Exercise-induced desaturation in chronic obstructive pulmonary disease (COPD) frequently has prognostic implications. Desaturation within the first minute of the walk 6-minute walk test will probably also occur in daily life activities and translate into hypoxaemic respiratory failure at rest in later years. This study aimed at comparing these patients with those who desaturate after the first minute and determine potential markers.
MethodsWe conducted a cross-sectional, retrospective study collecting data on respiratory function tests, cardiovascular comorbidity, body mass index, pack-year index, 6-minute walk test outcomes, BODE index, and Charlson comorbidity index. Patients who desaturated during the first minute of the test were referred to as early desaturators compared to the non-early ones.
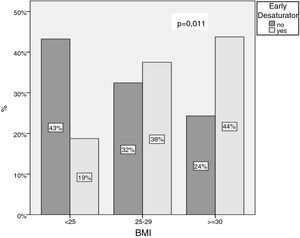
ResultsWe observed a higher mean body mass index in early desaturating patients, and an inverse relation as to the body mass index categories <25, 25–29, and ≥30. Early desaturators had a lower FEV1/FVC index. The mean distance walked in the test was shorter in early than in non-early desaturators, and they desaturated more deeply.
ConclusionOverweight and obesity, as determined by body mass index, seem to behave like markers for early desaturation. This simple anthropometric measure might indicate point to potential early desaturation in COPD patients.
Exercise-induced oxygen desaturation (EID) occurs in up to 20% of the patients with chronic obstructive pulmonary disease (COPD).1 However, despite being a relatively frequent condition, its definition has not yet been agreed upon.2–4 The most widely accepted criterion in common practice comprises a drop in oxygen saturation (SatO2) of more than 4% with a nadir of at least 88%. Although the pathophysiology of EID is a matter of debate, aspects such as the severity of airflow obstruction, a low CO diffusion capacity (DLCO), a high degree of emphysema, obesity, and a SatO2 at rest ≤93% have been related to it.5–8
Studies carried out by our group show that the decrease in the SatO2 curve during the 6-minute walk test (6MWT) has prognostic implications. Patients with such an event before the end of the first minute of the test, termed ‘early desaturators’ (EDs), had a high probability of also experiencing them during their daily life activities and of additionally developing hypoxaemic respiratory failure at rest within the subsequent 5 years compared to subjects who desaturated after 3min.9,10 Given the occurrence of the two desaturation profiles in patients with the same disease, the assessment of possible differential factors associated with this behaviour is imperative.
The purpose of this study was to characterise COPD patients with early desaturation versus non-early desaturation as well as determine potential markers that point to events of EID before the end of the first minute.
MethodsPatientsFrom a pool of 163 patients with COPD and exercise desaturation on the 6min walking test registered on our laboratory data base, 57 were not selected because they had interstitial disease, severe cardiac disease, domiciliary oxygentherapy. Then we conducted a cross-sectional study in 106 COPD (Table 1) patients, normoxaemic at rest but experiencing EID. The inclusion criteria were: aged over 40 years, active or former smoker with a pack-year index (PYI) >10 and a post-bronchodilator ratio of forced expiratory volume in one second (FEV1)/forced vital capacity (FVC) <70%, in addition to a basal SatO2 >90%. Patients with SatO2 at rest ≤90% or who were not able to correctly perform the 6MWT were excluded.
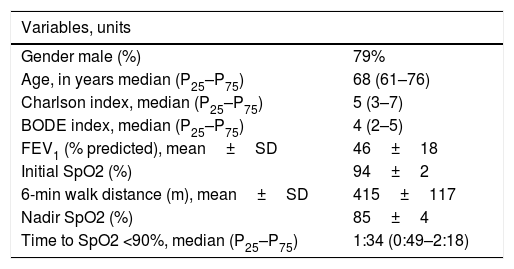
Baseline characteristics of patients with exercise-induced desaturation.
| Variables, units | |
|---|---|
| Gender male (%) | 79% |
| Age, in years median (P25–P75) | 68 (61–76) |
| Charlson index, median (P25–P75) | 5 (3–7) |
| BODE index, median (P25–P75) | 4 (2–5) |
| FEV1 (% predicted), mean±SD | 46±18 |
| Initial SpO2 (%) | 94±2 |
| 6-min walk distance (m), mean±SD | 415±117 |
| Nadir SpO2 (%) | 85±4 |
| Time to SpO2 <90%, median (P25–P75) | 1:34 (0:49–2:18) |
Data are given as median (25th, 75th percentile) or mean±SD (mean±standard deviation); FEV1: forced expiratory volume in 1s.
