We report a clinical case of severe malaria, where the rate of initial parasitaemia by Plasmodium falciparum was 43 %.
Multiple organ dysfunction, including ARDS, forced admission in a close surveillance unit, with survival of the same.
A brief review of the subject is made, focusing on severity and general conduct, alerting and awareness for this entity, whose expression, among us, could take on increasing importance.
Apresenta-se o caso clínico de um doente regressado de Angola com malária grave, em que o índice de parasitémia inicial pelo P. falciparum era de 43 %.
Disfunção múltipla de orgãos, incluindo ARDS, implicaram o ingresso do doente numa unidade de alta vigilância, com sobrevivência do mesmo.
Faz-se uma breve revisão do assunto, com enfoque nos indicadores de gravidade e na conduta geral, alertando e sensibilizando para esta entidade, cuja expressão, entre nós, poderá vir a assumir importância crescente.
Malaria is caused by the protozoa Plasmodium, 1 with an intra and extra erythrocyte life cycle, and man is infected by the bite of the anopheles mosquito. There are four species responsible for human malaria: Plasmodium falciparum, P. vivax, P. ovale and P. malariae.
Most cases of imported malaria are caused by P. falciparum. It is characterized by fever, chills, intense sweating and headaches, that arise between the 9th and 14th days after bite. Incubation can last for months.
With postponed diagnosis erythrocyte parasitemia may reach critical values, massive hemolysis and multiorgan dysfunction resulting in death.
The pulmonary involvement with edema is a major complication. 2 More common in adults, is more severe in pregnant and non-immunized individuals. 3 The alveolar-capillary barrier suffers increased permeability and alveolar flooding, conditioning acute lung injury/acute respiratory distress syndrome (ARDS). 4
Case reportMan, 44 year old, black, born in Angola and resident in Portugal for 24 years, where he works in building construction.
Medical and surgical history irrelevant. Denies alcohol or smoking habits, illicit drug use or sexual risk contacts. He had returned from Angola two weeks ago from his first trip there, without taking any precaution.
He recurs to the emergency room with fever (40ºC) and general malaise of a week duration, and watery stools since the last three days.
He presented with a reasonable general condition, dry mucous membranes and icteric sclerae. A hypotensive and tachycardic profile was noted, while being apyretic with good peripheral saturations on ambient air.
No obvious focus of infection was detected and the rest of the objective examination was irrelevant.
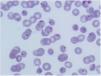
Initial laboratory parameters was as follow: hemoglobin 11.9g/dL, WBC 7,200/μL, platelets 27,000/μL; normal ionogram and renal function, mild liver cytolysis without hyperbilirubinemia, LDH 693 U/L, C-reactive protein (CRP) 228.9mg/dL. Positive thick smear for Plasmodium with 43 % of parasitemia (Fig. 1).
Therapy was started with quinine sulfate and doxycycline.
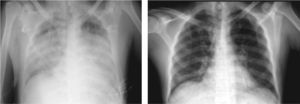
Infection with hepatotropic virus, HIV I/II, intestinal parasites, urinary tract infection, bacterial gastroenteritis or bacteraemia was excluded. The chest radiograph shows no abnormality.
On the 3rd hospital day (D3), the patient became more obtunded, pale, dehydrated, and more icteric with profuse sweating, fever, tachypnea and hemodynamic instability. On pulmonary auscultation there was new bilateral inspiratory crackles.
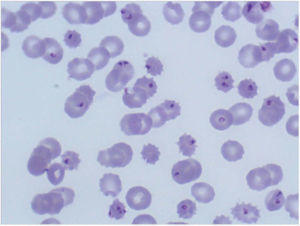
Hemoglobin fall to 6.8g/dL accompanied by hyperbilirubinemia, LDH = 801 U/L, haptoglobin < 7mg/dL, thrombocytopenia (37,000/μL), creatinine 1.7mg/dL and mild hyponatremia. The CRP remained high and procalcitonin reached 42.6mg/dL. Plasmodium on direct examination was negative. The characterization of the agent trough the BinaxNOW® test showed a single antigen band for P. falciparum.
The patient was admitted to a High-Dependency Unit (HDU), with multiple dysfunctions, including cardiovascular, hematological, renal, hepatic and respiratory systems (PaO2/FiO2 = 129) with criteria for ARDS (Fig. 2). After attempts was made to exclude secondary septic complications, to the general support measures, which included liberal fluids infusion and transfusion of packed red blood cells, an empiric antimicrobial coverage with linezolid plus piperacillin/tazobactam was instituted.
