide – DLCO). Nevertheless, her chest X-ray disclosed extensive infiltration in both lungs (Fig. 1A). A chest computed tomography (CT) scan revealed bilateral lung consolidation, particularly in the S6 area on the right side (Fig. 2A). In differential diagnosis according to findings of high-resolution CT (HRCT) of thorax, we considered pulmonary alveolar proteinosis, alveolar hemorrhage, or bronchioloalveolar carcinoma. However, the clear right predominance of lesions gave primary support to the aspiration etiology of lesions. Laboratory blood findings (hematology, biochemistry, antibody, tumor markers) were normal. By auscultation, we found sporadic crackles over the right lung. The bronchoalveolar fluid had a greasy appearance. Lymphocytic alveolitis was also found (lymphocytes 21%). The transthoracic lung biopsy revealed vacuolated macrophages, giant cells, optically empty spots, a foreign body reaction with granulomatous process. All vacuolated macrophages contained lipids (lipophages) and represented 35% of all cells in the biopsy. This finding raised the suspicion of oil substance aspiration – ELP (Fig. 3). Subsequently, the patient confessed to daily nasal application of baby body oil drops (with azulene and medicinal liquid paraffin) over a period of five years to treat the dryness of her nasal mucosa. The otorhinolaryngologic examination was normal. The patient refused glucocorticoid therapy. Regular controls of the pulmonary function test, chest X-ray (Fig. 1B) and HRCT of thorax were performed in the patient. Two years after discontinuing “baby body oil therapy”, a chest CT scan revealed partial improvement (Fig. 2B). We proposed additional corticosteroid therapy due to persisting lesions on CT. However, this therapy was refused by the patient.
Chest high-resolution computed tomography (HRCT) at diagnosis (A) and two years after diagnosis (B). Bilateral lung infiltration in the lower lobes, particularly on the right side in the area of segment S6, with the following dimensions: 85mm×38mm×70mm. The surrounding tissue shows ground-glass opacities, thickened interlobular septa, and a craving paving picture with air bronchogram (A). Partial regression of pulmonary infiltration after discontinuation of “baby body oil therapy” (B).
Hematoxylin- and eosin-stained slide (×200) of patient's lung tissue. Instead of normal alveoli in the lung, there are empty spaces of different sizes, lined with partially flattened multinucleated giant cells. Between those empty places, there is fibrous connective tissue, sometimes with infiltration of lymphocytes. In the connective tissue, there are also foreign body granulomas with large multinucleated cells that have vacuoles in the cytoplasm. The lesions do not have a distinct margin from the normal lung.
ELP is a rare disease resulting from the micro-aspiration of lipid formulations. These substances elicit a foreign body reaction and proliferative fibrosis in the lung. Acute, sometimes fatal, cases can occur, but the disease is usually indolent. The diagnosis of ELP is often difficult as symptoms, signs, and radiographic findings can be non-specific.1 On HRCT, alveolar filling causes a ground-glass pattern of a crazy paving appearance, which stays at some distance from the pleura and exhibits low attenuation numbers. On the other hand, in unenhanced HRCT, pulmonary vessels may spontaneously be visible within the areas of parenchymal filling, a sign known as the “spontaneous angiogram”.3–5 The most characteristic computed tomography of finding of ELP is the presence of low-density space consolidation (−30 to −150 Hounsfield units) in the lungs.6 As illustrated by our case, there should be a clear right predominance of lesions supporting an aspiration etiology of pneumonia. A lung biopsy is not always indicated for diagnosis.1 Diagnosis of ELP is suggested at history taking, and is confirmed by the examination of sputum or BAL, which show lipid laden cells and free-floating oil.
Our case was caused by improper use of baby body oil containing paraffin. So far, paraffin has been described as a cause of ELP in fire-eaters,7–9 and in children.10 In differential diagnosis of ELP in adults, mainly lipoid pneumonia caused by amiodarone must be taken into consideration.11
Treatment of LP is not well-studied. Treatment in patients without clinical symptoms remains controversial, but in patients with diffuse pulmonary damage, therapies have been reported. Avoiding ongoing exposure and providing supportive care is the mainstay of treatment. Not every patient with exogenous lipoid pneumonia will improve after the withdrawal of lipid-containing material or corticosteroid therapy. Gondouin et al., in a retrospective multicenter study, found that corticosteroid therapy had not been very effective for every cases of lipoid pneumonia.1 The use of systemic corticosteroids in patients without clinical symptoms remains controversial; however, whole lung lavages, and systemic corticosteroids have been used in patients with diffuse pulmonary damage.1,12 In our case, however, corticosteroid therapy has been refused by the patient. Complications of this disease include recurrent bronchopneumonia, superinfection, pulmonary fibrosis, and lung cancer.1
ConclusionThe diagnosis of ELP is often difficult as symptoms, signs, and radiographic findings can be non-specific. Chronic improper use of miscellaneous oil substances can cause this very rare disorder and we would like to emphasize the role of precise case history in better identification of interstitial lung disorders. Correct HRCT description avoids the misdiagnosis of ELP.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.