The following data from this descriptive, observational study was collected retrospectively from computerised medical records: age; sex; smoking history (active smokers if they had smoked at least one cigarette in the course of the foregoing 6 months; former smokers if they had maintained continuous abstinence for at least 6 months); smoking intensity by means of the PYI (defined as the number of packs of cigarettes smoked per day multiplied by the number of years as a smoker and divided by 20); body mass index (BMI) following the SEEDO11 criteria; dyspnoea (modified Medical Research Council [mMRC] scale); comorbidity (assessed by means of the Charlson index); BODE index; the associated cardiovascular risk factors arterial hypertension Type 2 diabetes mellitus, dyslipidaemia, and obesity; and finally cardiovascular diseases such as arrhythmia, ischaemic heart disease, and congestive heart failure. In addition, we recorded the results of the following pulmonary function tests: FEV1, FVC, FEV1/FVC, inspiratory capacity (IC), residual volume, total lung capacity, and lung diffusion capacity for CO (DLCO). Patients were stratified according to the four degrees of airflow obstruction collected in the 2009 GOLD (Global Initiative for Chronic Obstructive Lung Disease guidelines.12
The 6MWT was performed in a 30-m long corridor following the ATS/ERS13 protocol. Briefly, all tests were performed without supplemental oxygen and supervised by two observers, who instructed the patients to walk 6min along the corridor to complete as many metres as possible. Patients were allowed to stop if they had dyspnoea and resume walking when the symptoms had disappeared. The following variables were collected: initial and minimum SatO2, metres walked during the 6min of the test, as well as the point in time at which the SatO2 had come to the threshold of 90% (T90). EID was defined as a 4% drop in SatO2 from baseline, reaching a minimum of 88% or lower. Patients who desaturated during exercise within the first minute of the 6MWT were defined EDs and those who did so at a later point in time as non-early desaturators (NEDs).
