Lymphadenopathy is the most common form of extra-pulmonary tuberculosis (EPTB).1
Diagnosis of EPTB may not be easy, given the lack of specific presentation, the need for tissue sampling, the lack of accessible tissue, non-specific pathological findings and the relatively low microbiological yield.
The aim of our study was to review the diagnostic approaches to tuberculosis (TB) lymphadenitis.
All TB lymphadenitis cases treated in an urban Chest Disease Center in Portugal, from 2003 to 2010, were reviewed. Patients were referred after diagnosis, either to start or continue treatment. They all had a positive response to anti-bacillary treatment.
Positive cyto/histological results were defined as findings of histological features compatible with TB2 (granulomatous inflammation and epithelioid cells with/without Langhans cells, caseous necrosis or positive Ziehl–Nielsen stain in lymph node (LN) samples). Positive microbiological results were defined as positive results on smear, culture or nucleic acid amplification test (NAAT).
We received 60 patients with TB lymphadenitis, 26 male and 34 female, with a mean age of 52.9±20.8 years. They were all tested for human immunodeficiency virus (HIV) and 8 tested positive. Collection of LN tissue was performed through fine-needle-aspiration cytology (FNAC) in 34 (56.7%) and through excision in 24 (40%). For 2 patients there was no information.
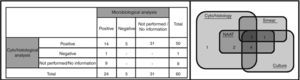
A cyto/histological analysis was performed on 51/53 patients (there was no information on 7), which was positive for 50/51 (98%) (Fig. 1). A microbiological analysis was performed on 29/59 (no information on 1 patient), which was positive in 24 (82.8%). A positive smear was found in 14/29 (48.3%), positive culture in 19/28 (67.9%) and positive NAAT in 14/16 (87.5%) (Fig. 1). No differences were found between the microbiologically tested group and other patients, in terms of sex, age, HIV-infection, previous TB and recent TB contact. No differences in diagnostic yield were found between FNAC and excision.
It becomes clear that in the approach to lymphadenitis it is still not routine to send LN samples for both cyto/histological and microbiological analyses. Since the diagnostic process was not conducted in our center, it is not possible to exclude the presence of bias on the cohort that was microbiologically assessed, whether these patients had a higher suspicion for TB or not.
Culture for Mycobacterium tuberculosis is the primary diagnostic standard,3 not only for diagnosis, but also to provide information about drug susceptibility. However, it is time-consuming and sensitivity is not very high (43–88%).3 When cyto/histological analysis is combined with smear and culture results the diagnostic efficacy of NAAT did not improve. However, there are some important advantages of NAAT, such as immediate response, high specificity3,4 and the possibility of molecular resistance tests, when drug resistance is suspected.5
These results strengthen the case for increased suspicion of TB lymphadenitis and for utilization of a combination of cytology/histology and microbiology in diagnostic approaches to lymphadenitis.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Soares Pires F, van Zeller M, Reis R, Carvalho A, Duarte R. Abordagem diagnóstica na tuberculose ganglionar. Rev Port Pneumol. 2013;19:237–238.