Bronchiectasis (BE) is characterized by irreversible dilation and damage to the bronchial walls. It is a morphological expression of a large variety of pathologies.
The true prevalence of BE is unknown. It is known, however, that in Third World countries it is common due to lung infections. Its current prevalence in developed countries is rather significant due to a greater capacity for diagnosis, its association with highly prevalent diseases and to a greater chronicity of some of the underlying pathologies.
Over the last few decades there has been little interest in the investigation of BE, unless it is associated with cystic fibrosis. One of the reasons is the presupposition that treatment is the same for all patients diagnosed with BE, regardless of the underlying aetiology. Several works carried out over the last decade show that a diagnosis based on aetiology changes both the approach and the treatment of BE within a relevant percentage of patients, with a consequent change in the prognosis.
Currently, systematic investigation into the aetiology of BE is recommended, particularly in those disorders that respond to specific treatment.
As bronquiectasias caracterizam-se por uma dilatação e destruição irreversível das paredes brônquicas. São a expressão morfológica de uma grande variedade de patologias.
A verdadeira prevalência das BE é desconhecida, contudo sabe-se que são frequentes nos países de Terceiro Mundo devido a infecções pulmonares. A sua prevalência nos países desenvolvidos é também significativa em consequência da maior capacidade de diagnóstico, da sua associação com doenças de prevalência elevada e da maior cronicidade de algumas das patologias subjacentes.
Durante as últimas décadas tem havido pouco interesse na investigação das BE, exceptuando as consequentes à fibrose quística. Uma das razões relaciona-se com o pressuposto de que o tratamento é comum a todos os doentes com BE, independentemente da etiologia subjacente. Vários trabalhos nesta última década demonstraram que a obtenção de um diagnóstico etiológico modifica a abordagem e o tratamento numa percentagem relevante de doentes e consequentemente o seu prognóstico.
Recomenda-se actualmente a investigação sistemática da etiologia, principalmente das doenças que poderão responder a um tratamento específico.
Bronchiectasis (BE) is characterized by irreversible dilation and damage to the airways, associated with a vicious cycle of inflammation, recurrent infection and bronchial impairment.
BE is frequently described as a lung disease but it is more appropriate to say that it is the pathological expression of a large variety of disorders. However, its aetiology is still unknown in many cases.
Practically two centuries have gone by since Rene Laennec described a patient with BE 1 for the first time, more than 80 years since Jean Athanase Sicard introduced the bronchography as a diagnostic tool, 2 more than 50 years since Reid described and classified BE based on histologic and bronchographic findings 3 and approximately 20 years since high resolution computed tomography (HRCT) has progressively replaced bronchography as a diagnostic tool.
Over the last century several syndromes/pathologies associated with BE have been described: the Mounier-Kuhn syndrome in 1932, 4 cystic fibrosis (CF) in 1944, 5 the Williams-Campbell syndrome in 1960, 6 the yellow nail syndrome in 1964, 7 diffuse panbronchiolitis in 1969, 8 the Young's syndrome in 1970, 9 the Lady-Windermere syndrome in 1992. 10
During the last two decades of the 20th century an apparent correlation was noted between BE and several systemic disorders, such as rheumatoid arthritis, inflammatory bowel disease and AIDS. 11 Just recently an association between the autosomal dominant polycystic kidney disease and BE 12 has also been described.
Towards the end of the 80's, Barker defined BE as “an orphan disease”, 13 referring to the definition used to describe diseases that had been forgotten by the scientific community and were of no interest for therapeutic research due to the supposedly low prevalence. 14
EpidemiologyThere are very few studies on the true prevalence of BE. In the past, tuberculosis, whooping cough and measles were seen as the significant causes of BE. Better social conditions, the development of broad spectrum antibiotics, the appropriate treatment of pulmonary tuberculosis and vaccination during childhood have most certainly contributed toward a decrease in postinfectious BE in developed countries. On the other hand, various factors have contributed to an increased prevalence of BE in these same developed countries: greater diagnostic capability through the use of HRCT, insight into new causes of BE that are highly prevalent, such as AIDS, recognising that BE can be a possible complication of heart, lung and bone marrow transplants and the higher survival rate of patients with CF and immunodeficiency disorders.