Statistical analysisData were summarised as frequencies for categorical variables, as mean±SD for normally distributed data, and median (25th–75th percentile) for non-normally distributed outcome data. Comparisons between the groups ED and NED were explored using Pearson Chi-squared test, the Mann–Whitney U-test, and Student t-test as appropriate.
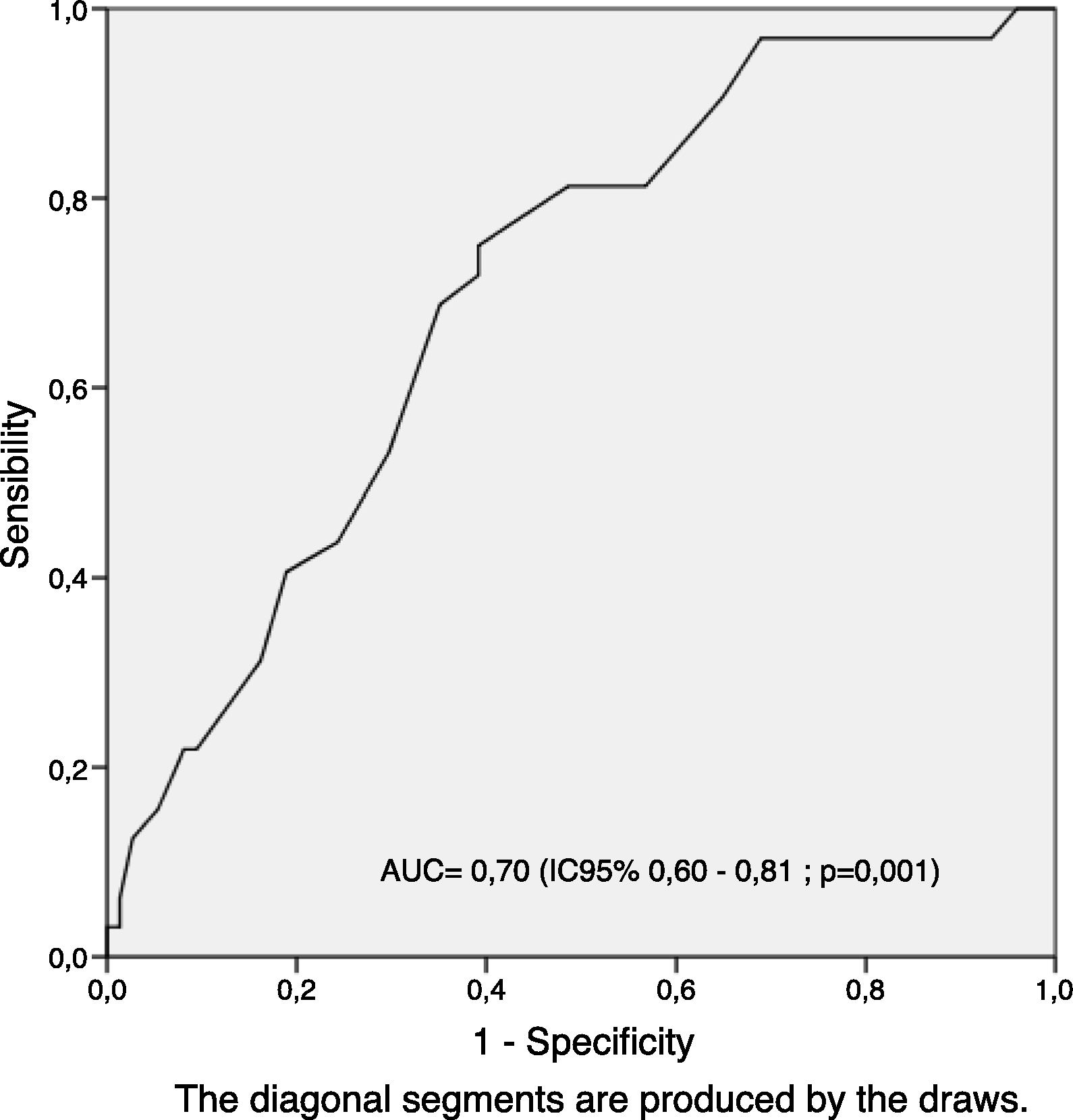
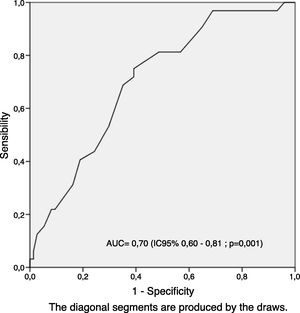
Differential patient characteristics before performing the 6MWT test were BMI and initial pulse oximetre saturation (SpO2) (Table 1). We applied multivariate logistic regression analysis, adjusted by initial SpO2, to determine the association between BMI and ED. Finally, to evaluate the discriminative capacity of the continuous BMI scale as a possible marker of ED, a receiver operator characteristic (ROC) curve was generated and the area underneath the curve (AUC) calculated.
The sample size (n=106) was estimated based on a frequency-of-outcomes factor of at least 20% of ED in the population with a confidence interval of 95% and a beta error of 20%. The significance level was established as p<0.05. All analyses were performed with the SPSS/PC statistical programme (version 21.0 for Windows; SPSS, Inc., Chicago, IL, USA). The study was approved by the ethics committee of the University Hospital Nuestra Señora de Candelaria (Tenerife, Spain).
ResultsSubject characteristicsA total of 106 patients were included in this study, all of them had COPD diagnosed and were staged as per GOLD guidelines. All patients desaturated either before or after the first minute of the 6MWT. The patients’ characteristics are reflected in Table 1. Most of them were men (ratio 4/1) with a median age of 68 years and a predicted FEV1 of 46%. The baseline oxygen saturation was above 90%. 93% of patients had moderate to severe airflow limitation and a high risk measured by BODE scale. Thirty two subjects (30%) were classified as EDs.