By D7 the clinical situation allowed us to continue treatment in the general ward. On D8, a clear improvement on radiological findings and gas exchange was noted. The microbiological screening remained negative, and so, we proceed therapy with only quinine sulfate.
By D11 hemoglobin was 9.2g/dL, with no leukocytosis or thrombocytopenia, and renal function, bilirubin and CRP normalized or continued to improve. Plasmodium on ticks mear remained negative. Abdominal ultrasound excluded pathologic findings.
The patient lived the hospital with a good general condition, with permanent apyrexia and without need for oxygen supply. On a subsequent ambulatory revision, a completely normal clinical status was verified.
Discussion and conclusionsMalaria presentation is very unspecific so alternative and more frequent diagnoses should be excluded, such as severe pneumonia, meningitis, hemorrhagic fevers, salmonellosis, viral hepatitis and dengue. Fever is common and should be treated with paracetamol, to minimize bleeding diathesis. It responds poorly to antipyretics and physical measures can be necessary.
Imported malaria, in the beginning rarely follows the classical pattern of tertian or quartan fever, which appears only after a few cycles when synchronization occurs. Additional symptoms include chills, headache, malaise, nausea, vomiting, diarrhea, abdominal pain and myalgia. Splenomegaly is an inconstant finding. In practice, malaria should be suspected in any febrile individual returning from tropics, especially if coexisting anemia, thrombocytopenia or cytolysis.
10 % of all cases have a malignant evolution. These are mostly induced by P. falciparum and may follow a explosive course with 50 % of deaths occurring in the first 24 hours. 5
Diagnosis is made by direct demonstration of parasites in blood. Parasitaemia should be determined initially, at D3, D7 and D28, to assess severity, therapy monitoring and late failures detection. 6
Agent detection can imply repeating tests at 12h intervals, but is generally accepted treating patients empirically if suspicion remains high.
Malaria is a paradigmatic example where the early therapy and intensive monitoring brings benefits.
ARDS is defined by acute onset of bilateral pulmonary infiltrates in the absence of heart failure and a PaO2/FiO2 ≤ 200mmHg.
The absence jugular engorgement, hepatojugular reflux, peripheral edema and the typical “butterfly” infiltrates and cephalic pulmonary blood redistribution on chest x-ray, don't support cardiogenic edema. These parameters helped us to guide the fluids supplementation, without jeopardize gas exchange. However, alveolar-capillary damage really favors pulmonary edema formation.
Non-cardiogenic pulmonary edema rarely occurs with other species then P. falciparum.
Quinine sulfate is the drug of choice for severe malária, but caution should be taken in those patients with a family history of sudden death or long QT by its intrinsic arrhythmogenicity. Glocunato form is even more pro-arrhythmic.
Severe and recurrent hypoglycemia can result from hyperinsulinism induced by quinine/quinidine, malarious toxins or massive parasitism.
Renal failure, usually oliguric, rarely requires dialysis support and reverses in days.
Thrombocytopenia is common, but rarely contributes to hemorrhagic diathesis. Anemia is induced by parasitic hemolysis.
The fever increases during the first two days but should disappear after 48 hours of treatment.
The efficacy of treatment must be verified by microscopic examination of the blade. The degree of parasitaemia decreases 90 % in 48 hours and must be zero at D3.
The actual case illustrates the counsequencies of preventive measures failure, such as chemoprophylaxis.
If a parasitaemia score of 5 % reflects severity, the 43 % presented by out promised a complicated evolution, as was the case with the installation of successive failures that culminated in ARDS.
The inability to microscopically characterize the type of Plasmodium, do limited therapy institution. Results of the BinaxNOW® test, showing a single band for P. falciparum antigen, comes later. Genomic identification by polymerase chain reaction (PCR) is another available mean to identify the Plasmodium.
Compared with PCR, BinaxNOW® test showed a sensitivity of 94 % for detection of P falciparum and 84 % for other species, with overall specificity of 99 %.(7,8)
Multiorgan dysfunction, led us to admit secondary sepsis superposed on malaria, influencing the strategy.
Despite severity of the condition and the limited clinical experience, admission to a HDU capable of monitoring and early warning to complications, associated with elected conduct, proved critical to reverse the various dysfunctions, allowing the avoidance of mechanical ventilation.
Although relatively rare in Portugal, the clinical picture of malaria tends to change with progressive flow of people between countries with multiple affinities, as is the case of Portugal with African ex-colonies.
- Home
- All contents
- About the journal
- Metrics
- Open access