The World Health Organization has classified the COVID-19 situation as a pandemic. Patients infected with COVID-19 typically present with fever, cough, dyspnea, and myalgia, and the infection may cause severe pneumonia. Laboratory findings are unspecific. Although test results are normal for many patients, the predominant laboratory abnormalities include the elevation of inflammatory markers, such as C-reactive protein, lactate dehydrogenase, and the erythrocyte sedimentation rate. Additionally, lymphopenia is consistently present in more than 40% of patients.1–3 Currently, real-time reverse-transcription polymerase chain reaction is the reference standard test for the definitive diagnosis of COVID-19 infection.
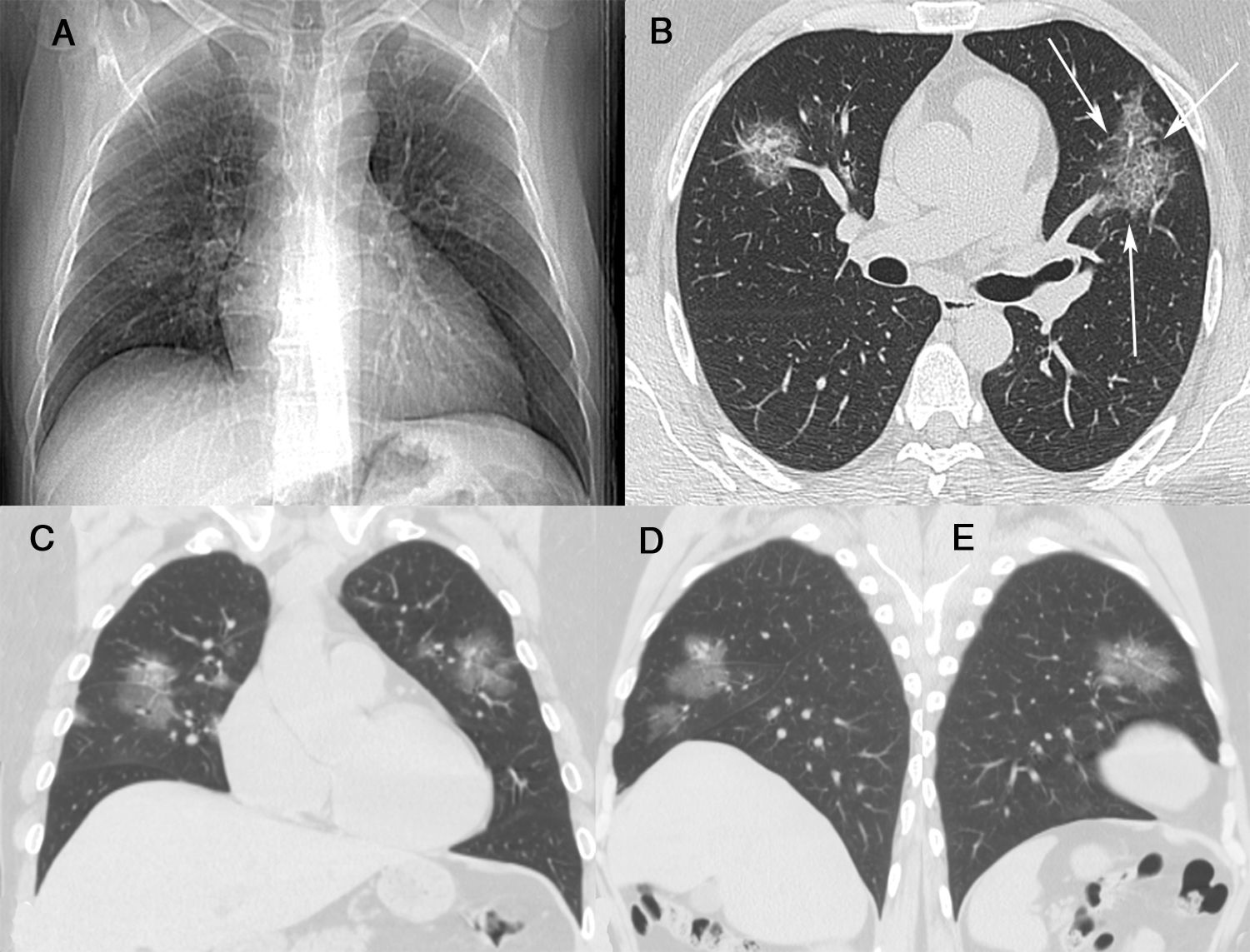
A 44-year-old man presented to the hospital (Centro Hospitalar do Porto, Porto, Portugal) on 7 March 2020 with a 6-day history of fever, cough, rhinorrhea, diffuse myalgia and fatigue. He had had close contact with a friend who had traveled to Milan, Italy, on 22–23 February 2020, during the COVID-19 pneumonia outbreak. On admission, the patient was in good general condition; he was tachypneic (respiratory rate of 30 breaths/min), his body temperature was 38.2°C, and cardiac auscultation was normal, with no murmur or arrhythmia. Pulmonary auscultation demonstrated the presence of sparse bilateral crackles. Laboratory tests showed a normal blood cell count, erythrocyte sedimentation rate of 84mm/h (normal=0–10mm/h), C-reactive protein level of14mg/L (normal=0.3–10mg/L), and unremarkable lactate dehydrogenase, creatine phosphokinase, and liver function findings. Blood gas analysis yielded normal findings (O2 saturation=98%). The patient's respiratory rate returned to normal after the normalization of his temperature. Non-enhanced chest computed tomography (CT) showed multiple round and oval ground-glass opacities in both lungs, with a crazy-paving pattern (Fig. 1B–D). No mediastinal lymphadenopathy or pleural effusion was present. Real-time reverse-transcription polymerase chain reaction of a nasopharyngeal sample revealed positivity for 2019-nCov nucleic acid. Hydroxychloroquine and symptomatic medication were administered. The patient recovered uneventfully and was discharged after 16 days in an asymptomatic state.