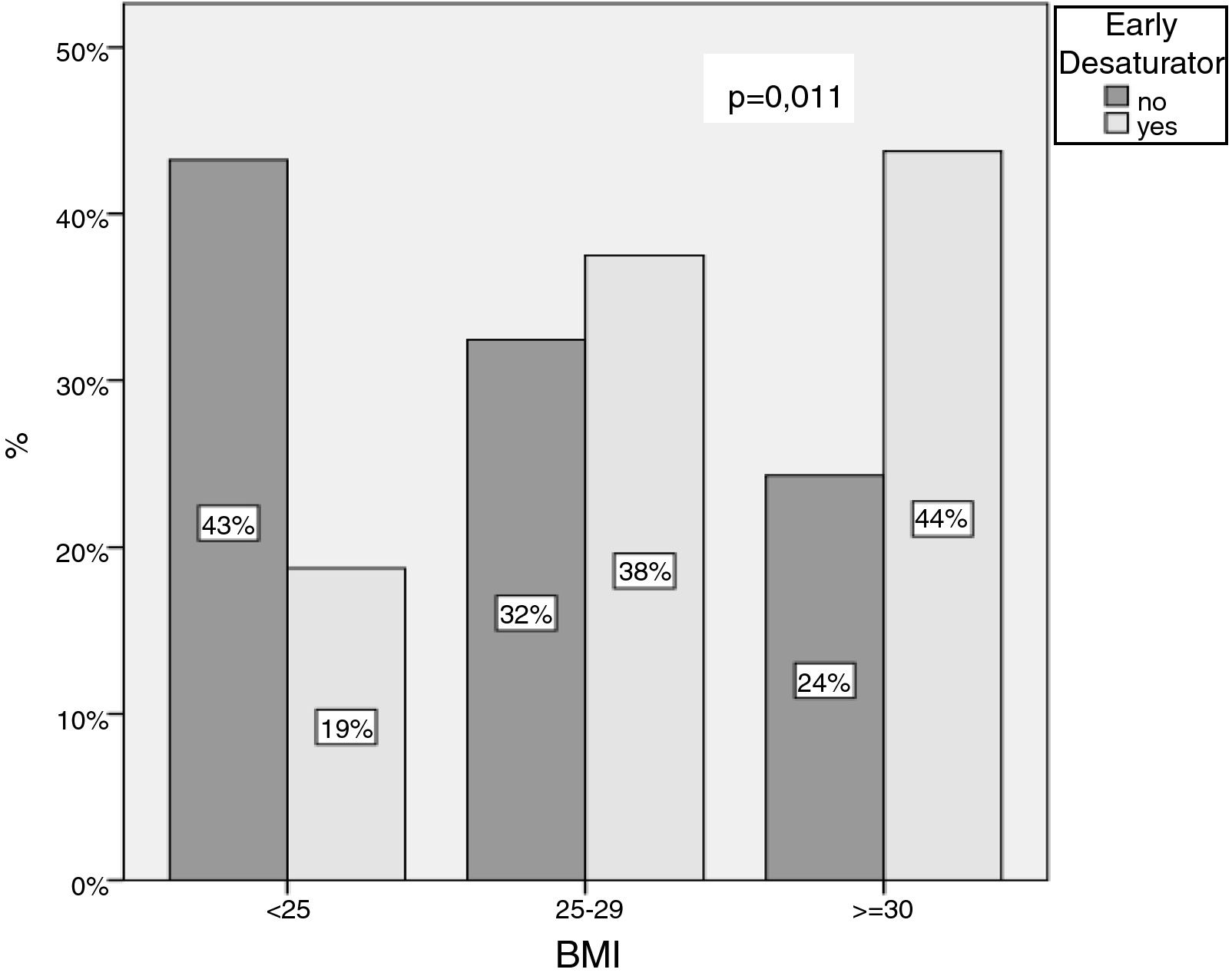
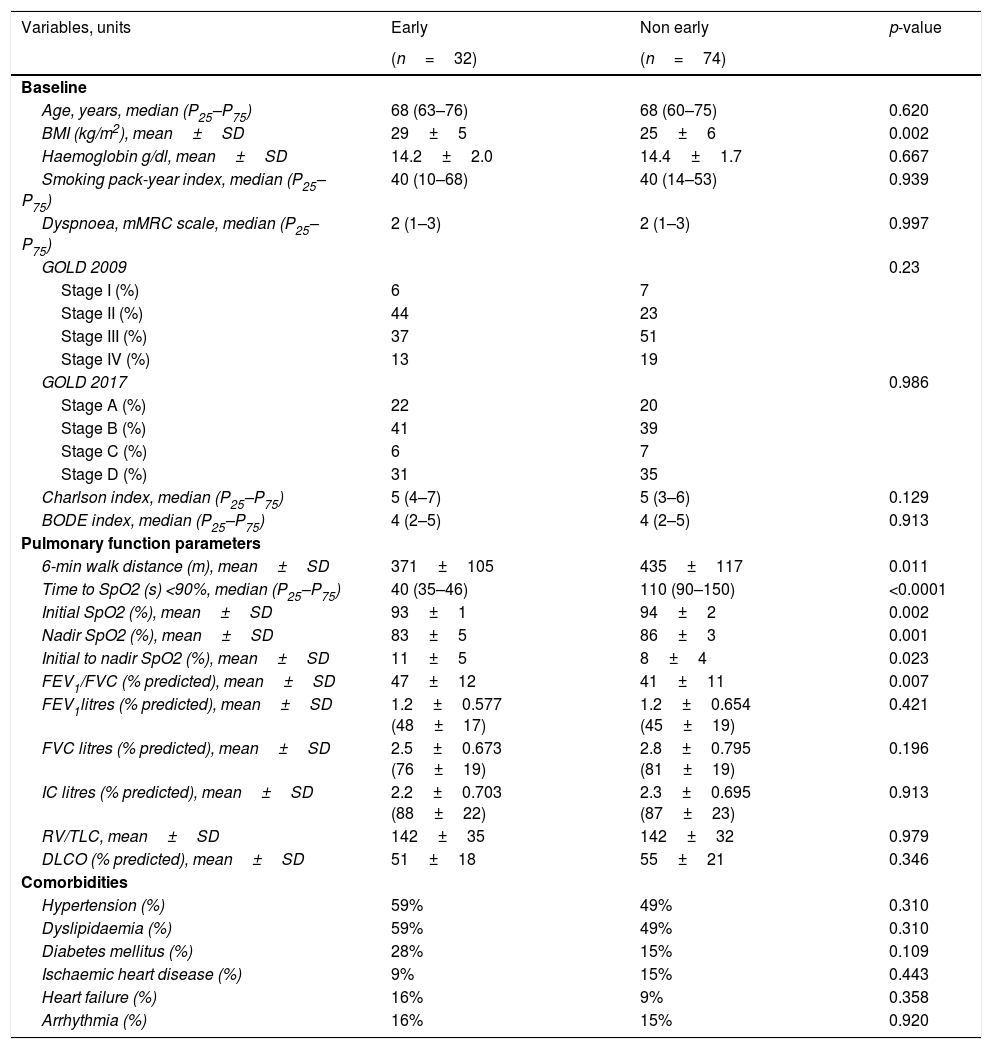
Differences between ED and NEDTable 2 compares the baseline characteristics of the ED versus the NED group, which resembled each other in age, GOLD stages with most of the subjects suffering from moderate to severe obstruction, as well as BODE and Charlson index. Hypertension and dyslipidaemia were the most frequent comorbidities in general; no differences were observed in mortality. When performing the 6MWT, differential BMI values became evident. The mean BMI was higher in ED than in NED patients with an inverse relation as to the categorical BMI levels <25, 25–29, and ≥30 (p for trends=0.011; Fig. 1).