In the 40's and 50's in the United Kingdom, there was described a prevalence of 77-130/100,000 inhabitants. 15,16 A recent study, carried out in the USA, calculated a prevalence of 52/100,000 adults. Prevalence was higher in women of all ages, a fact which is in accordance with many other studies. 17
There was considerably higher prevalence noted in some communities: 16/1,000 in children from a region in Alaska, 15/1,000 in aboriginal children from Australia and 1/6,000 in children from New Zealand. 18–20 These differences are essentially due to social and economic conditions, although other possible underlying genetic factors are also being considered.
There are only 2 studies that estimated incidence. In Finland there was an annual incidence of 0.5/100,000 for children under 15 years of age and 3.9/100,000 for the total population and in New Zealand it was estimated an incidence of 3.7/100,000 for children under 15. 21,22
A study carried out in the USA revealed that treatment costs per patient were higher than those spent on heart disorders and COPD. 17 Data provided by the United Kingdom indicate that 78 % of patients afflicted by BE that use the emergency services are hospitalized and one third have at least one annual exacerbation that requires hospitalization, lasting for an average of 10.5 days, higher than that estimated for other pathologies such as asthma and COPD. 23 To conclude, in another study it was noted that 25 % of the patients died within the 9 years following the first hospitalization during which BE was detected. 24
The importance of diagnosis and of aetiological investigationDespite the increasing interest in this pathology, BE continues to be underdiagnosed and given little importance. Many cases are misdiagnosed as asthma or COPD. 25
Most cases are diagnosed when the illness is already in an advanced stage even though symptoms have been present for many years. 26 Early diagnosis of BE probably will have a positive effect on the prognosis, as has been demonstrated by doing screenings for CF in newborns. 27
Several studies suggest that the HRCT is more sensitive than the pulmonary function studies in detecting early damage and in assessing the development of the disease, because radiological scales become significantly worse in serial HRCT while the pulmonary function remains stable. 28
The importance of a BE diagnosis also arises from the fact that its presence can increase the morbidity and mortality of the underlying disease. This has already been registered, for instance, in COPD. 29,30
CF has been highly researched. These patients are normally put in specialized units where there is general consensus regarding the treatment and follow-up of the disease. However, this does not happen with BE caused by other aetiologies and so they are commonly called non-CF BE.
Non-CF BE comprises patients with BE from rather distinct aetiologies. The latter are usually broadly described and not differentiated according to their underlying aetiologies. 31
For many years BE was believed to be caused by serious infections so a standard protocol of investigating other possible aetiologies was rarely pursued, a practice which continues today.
Nowadays aetiological investigation is far more complex and has progressively been focusing on intrinsic causes such as CF, birth defects, ciliary changes and immunodeficiency.
The studies which have been published show varied rates of aetiological diagnosis, probably due to the use of different criteria, populations and levels of investigation.
In certain cases obtaining an aetiological diagnosis is undervalued because it is not considered relevant for treatment. In a review carried out on 136 children with BE, a cause was identified in 101 patients (74.3 %). In 56 % of these cases, this identification implied a change in the individual treatment plan. 32 Pasteur et al investigated the cause of BE in 150 adults and was able to give a diagnosis in 47 % of the cases. In 15 % of the patients, identifying the cause significantly affected both the prognosis and the treatment. 26 Shoemark et al also studied the aetiology of BE in 165 adults but obtained a higher rate of diagnosis (74 %). The diagnosis changed the therapeutic strategy in 37 % of the patients. 31
Given the complexity of the diagnosis and the lack of consensus, the first norms for diagnosis and treatment of BE were recently published by the Spanish Society of Pneumology. 33
Investigation into specific causesThere are various causes that must always be ruled out when dealing with a situation of BE of unknown origin, due to the consequences it will have in the approach and treatment of patients.
Cystic fibrosisCF is the most frequent autosomal recessive hereditary disorder in white people.
A diagnosis of CF is rather important as it is a disease with very well defined clinical, microbiological and therapeutic monitoring strategies. Compliance with the latter leads to important benefits for the patient, namely in terms of life expectancy. In addition it also has implications for genetic counselling in family planning.
In 1998 the criteria for diagnosis were defined 34 (Table 1).
