Primary sarcomas of the lung are uncommon, potentially aggressive neoplasms that need to be distinguished from other malignant pulmonary tumors and whose biological behavior is as yet not fully understood.
Primary undifferentiated pleomorphic sarcoma was diagnosed in the right lung of a 66 year-old man, who has survived over 11 years after treatment with endobronchial tumor debulking by laser therapy and radiotherapy.
Os sarcomas primários do pulmão são neoplasias raras e potencialmente agressivas, que devem ser distinguidos de outros tumores pulmonares malignos e cujo comportamento biológico não está completamente esclarecido.
Os autores apresentam um caso clínico de sarcoma pleomórfico indiferenciado do pulmão, que foi diagnosticado a um homem de 66 anos. Na altura do diagnóstico foi realizada desobstrução brônquica por laser e radioterapia, posteriormente foi observada uma sobrevivência superior a 11 anos.
Primary sarcomas of the lung are rare, accounting for less than 0.5 % of lung malignancies, and their classification is not consensual in the literature, largely due to changes in terminology and in diagnostic criteria that have taken place since the advent of immunohistochemistry.1–5
Because of their rarity, the treatment of these tumors is not standardized; although complete surgical removal confers the best length of survival. 1 Tumor size and grade are additional factors that may influence the outcome.6
Case reportA 66 year-old retired painter and bricklayer, who had recently given up smoking (smoking history of 132 pack per year), presented in August'99 with complaints of cough with purulent sputum, hemoptysis, dyspnoea and fever that did not improve with a course of antibiotherapy.
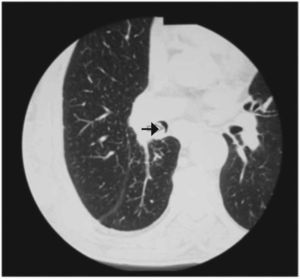
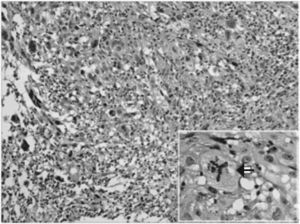
His general condition was good, but he had reduced lung sounds in the lower third of the right hemithorax. The PaO2 in room air was 73mmHg. Chest X-ray showed an opacity in the lower right hemithorax, and CT scan revealed an endobronchial mass causing obstruction of the lumen of the inferior lobar bronchus (Fig. 1), with an irregular, approximately 3cm, extension into the lung parenchyma. Sputum cytology showed malignant cells and the histology of the endoscopic bronchial biopsy revealed a malignant tumor with sarcomatous features. There was no evidence of tumor elsewhere on abdominal and brain CT scans and bone scintigraphy. The endobronchial tumor mass was subsequently removed with laser, and histological examination showed a spindle cell tumor with marked nuclear pleomorphism, multinucleated tumor giant cells and numerous mitotic figures (Fig. 2). There was no evidence of epithelial differentiation. The tumor was immunoreactive for vimentin and focally for CD68, and negative for multiple high and low mol. wt. cytokeratins, epithelial specific antigen, epithelial membrane antigen, actin, smooth muscle actin, desmin, S-100 protein and CD34. CD117 immunostaining showed no mast cells within the tumor. The cell proliferation index with Ki 67 was 60 %. A diagnosis of pleomorphic undifferentiated sarcoma was made.
Exploratory thoracotomy showed mediastinal invasion and radiotherapy was given to the tumor and mediastinum in a dose of 56 grays in 28 fractions, resulting in disappearance of the mass.
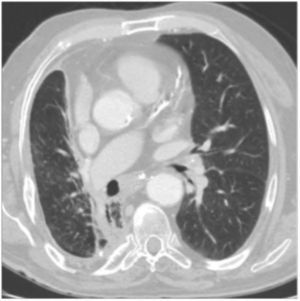
The patient has been followed-up regularly for the last 11 years, and has suffered recurrent respiratory infections recovering easily with antibiotherapy. Serial chest CT scans (Fig. 3), showed an unaltered diffuse density in the subcarinal and right hilar regions extending to the right pulmonary artery, thought to be scarring. The patient has refused to undergo further bronchial endoscopy.