Characteristic of early and non early desaturators patients.
| Variables, units | Early | Non early | p-value |
|---|---|---|---|
| (n=32) | (n=74) | ||
| Baseline | |||
| Age, years, median (P25–P75) | 68 (63–76) | 68 (60–75) | 0.620 |
| BMI (kg/m2), mean±SD | 29±5 | 25±6 | 0.002 |
| Haemoglobin g/dl, mean±SD | 14.2±2.0 | 14.4±1.7 | 0.667 |
| Smoking pack-year index, median (P25–P75) | 40 (10–68) | 40 (14–53) | 0.939 |
| Dyspnoea, mMRC scale, median (P25–P75) | 2 (1–3) | 2 (1–3) | 0.997 |
| GOLD 2009 | 0.23 | ||
| Stage I (%) | 6 | 7 | |
| Stage II (%) | 44 | 23 | |
| Stage III (%) | 37 | 51 | |
| Stage IV (%) | 13 | 19 | |
| GOLD 2017 | 0.986 | ||
| Stage A (%) | 22 | 20 | |
| Stage B (%) | 41 | 39 | |
| Stage C (%) | 6 | 7 | |
| Stage D (%) | 31 | 35 | |
| Charlson index, median (P25–P75) | 5 (4–7) | 5 (3–6) | 0.129 |
| BODE index, median (P25–P75) | 4 (2–5) | 4 (2–5) | 0.913 |
| Pulmonary function parameters | |||
| 6-min walk distance (m), mean±SD | 371±105 | 435±117 | 0.011 |
| Time to SpO2 (s) <90%, median (P25–P75) | 40 (35–46) | 110 (90–150) | <0.0001 |
| Initial SpO2 (%), mean±SD | 93±1 | 94±2 | 0.002 |
| Nadir SpO2 (%), mean±SD | 83±5 | 86±3 | 0.001 |
| Initial to nadir SpO2 (%), mean±SD | 11±5 | 8±4 | 0.023 |
| FEV1/FVC (% predicted), mean±SD | 47±12 | 41±11 | 0.007 |
| FEV1litres (% predicted), mean±SD | 1.2±0.577 (48±17) | 1.2±0.654 (45±19) | 0.421 |
| FVC litres (% predicted), mean±SD | 2.5±0.673 (76±19) | 2.8±0.795 (81±19) | 0.196 |
| IC litres (% predicted), mean±SD | 2.2±0.703 (88±22) | 2.3±0.695 (87±23) | 0.913 |
| RV/TLC, mean±SD | 142±35 | 142±32 | 0.979 |
| DLCO (% predicted), mean±SD | 51±18 | 55±21 | 0.346 |
| Comorbidities | |||
| Hypertension (%) | 59% | 49% | 0.310 |
| Dyslipidaemia (%) | 59% | 49% | 0.310 |
| Diabetes mellitus (%) | 28% | 15% | 0.109 |
| Ischaemic heart disease (%) | 9% | 15% | 0.443 |
| Heart failure (%) | 16% | 9% | 0.358 |
| Arrhythmia (%) | 16% | 15% | 0.920 |
Data are given as median (25th, 75th percentile) or mean±SD (mean±standard deviation). Pearson Chi-squared, Mann–Whitney U, or Student t-test were applied. BMI: body mass index; FEV1: forced expiratory volume in 1s; FVC forced vital capacity; FEV1/FVC index; IC: inspiratory capacity; RV: residual volume; TLC: total lung capacity; DLCO: carbon monoxide diffusion capacity. mMRC: modified Medical Research Council scale.
Although we observed a significantly lower mean initial SpO2, this was clinically not relevant. Therefore its influence was adjusted in the multivariate analysis using the quartil of initial SpO2. The probability of ED during exercise increased by 1.79 (ORajusted) in overweight and obese patients (95% CI 1.12–2.86; p=0.015).
Finally, the area under the curves showed the discriminative capacity of the continuous scale for BMI analysis: AUC=70% (95% CI, 60–81%; p=0.001; Fig. 2).
Table 2 also reflects the distribution of clinical, functional parameters and lung function. We did not detect any differences in static functional respiratory parameters except that EDs had a lower FEV1/FVC index than NEDs. ED patients also walked 64m less (mean) in the 6MWT (p=0.011), and they desaturated more deeply (10.7±4.6% versus 8.6±3.5%; p=0.025).