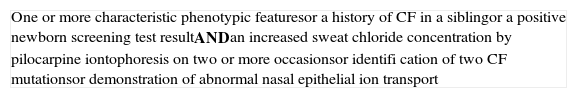
Criteria for the diagnosis of CF
| One or more characteristic phenotypic featuresor a history of CF in a siblingor a positive newborn screening test resultANDan increased sweat chloride concentration by pilocarpine iontophoresis on two or more occasionsor identifi cation of two CF mutationsor demonstration of abnormal nasal epithelial ion transport |
For many decades CF was considered a children's disease. In 1970 the average life expectancy was 16 years of age. 35 In spite of the average age of the diagnosis in the USA being 6 months of age, the actual interval ranges between 0 and 80 years of age. 36 In the last three decades the number of adult patients has increased. A fundamental reason for this situation is the increase in the life expectancy of patients, which currently is around 37.4 years. 36 Another reason comes from the vast heterogeneity of clinical manifestations of CF, secondary, in part, to the large variety of mutations of the gene responsible for the disorder (1,604 mutations). 37–39 As a consequence of these findings, CF is currently subdivided into two large groups: typical or classic CF and atypical or non-classic CF. 40 The latter is characterized by pancreatic sufficiency, pulmonary disorder of minor severity, and intermedíate to normal values on sweat tests. 40
Most patients diagnosed with CF after the age of 18 are diagnosed because of respiratory symptoms, male infertility, or in some cases because of recurrent pancreatitis. Individuals diagnosed during the adult years have greater diversity of mutations, less serious lung disease, higher rates of pancreatic sufficiency, less growth of Pseudomonas aeruginosa and Burkolderia cepacea and higher rates of infections by atypical mycobacteria, Staphylococcus aureus and allergic bronchopulmonary aspergillosis (ABPA). 41–44 Pancreatitis is the only most common complication. 41
In a retrospective study, it was noted that of the 601 adults with diffuse BE, 46 (7,6 %) were diagnosed with CF. The mean age of these patients was 31 (18-56) years. Sixteen patients had a severe lung disorder (VEMS < 40 %), with symptoms that they had had since childhood. Until the diagnosis was confirmed it was thought that they had asthma, chronic bronchitis or BE of unknown origin. In 20 % of the cases, it was noted that the sweat test alone was not sufficient to make a diagnosis. In 22 % genetic study was also not sufficient, but when both tests were done all patients except for one, were diagnosed, in which the nasal potential differential confirmed the CF. 44
In consequence of all of these studies, one concludes that the sweat test must be included in the aetiological investigation of BE of unknown origin, even in adult patients. The genetic study in conjunction with the sweat test increases the diagnostic probability, but many times it is still necessary to broaden the study to be able to identify mild and less frequent mutations.
Non-tuberculosis mycobacteria infectionsThe relationship between non-tuberculosis mycobacteria (NTM) and BE is still, in part, unknown because in some cases the infection is a consequence contributing to the development of the disease, while in others it can be considered a cause.
Very little information has been published about the prevalence and the meaning of NTM in non-CF BE. Mycobacterium avium complex (MAC) is the predominant species, regardless of the BE aetiology, both in single and multiple isolates, as opposed to patients with atypical mycobacteriosis without BE. 45,46 However, it is not uncommon to isolate more than one species. 45 A considerable percentage of isolates occurs in the routine sputum cultures (28 %). 46
Lung infection due to MAC was initially detected in older men, with smoking habits and COPD - apical fibrocavitary disease (Table 2). 47
Characteristics of apical fi brocavitary disease
| Generally progressiveComplication of other pre-existing lung disease (COPD, BE, pneumoconiosis, tuberculosis-related lesions)Cavitation and thickening of the pleura are commonTreatment is frequently requiredBE occurs in areas where the disease is more severe |
