Understanding basic principles of pathophysiology, modes, patient-ventilator interaction and waveform analysis is essential for the safe delivery of mechanical ventilation.1–3 The COVID-19 pandemic has profoundly impaired medical education, reducing the chance of in-person educational events and leading to an increasing number of physicians with little or no specific experience (i.e. trainees or physicians from other fields) being hired and managing mechanically ventilated critically ill patients. Thus, effective methods to teach competencies in mechanical ventilation to large cohorts of physicians in short periods of time were urgently needed. Simulators for training had been previously investigated4–6 for teaching purposes, but free or open source simulators are rare, and they often have outdated technical requirements, limiting their use in current educational programs.
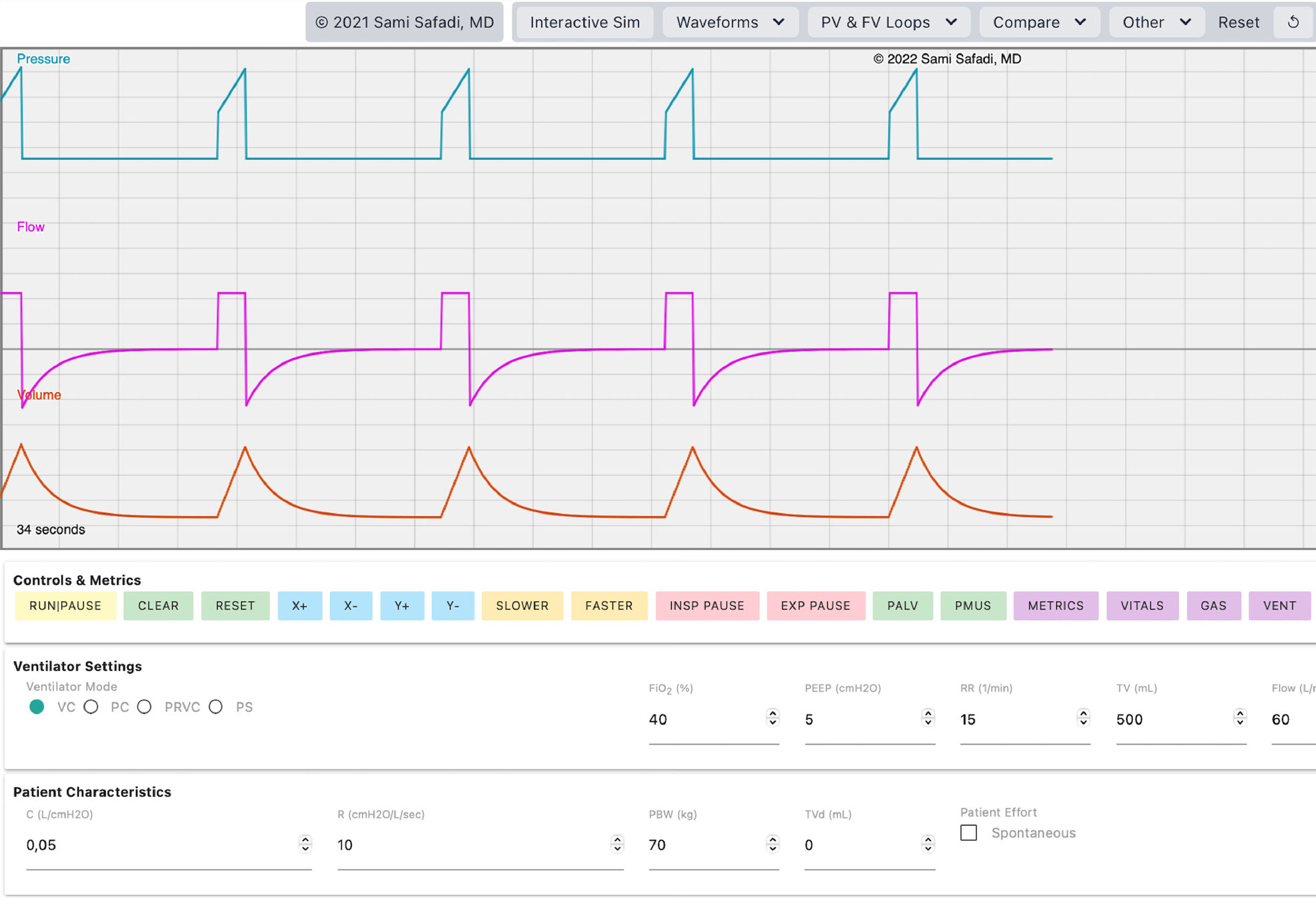
To address such issues, we conducted a randomized controlled trial assessing the effectiveness of a remote simulation-based training using VentSim©,7 free, interactive, online software with a graphic interface displaying standard ventilator curves, able to simulate basic modes of mechanical ventilation and patient-ventilator interaction (Fig. 1). The protocol of this trial was approved by the Ethics Committee Palermo 1 (ID: 11/2021, date: 15 December 2021) and followed the Helsinki Declaration. We assessed the effectiveness of providing a short educational cycle with standard teaching alongside simulation-based lessons, in comparison to standard teaching alone, to increase the knowledge and skills on mechanical ventilation of trainees in anesthesia and intensive care.