DiscussionPrimary pulmonary sarcomas are rare tumors, representing about 40 % of "rare" pulmonary neoplasms and 9 % of all sarcomas.2 To date, approximately 300 cases have been reported in the literature.1 Sarcomas in the lungs can arise from pulmonary parenchyma, the bronchi or the pulmonary artery and its branches.2,3 They typically occur in middle-aged individuals with slight predominance in men. Prior history of radiotherapy or accidental exposure to radiation, confer greater susceptibility to the development of sarcomas. Symptoms and radiographic features are similar to those seen in other epithelial lung tumors and depend more on tumor localization than on their histological characteristics.2
Primary sarcomas of the lung present a considerable diagnostic challenge to both the histopathologist and the clinician. Litzsky 7 stresses two points; most malignant spindle cell tumors in the lungs will turn out to be carcinomas with sarcomatoid differentiation and sarcomas metastatic to the lung are far more frequent than primary sarcomas.
The lung presents all the common histological types of primary sarcomas seen elsewhere in the soft tissues. Changing terminology and histological criteria make it difficult to compare the incidence of different types of sarcoma. 1–7 Fibrosarcoma, a common sarcoma of the lung in earlier studies, 6 is no longer mentioned and fibrohistiocytic tumors such as malignant fibrous histiocytoma also thought to be common,4 are rarely encountered.2 The most common sarcomas now reported, are leiomyosarcoma, synovial sarcoma, malignant peripheral nerve sheath and vascular tumors.7
It is now accepted that along with morphological features, immunohistochemistry plays an important role in the classification, and the wide range of antibodies currently available means that entities previously diagnosed as fibrosarcoma, malignant fibrous histiocytoma and hemangiopericytoma have now been reclassified. Undifferentiated pleomorphic sarcoma, previously called pleomorphic malignant fibrous histiocytoma, is diagnosed only when no definable line of differentiation can be established,8 as in our case. Immunohistochemistry is also essential for ruling out the much more frequent pulmonary sarcomatoid carcinomas. In our case, antibodies to high and low molecular cytokeratins, epithelial specific antigen and epithelial membrane antigen ruled out sarcomatoid carcinoma, synovial sarcoma and diffuse malignant mesothelioma, a diagnosis that should be considered when the tumor involves the pleura or mediastinum.7 Synovial sarcoma is characterized by mast cells within the tumor,9 and none were detected in this tumor on staining with CD117. Smooth muscle actin, actin and desmin are seen in leiomyosarcoma, and the latter two in rhabdomyosarcoma, S-100 protein in malignant peripheral nerve sheath and liposarcoma, while malignant solitary fibrous tumor and malignant vascular tumors are immunoreactive for CD34, all of which were negative in our case. CD68, focally positive in our case and previously thought to be a marker for pleomorphic undifferentiated sarcoma (malignant fibrous histiocytoma), is no longer believed to be useful.8 All the tumors that were considered in the histological differential diagnosis are predominantly composed of spindle cells and express vimentin. The problem of overlapping immunohistochemical profiles seen in sarcomas is being addressed increasingly by turning to molecular genetic studies in these tumors.9
Sarcomas of the lung are histologically indistinguishable from metastatic sarcomas. Careful clinical and radiological examination is required to exclude a primary tumor elsewhere.5 In the long follow-up of our patient, no tumors have appeared elsewhere in the body.
Primary pulmonary sarcomas may have an aggressive progression.3 Surgical removal is the treatment of choice for all histological types, followed by radiotherapy of 50–60 grays in fractionated doses, if the removal is incomplete.1 Chemotherapy with doxorubicine and ifosfamid is advised only in metastatic or advanced sarcomas, but the response is less than 20 %.2
Local recurrence is frequent and is the main cause of death, while distant metastases are rare. The most relevant prognostic factors are tumor size at diagnosis, histological grade and complete surgical removal.1,6 Reported median survival for these tumors is 24–36 months. 1,5,6 However, with complete surgical removal of the tumor, this extends to 47 months.1 In a series of pulmonary leiomyosarcomas, high-grade tumors had a median survival of 5 months, 10 although one patient with a high-grade tumor was well 12 years after surgery. Another patient subjected a sleeve-lobectomy for a high-grade shwannoma was alive without recurrence after 25 years.6 Although our patient had a relatively small tumor, the histological type, and inability to carry out complete surgical removal should have suggested a poor prognosis. The response to radiotherapy is inconsistent in literature, with a few patients, usually those in whom complete tumor removal was achieved, responding well.1,6
We describe a patient with a primary undifferentiated pleomorphic sarcoma of the lung, whose tumor could not be resected, still alive after 11 years. This clinical case testifies to the importance of reporting primary sarcomas of the lung to improve the understanding of the biological behavior of this group of rare tumors.