In 1989, Prince et al described a series of patients with lung disorder due to MAC without any apparent predisposing factors, predominantly in females (81 %), that were elderly and that showed a fibronodular radiological pattern (76 %). 48 In 1992, Reich and Johnson described 6 cases of lung disorder due to MAC, all in female patients, with a mean age of 65, with no clinically evidence of past lung disorder, with initial involvement of the periphery and the dependent portion of the middle lobe (ML) and/or lingula. 49 Admitting that women consider coughing as a socially unaccepTable behaviour, these authors defined this new pattern as “Lady Windermere syndrome”. The mechanism of volunteer suppression of cough would lead to the development of obstructive pneumonitis, pulmonary fibrosis or BE in the ML/lingula, as these 2 lobes require a more effective cough to eliminate secretions. This disease is currently called nodular bronchiectasis disease (Table 3). 47,50–53 It is more frequently associated with MAC but can also be secondary to M. abcessus, M. chelonae, M. simiae and M. kansasii (and probably other species). 47 The evolution of the disease is variable but tends to be more chronic and insidious. Therefore, it is sometimes necessary to provide follow-up for months or even years until the diagnosis can be confirmed. 47 The most frequent symptom is a chronic cough, usually productive. In cases of extensive disease, the constitutional symptoms, such as fever, malaise, night sweats, fatigue and weight loss are common. 50,55 The most common characteristics of HRCT, regardless of the isolated NTM, are multiple small nodules (< 1 cm), followed by cylindrical BE and “tree-in-bud” pattern, predominantly in the ML, lingula and dependent areas of the lung. 47,55 This combination features a sensitivity of 80 % and a specificity of 87 % in the diagnosis of this infection. 56 The nodules can precede BE but frequently they appear together within the affected areas. 54
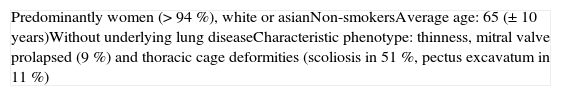
Characteristics of nodular bronchiectasis disease
| Predominantly women (> 94 %), white or asianNon-smokersAverage age: 65 (± 10 years)Without underlying lung diseaseCharacteristic phenotype: thinness, mitral valve prolapsed (9 %) and thoracic cage deformities (scoliosis in 51 %, pectus excavatum in 11 %) |
Several explanations have been advanced for the development of the nodular bronchiectasis disease. Reich and Johnson considered anatomic (long and narrow ML/lingular bronchi) and social (voluntary inhibition of cough) reasons, as possible explanations, respectively, for the predominance of changes in the ML/lingula and in women. 49 Other authors look at pulsating heart as a possible cause for rarefaction and distortion of the parenchyma of the ML/lingula, in patients with a mild deficit in the connective tissue. 57 The onset of symptoms in post-menopausal women also suggests the involvement of sexual hormones. 53
In most of these possible explanations, the underlying idea is that the causal mechanism lead to the development of BE which then creates a predisposition for mycobacterial infections. However, in studies correlating the radiological changes and the histopathological findings, it has been shown that the small nodules can coalesce and lead to ectatic changes and that the bronchial wall can also be damaged due to inflammation, with or without the formation of granulomas, at the peribronchial and bronchial areas. These changes demonstrate the invasion of tissue by the NTM and show its potential for developing bronchiectasis. 46,58 Another result that favours the pathogenic role of NTM, is the HRCT findings showing the increasing severity of BE, as well as the formation of new BE areas as the disease spreads. 56
Several recent studies have shown that the CF diagnosis (20 % vs 2 %) 45 or the presence of the CFTR (36.5 %) 53 are more common in patients with atypical mycobacteriosis in comparison to patients with negative cultures. Therefore, patients with multiple bacterial isolations must also be carefully assessed to rule out CF.