(A) A posteroanterior chest radiograph was considered normal. Unenhanced chest computed tomography with axial (B), coronal (C) and sagittal (D and E) maximum-intensity projection imaging demonstrated areas of ground glass opacity, many with round and oval morphologies, in both lungs. Not also in B inter- and intralobular septal thickening with a crazy-paving pattern (arrows).
Although our patient had pneumonia, as confirmed by CT, the chest radiograph was normal. Chest radiography has not been recommended as a first-line imaging modality for the diagnosis of COVID-19 due to its limited sensitivity in the detection of ground-glass opacities and other incipient pulmonary findings of the infection, which are evident on CT. However, nonspecific chest radiography findings have been reported occasionally, particularly for patients with severe disease.4,5 The role of CT in COVID-19 evaluation is the subject of much discussion. Some authors suggest that CT has a pivotal role, whereas other investigators are less optimistic. The predominant CT findings are multifocal, bilateral, peripheral, and basal-predominant ground-glass opacities, often with round and/or oval morphology and/or consolidation. The crazy-paving pattern may be observed. This pattern is defined as thickened interlobular septa and intralobular lines superimposed on a background of ground-glass opacities. Pleural effusion, small lung nodules, cavitation, and lymphadenopathy are very uncommon findings.2,5,6 These CT findings are not specific to COVID-19; similar results can be obtained for other infectious and non-infectious diseases.6
However, two characteristics of the ground-glass opacities may suggest the diagnosis of COVID-19 in the context of the current pandemic. The presence of multifocal nodular (round or oval) ground-glass opacities7,8 and/or the association of these opacities with reticulation (the crazy-paving pattern)8–10 should alert the radiologist to the possibility of COVID-19 infection. The latter finding appears particularly when the disease progresses. Our patient presented both findings. We believe that these two findings are important for the diagnosis of COVID-19, although the crazy-paving pattern is less specific; Amorim et al.11 observed it in 15% of 70 patients with confirmed H1N1 infection.
Conflicts of interestThe authors have no conflicts of interest to declare.