For the purpose of this study, all the trainees regularly attending the specialty training program in a single centre in Italy were officially invited to participate to the study. A total of 183 residents voluntarily joined the study and were randomized, using strata based on previous rotation in the Intensive Care Unit (ICU). The rate of lost to follow up was 19%. All the analyses were performed under the intention-to-treat principle. All the participants attended two two-hour remote lessons provided by two academics, consultants in Anesthesia and Critical Care (CG and AC) on core topics of mechanical ventilation. Participants randomized to the intervention group (“VentSim© group”) also attended two remote simulation-based lessons, delivered using the simulation software VentSim©.7 All the lessons were held in the period from 24th February and 29th March 2022. We collected baseline characteristics of the participants including age, gender and information about previous rotations in ICU.
The primary outcome of the trial was the number of correct answers to a 50 multiple choice questionnaire, composed of 21 theorical questions, 24 waveform interpretation questions, and 5 clinical scenarios. Trainees’ satisfaction on the educational program was also assessed as secondary outcome, through 5 sentences on which the participants had to express agreement with a 5-points Likert scale.
The overall number of correct answers was similar between the VentSim© group and control group (28.6 ± 8.6 vs. 27.6 ± 9; P = 0.49). Using a 5-points-Likert scale, the VentSim© group rated 4 [4–5] the contents, 4 [4–5] the clarity of explanation, 4 [4–5] the self-perceived comprehension of mechanical ventilation and 4 [3–4] the self-perceived ability to manage mechanically ventilated patients. No significant effect of the intervention was registered in term of satisfaction through these items. The VentSim© group rated 5 [4–5] the utility of integrating simulation in routine training of residents.
Our data showed that a remote simulation-based course on mechanical ventilation with VentSim© did not significantly improve the competencies of trainees in anaesthesia and intensive care in comparison with traditional lessons at the end of a short educational cycle (Table 1). These data could be interpreted in favor of the potential need to resume face-to-face teaching educational programs of adequate duration during the chronic phase of pandemic. Among limitations, the single-center design and the potential bias due to assignment to intervention (e.g., residents in the control groups may have studied more to offset their assignation group) may have limited the results. Also, the external validity is limited, as the results may be different in other centers. Finally, we did not grant learners free access to the platform after the workshops, which could be an advantage of using software instead of macrosimulation, also in term of information retention. However, the high rate of satisfaction among the participants, the absence of associated costs and the readiness to be used in remote meetings, make VentSim© a potentially valuable complementary didactical tool.
Characteristics of included participants and outcome measures.
Data are reported as mean ± SD or median [IQR] and percentages, as appropriate.
The number of correct answers (primary outcome) and overall agreement on satisfaction statements (additional outcome) were compared using t- test for independent means, if normal distribution confirmed through Shapiro-Wilk test. Mann Whitney U test was used in case of non-normal distribution of the data. Unbalances between of the two groups on participants’ characteristics were also checked for, using Mann Whitney U test and Chi-square, as appropriate. Statistical significance was accepted at p-value < 0.05 and all tests were 2-tailed. A secondary analysis was conducted on the type of questions, considering only the questions related to waveforms interpretation. A subgroup analysis basing on previous clinical rotation in ICU was also conducted.
Overall, our data seem to suggest that remote training may not be the best option for educational programs on mechanical ventilation, although these pandemic years made such solutions inevitable. Moreover, the results suggest that it is unlikely that a single short educational cycle can lead to full understanding of the mechanical ventilation techniques or the ability to solve clinical scenarios, independently of the methods. These considerations should be taken into account when setting educational programs for young physicians. Further studies should assess the efficacy of face-to-face simulation-based educational program on mechanical ventilation using VentSim©, also evaluating the best group size of trainees to optimize such learning experiences.
Data availability statementData are available upon reasonable request to the corresponding author.
FundingNone.
CRediT authorship contribution statementM. Ippolito: Conceptualization, Visualization, Formal analysis, Data curation, Writing – original draft. B. Simone: Data curation, Resources, Writing – review & editing. S. Safadi: Writing – original draft, Software, Data curation, Writing – review & editing. E. Spinuzza: Data curation, Writing – review & editing. T. Catania: Data curation. G. Ingoglia: Data curation, Writing – review & editing. M. Milazzo: Data curation, Writing – review & editing. S.M. Raineri: Data curation. A. Giarratano: Data curation, Writing – review & editing. C. Gregoretti: Writing – original draft, Writing – review & editing. A. Cortegiani: Conceptualization, Visualization, Writing – original draft.
We would like to thank you Dr. Sergio Palazzolo and Dr. Francesco Muffoletto for the support provided for the use of remote meeting platforms.