Primary humoral immunodeficiency — Selective antibody deficiencyThe prevalence of primary humoral immunodeficiency (PHI) is of approximately 1:25,000. 59 This value is probably grossly underestimated due to underdiagnosis and because some patients die before the diagnosis is confirmed. PHI corresponds to around half of all primary immunodeficiencies and the main clinical manifestations are recurrent bacterial infections of the upper and lower respiratory tract. 59,60
The delay in the diagnosis of PHI, in spite of the usual presence of chronic respiratory symptoms, remains a current problem associated to structural lung damage. In 95 % of the cases the symptoms appear after 6 years of age and reach a peak in the 3rd and 4th decades of life. 59
Several studies reported BE prevalence levels between 17 % and 76 %. This variation can be justified, in part, by the delay in beginning treatment. In most cases there is a description of cylindrical BE, predominantly in the ML and lower lobes. 59
PHI is divided into 2 groups: those that are secondary to a defined genetic disorder (e.g. X-linked agammaglobulinemia, automosal recessive agammaglobulinemia) and those of unknown genetic base. This later comprises the largest group and includes the variable common immunodeficiency, IgG subclass deficiencies, IgA deficiency and selective antibody deficiency. 60 The first group of diseases appears mainly during childhood and the second group appears later on. Thus, it is important that in an adult with BE of unknown origin and recurrent respiratory infections, the immunoglobulins (Igs) levels and subclasses be assessed. However, this is not enough to diagnose selective antibody deficiency, as it presents with normal or nearly normal IgG serum levels, including IgG subclasses, but has a deficiency response to polysaccharide antigens. 60 The diagnosis implies immunization with a non-conjugate pneumococcal polysaccharide vaccine (e.g. Pneumo 23®). Measuring the titers up to 14 serotypes, both prior to and 3 to 4 weeks following vaccination 60,61 is recommended. Some authors defend the simultaneous assessment of response to the conjugate vaccine for Haemophilus influenzae, as it was noted that there are normal individuals who do not respond to the non-conjugate polysaccharide vaccine. Therefore, the assessment of the response to the two vaccines will lead to greater precision in diagnosing the true nonresponders. 62 Selective antibody deficiency has been associated with recurrent sinopulmonary infections and BE. 62,63 In an investigative study carried out on the causes of BE, practically half of the primary immunodeficiency cases were caused also by this syndrome. 26 In another study, 11 % of BE patients, where the primary causes had been ruled out, there was a deficiency in the production of specific antibodies for S. pneumoniae and H. influenzae. 62
Determining a vaccine response is not a routine examination but must be carried out on BE patients, where other known causes were ruled out, especially on those with a history of otitis media and low IgG2 levels. 62,64
In conclusion, the functional assessment associated to the serum quantification of Igs must be included in the BE diagnostic algorithms. 33
Primary ciliary dyskinesiaIn most cases primary ciliary dyskinesia (PCD) is an autosomal recessive disorder, relatively rare, with an estimated prevalence of 1:15-30,000. 65 This value is probably higher as the disorder is commonly underdiagnosed. 66 It is caused by a large variety of ciliary disorders thus resulting in a vast clinical array of symptoms. If the disease does not present the usual aspects, namely situs inversus, the diagnosis may be delayed or might not even be made. 67
To date, were identified only 2 disease-causing mutations in genes that encode outer dynein arms (DNAI1 and DNAH5). 68 An adequate clinical history is sometimes sufficient to consider the PCD diagnosis. Typically, rhinitis or nasal congestion starts on the very first day of life, it is constant and treatment is difficult. Current data allow us to state that 50-75 % of PCD patients present significant respiratory symptoms immediately upon birth. 68 The situs inversus occurs in approximately 50 % of the cases and when associated with BE and sinusitis it is designated as the Kartagener syndrome. Other aspects that should alert one to the presence of PCD are chronic productive cough, atypical asthma, BE, daily rhinitis, serious chronic sinusitis and chronic otitis media. BE is predominant in the ML and in the lower lobes. 67 Nasal polyposis is rare. Approximately 50 % of men are infertile and women present with subfertility and a greater risk of ectopic pregnancy. 65,66
In a study of 47 adult patients, with well defined ultrastructural disorders, the following changes were observed: cough (100 %), BE (98 %), otitis media (92 %), history of neonatal respiratory symptoms (65 %), sinusitis (47 %) and situs inversus (46 %). 67
There are various works that suggest that early diagnosis can prevent the development of BE and the subsequent decline of the pulmonary function. The confirmation of the diagnosis should imply monitoring and an approach similar to that recommended for CF. 65
The definitive diagnosis is based on the ultrastructural ciliary exam of ciliated epithelium, which is expensive and very specific. 65 The saccharin test was the only screening test available for some years but it is not very precise and is difficult to perform on small children. Over the last few years several works have been published demonstrating that exhaled nitric oxide (FeNO) and nasal NO is very low in PCD, specially the nasal NO (10-20 % of the normal values). 67,68 The underlying pathophysiologic mechanism is unknown. Low values are also associated with some CF cases, serious rhinosinusitis of infectious or allergic origin, nasal polyposis and diffuse panbronchiolitis. 66,68 The sensitivity and specificity of nasal NO in PCD vary between 89-100 % and 97-100 %, respectively. 69,70 Nasal NO is currently a good and feasible screening test.