DiscussionEID is the result of a mismatch between ventilation and perfusion during physical effort. Airflow limitation and loss of lung elasticity lead to increased air trapping and dynamic hyperinflation, increasing patient inspiratory work and thereby increasing oxygen consumption in COPD patients.3,13,14 Until a few years ago, this phenomenon observed during the 6MWT, did not provide any further information than that of the change in SatO2. It was considered a mere curiosity, which appeared in a group of COPD patients but did not translate into a change in medical attitude, perception of poor prognosis or treatment modification. Takigawa et al.15 demonstrated that, in addition to the distance walked in the 6MWT, the variation in SatO2 also had prognostic implications. Later, the phenomenon came to be no longer regarded as an unimportant fact, but one to be taken into account together with parameters such as the metres covered in the 6MWT, the FEV1, and the oxygen partial pressure in blood. A few years later, these findings were corroborated by the ECLIPSE8 group, who demonstrated that both desaturation and the frequency of stops during the walk test were prognostic factors. However, the possible different types of desaturation have not yet been well characterised, neither in terms of their definition, which remains ambiguous, nor addressing the different forms as to the distinction between basal and minimal desaturation, its quality and nature. We defined a category, termed ED, to differentiate it from late and intermediate desaturation. This was the result of a study where we compared desaturation in two different settings, the 6MWT and daily life activities. Only the patients who desaturated within the first minute of the test also did so outside the hospital in their daily activities, something that was not true of those who desaturated only after 3.5min.9 Therefore, early desaturation in the 6MWT is a relevant aspect, because it implies desaturation during everyday activities and under low levels of physical strain. In addition to this aspect, the ED patient group is more likely to develop respiratory insufficiency over time than the NEDs. Hence, the elapsed time to desaturation in the 6MWT is a useful variable, which provides information of clinical interest. Additional potential markers to consider are the depth and persistence of desaturation. Of note, early desaturation also tends to be deep; according to our observations in this study, the nadir is very low. We were interested in defining a profile of patients who desaturate early and analyse clinical and functional characteristics to identify potential differential parameters between EDs and patients who desaturate after the first minute of the 6MWT. Like other authors,2,6 we found that desaturation is typical of patients with low FEV1 and relatively low baseline DLCO and SatO2 values. But it remained to be determined whether there was a defined profile for ED patients. We did not observe differences in either age or FEV1 values, and although DLCO was somewhat lower in EDs, this was not statistically significant. From a functional point of view, basal SatO2 and the distance walked in the 6MWT were significantly lower in EDs compared to the NED group, and it should be emphasised that the desaturation in the ED group was more profound, which may be considered as another feature of severity. However, BMI was the most outstanding parameter in the ED group. These patients were more obese, although this was not associated with comorbidities such as ischaemic heart disease, cardiac arrhythmia, or AHT. Recently, Andrianopoulos et al.8 analysed patients from the ECLIPSE cohort and described obesity as a factor involved in EID (OR 1.57, 95% CI 1.15–2.14) along with additional parameters, such as a high degree of airflow obstruction and low DLCO values. While obesity has been linked to low baseline SatO2 and EID,8,16 our study adds that this feature appears to be limited to ED COPD patients.
COPD patients may exhibit very diverse characteristics, which depend on the association with other conditions such as bronchial asthma, sleep apnoea, and fibrosis. EID occurs preferentially in severe patients with low DLCO values; although, unexpectedly, it is not observed in lean but in obese patients. Early desaturation, which we think is of great importance because it translates to increased severity, is preferentially observed in subjects with a BMI ≥30. Alterations in respiratory mechanics or higher levels of proinflammatory cytokines such as leptin may possibly explain this phenomenon.17
There are some limitations; the study is retrospective, the number of patients is not very high, the proportion of women is very low, we did not select non-smoker patients and the study only took place in hospital.
In summary, we would like to draw special attention to COPD patients with severe to very severe obstruction, low DLCO, and overt obesity, because they may experience early and profound desaturation during exercise and, together with the obesity, suffer from very harmful long-term effects.
FundingMenarini SA Corp Foundation.
Conflicts of interestThe authors have no conflicts of interest to declare.