Foreign body (FB) aspiration is uncommon in adults, with an estimated incidence around 0.2%.1 FB can either be organic (e.g., peanuts, peas, etc.) or inorganic (e.g., pins, screws, nails, etc.). Identification of FB aspiration requires clinical suspicion, especially in those presenting with no history of aspiration. Occasionally, a forgotten FB may be detected during bronchoscopy or on a chest radiograph obtained for unrelated reasons. During bronchoscopy, a FB can be directly visualized. Granulation tissue, endobronchial stenosis, or edema—all features of tissue reaction to an aspirated FB—may also be present. In children, rigid bronchoscopy is the procedure of choice for FB removal due to its ability to secure the airway, whereas flexible bronchoscopy can be employed to confirm adult diagnoses and remove the FB. Furthermore, in children, FBs lodge in the proximal tracheobronchial tree, which can be easily accessed using a rigid bronchoscope. In adults, foreign bodies lodge in the distal tracheobronchial tree.2
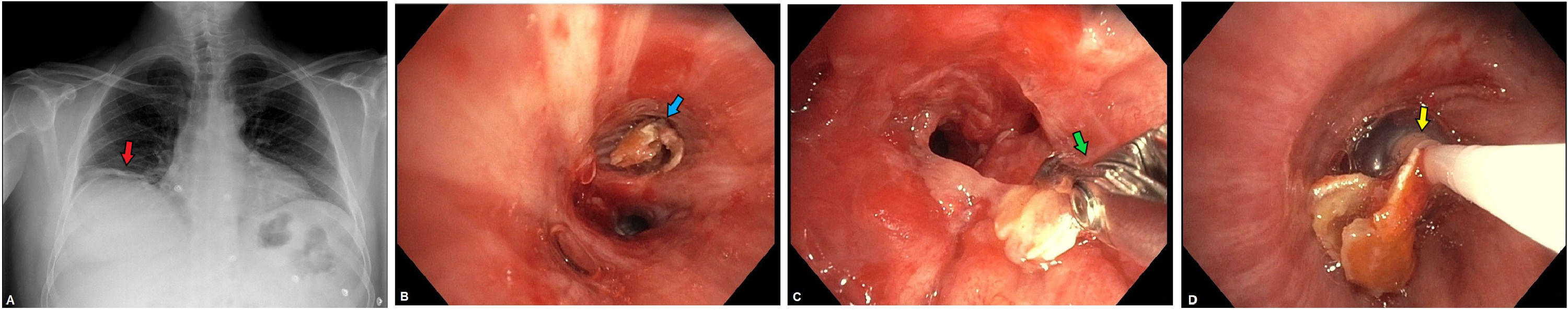
A 57-year-old male with no medical history was referred for evaluation of cough and dyspnea grade II / IV mMRC for 3 months’ duration after choking while eating, without improvement of vilanterol and inhaled fluticasone furoate. Physical examination revealed normal expiratory wheezing in the right hemithorax in complementary tests, except elevation of the right hemidiaphragm with subsegmental atelectasis in the right lower lobe (Fig. 1A).
A Subsegmental atelectasis in the right lower lobe (red arrow). B. Crustacean remains (blue arrow) at the bronchial entrance B8-B10 and adjacent mucosal erythema. C-D. Extraction of crustacean remains using EndoJawFB-231D Olympus® forceps (green arrow) and Fogarty® catheter (yellow arrow).
Flexible bronchoscopy was performed, revealing a circumferentially hard consistency, dotted irregular surface, and brown coloration FB was proximal to the entrance to bronchi B8-B10 and adjacent erythematous mucosa, with abundant whitish secretions. Complete removal was performed using EndoJawFB-231D Olympus® forceps, flexible ERBE® cryotherapy probe (2.4 mm diameter) and Fogarty® catheter (Image 1B-D). The pathological anatomy was compatible with crustacean remains. Oral treatment with methylprednisolone was prescribed, along with subsequent endoscopic and radiological revision without alterations. The patient reported cessation of symptoms after intervention.
In the face of chronic cough, a correct anamnesis and physical examination informed by the possible etiology should be carried out.3 FB aspiration has variable symptoms: cough, dyspnea, expectoration, wheezing or asphyxia. Symptoms may also be absent. When FB is suspected, chest radiography should be the initial test, after which a bronchoscopy should be performed for extraction.1