A sample of ciliated epithelium can be obtained via nasal brushing. The patient does not need to be hospitalised, it takes mere seconds, discomfort is minimum and only occasionally does it cause a minor epistaxis. 65 Over the last few years, with the appearance of high speed digital video photography, it was demonstrated that different ciliary beat patterns are related to specific structural changes and 10 % of the patients present normal beat frequency but dyskinetic beat pattern. 66 PCD can only be ruled out if the beat frequency and beat pattern of the cilia are normal. If only one of the parameters is altered it will be necessary to carry out an ultrastructural assessment via electron microscope. To rule out secondary ciliary defects, the treatment has to be intensified before collecting the sample and, if deemed necessary, the exam should be repeated some months later. 66
Similarly to CF, milder phenotypes of PCD, resulting from ciliary dysfunction and subtle or unapparent structural disorders, will probably appear. 68
Alpha-1 antitrypsin deficiencyThe deficiency of a1-antitrypsin (AAT) is mainly associated to the development of emphysema, in youngsters. Other alterations can also occur, namely BE. In a recent study of 74 patients with serious deficiency of AAT (phenotype PiZ) the radiological presence of BE was reported in 70 patients, 27 % of which had clinical significance (chronic sputum and involvement of ≥ 4 segments). In most patients BE was of cylindrical or cylindrical-varicose type. The distribution of BE, in general, was the same as that of emphysema, predominating in the lower lobes. It was noted that patients with frequent production of sputum had more serious BE and greater bronchial wall thickening. However, the severity of the disease normally reflected the severity of the emphysema but, in some cases, serious and sometimes cystic BE coexisted with relatively mild emphysema. 71 There are other descriptions of cases in which the predominant or exclusive radiological alteration of AAT deficiency is BE. 72–74
The explanation for the presence of BE in patients with AAT deficiency is still not totally clear, but the concordant distribution of BE and emphysema with greater severity suggests a common pathogenic mechanism or an interaction between the inflammatory processes associated with each entity. 71
Although the association between BE and AAT deficiency has not been firmly established, the standards for the diagnosis and management of individuals with AAT deficiency, published in 2003, by ATS/ERS, recommend quantitative testing of AAT in individuals with BE without evident etiology. 75 Accurate diagnosis is important because of the possibility of using AAT augmentation therapy, according to the criteria published, 75 and for the optimization of the therapeutic strategy of patients with AAT deficiency and BE.
Diffuse panbronchiolitisDiffuse panbronchiolitis (DPB) is an idiopathic inflammatory disorder mainly identified in adults in Asia, namely in Japan. However, since the end of the 80's there are some cases and small series described in western countries. It normally occurs between the 2nd and 5th decade in life and 2/3 of the patients are non-smokers. 76
The cause is unknown but the predominance of the disease in Asian individuals suggests genetic predisposition. 76,77
Initially the patients present with cough and profuse purulent sputum, followed by exertional dyspnea which progressively worsens. Over 80 % of the patients have chronic pansinusitis. 76,77 The pathogen which initially is most frequently isolated in sputum is Haemophilus influenzae and, as the disease develops, colonization by P. aeruginosa is common. 76,77
The most common laboratory alteration is the persistence of high cold agglutinins. The nasal NO is characteristically low in patients with DPB. 76,77
The HRCT findings are quite characteristic, consisting of centrilobular nodules, thickened and ectatic bronchioles and peripheral air trapping. The centrilobular nodules are not well defined and have a diameter of < 5 mm; some of these nodules are linked to distal ramified structures that represent bronchioles filled with secretions (“tree-in-bud”). In the later stages are observed bronchiolectasis (cystic dilations of the nodules) and BE. These alterations are disperse but are more significant in the lower lobes. 77
The typical histological features are the prominent involvement of the respiratory bronchioles, with transmural and peribronchial infiltration by lymphocytes, plasma cells and histiocytes. Most of the histiocytes appear as foamy macrophages and the accumulation of the latter, in the wall of the respiratory bronchioles and in the interalveolar septa, represent a histological feature practically exclusive to DPB.76
Without treatment the mortality rate at 5 and 10 years of age is 33.2 % e 62.1 %, respectively, however, treatment with a daily dose of 600 mg of erythromycin, for 2 years, has a curative effect. 76
Even though DPB is more common in Asia, this disorder should be included in differential diagnosis of sinopulmonary disorders, progressive bronchiolitis, BE and progressive obstructive pulmonary disease of unknown etiology. 78,79
Allergic bronchopulmonary aspergillosisABPA is an immunologically mediated lung disorder caused by hypersensitivity to Aspergillus antigens, especially A. fumigatus. The two pathologies which are most frequently associated with ABPA are asthma and CF, with an estimated prevalence of 1-2 % and 2-15 %, respectively. 80,81 There are, however, some cases reported in individuals without asthma or CF, with intermittent asthma (bronchospasm induced by exercise) 81 or asthma during childhood. 82 Most diagnoses occur during the 3rd-4th decade of life. 80
The development of ABPA can precede its diagnosis by many years or even decades and is many times confused with other lung disorders. 80
The diagnosis is based on 5 minimum criteria (Table 4). There are authors that consider the cut-off for total IgE to be > 1,000 kU/L and others > 417 kU/L (equivalent to 1,000 ng/ml). This last value can lead to an overdiagnosis of ABPA. 80 Other common aspects are peripheral eosinophilia, precipitin for A. fumigatus, the elimination of brownish mucous plugs and the presence of migrating pulmonary infiltrates during exacerbations. Although any area of the lung can be affected, the upper lobes are the most affected. 80,81
The most common symptoms are coughing and dyspnea, followed by sputum, wheezing, low-grade fever and haemoptysis. There are also cases of patients featuring few or no symptoms at all. 83
Currently there are two ABPA groups: central ABPA-BE and seropositive ABPA. The first group corresponds to cases in which on the HRCT one can see central or proximal BE, that is, BE in the inner 2/3 of the lung and normal peripheral bronchi and the second group comprises patients that satisfy ABPA criteria, but without BE. It is believed that the latter group corresponds to cases that are in an earlier or milder phase of the disease. 80,81 The response of the host to Aspergillus in the bronchial mucus can be an important factor in the development of BE in some patients, but not in others. 84 BE is characteristically central, but 40 % of the bronchioectatic segments extend out to the periphery. 80 The presence of BE indicates a poor prognosis in the normal course of ABPA. 80
Various stages of the disease were described but the latter do not correspond to disease phases because the patient does not necessarily progress from one stage to another. Stages I, II and III correspond to worsening, remission and exacerbation, respectively. Stage IV corresponds to glucocorticoide-dependent asthma or ABPA and stage V to a fibrocavitary disorder similar to pulmonary tuberculosis or to advanced stages of CF, with extensive BE. 80,81
It has already been noted that early diagnosis and treatment of ABPA prevents the disease from progressing to stage V. 81 A diagnosis made in a beginning stage, if possible prior to the development of BE (ABPA seropositive), can prevent the development of a clinically and radiologically serious disease. 84
ConclusionsBE has been considered an orphan disease, but recently it has begun to awaken more interest. Instead of being a disease on its way to extinction, it has gradually increased in importance, ever since it became known that its presence aggravates the prognosis of the underlying disease, accelerates the loss of pulmonary function, increases mortality, and significantly reduces quality of life. 85,86
A systematic investigation of the underlying aetiology in all BE cases is very important, especially in those that have more specific treatment. 87 In order to carry out the most effective tests, the initial assessment must be oriented by the clinical and family history.
Some of the disorders described, such as CF, PCD and IDP, are typically considered children's diseases, so a diagnosis in an adult patient is more complex and requires greater clinical suspicion.
The importance of diagnosing the abovementioned pathologies is related to treatment specificities, the subsequent prognoses, and in some cases, to the giving of genetic counselling.
The better the description of BE patients, the more we will be able to define the idiopathic BE group, and thereby have a greater probability of investigating possible underlying mechanisms within this group.
The publication of diagnosis and treatment regulations by the Spanish Society of Pneumology in 2008 demonstrates the growing interest in this pathology. This initiative should lead to reflection on the current approach to this issue and contribute to the effort to reverse the lack of interest so characteristic of the last few decades.
Conflict of interestAuthors state that they don't have any conflict of interest.