Mechanical ventilation in the prone position is a validated strategy of invasive ventilator support in the treatment of acute respiratory distress syndrome (ARDS).1 Given its beneficial effects, there has been some research into the use of prone positioning also in non-intubated patients with ARDS2,3 and in patients with COVID-19 to avoid intubation,4,5 but few studies2,3,6,7 have assessed its efficacy and possible effects during SARS Cov-2 pandemic.8–13 The use of standard oxygen and High Flow Nasal Cannula (HFNC) in refractory hypoxemia due to SARS CoV-2 is controversial and many International Guidelines, while suggesting a brief trial, raise concerns about the potential risk of unduly delayed intubation. We describe the physiological changes and clinical outcome of three patients suffering from severe Acute Respiratory Failure (ARF) due to COVID-19 undergoing trials using semi-recumbent, prone and lateral position during standard oxygen and HFNC. All patients tested positive on reverse transcription-polymerase chain reaction (RT-PCR) on throat swabs; comorbidities and administered drugs are reported in Table 1.
Demographic, clinical characteristics, laboratory and CT-scan findings at respiratory intensive care unit admission, drugs, ABGs.
| Patient 1 | Patient 2 | Patient 3 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Demographics | |||||||||||
| Age-yr | 74 | 71 | 70 | ||||||||
| Sex | Female | Male | Female | ||||||||
| Initial findings | |||||||||||
| Medical history | Dyslipidemia, hypothyroidism, carotid atheroma | Hypertension, deep venous thrombosis | Hypercholesterolemia and hypertension | ||||||||
| Symptoms at disease onset | Fever | Fever, cough | Fever, asthenia, dyspnoea | ||||||||
| Pharmacological treatment | |||||||||||
| (dosages are shown for drugs initiated during RICU stay) | Hydroxychloroquine, piperacillin-tazobactam, azithromycin, enoxaparin, tocilizumab 162 mg x2 s.c., methylprednisolone 1,6 mg/kg | Hydroxychloroquine, enoxaparin, ceftriaxone, tocilizumab 162 mg x2 s.c., methylprednisolone 1 mg/kg | Hydroxychloroquine, azithromycin, enoxaparin, ceftriaxone, tocilizumab, methylprednisolone | ||||||||
| Imaging features | |||||||||||
| Thoracic HRCT scan | GGO, bilateral pulmonary infiltrates, mainly in the posterior dependent zones | GGO and consolidations prevalent on the left lug | GGO and pulmonary infiltrates prevalent on the right lung | ||||||||
| Days from Hospital admission to prone/lateral decubitus | |||||||||||
| 6 | 11 | 8 | |||||||||
| ABGs | Patient 1 | Patient 2 | Patient 3 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| PRE | During NIV | PP/LD after 12h | PRE | During HFNC | DuringPP/LD | PRE | During HFNC | During PP/LD | |||
| pH | 7,49 | 7,48 | 7,47 | 7,42 | 7,45 | 7,43 | 7.48 | 7,49 | 7,45 | ||
| PaCO2 (mmHg) | 32 | 31 | 35 | 42 | 39 | 40 | 33 | 30 | 35 | ||
| PaO2 (mmHg) | 66 | 62 | 162 | 80 | 76 | 80 | 62 | 70 | 109 | ||
| PaO2/FiO2 | 83 | 80 | 203 | 160 | 158 | 211 | 115 | 116 | 205 | ||
| HCO3- (mmol/L) | 26 | 26 | 27 | 27 | 27 | 26 | 26 | 26 | 25 | ||
| Vital Parameters | |||||||||||
| PRE | PP/LD after 2h | After 12h | PRE | PP/LD after 2h | After 12h | PRE | PP/LD after 2h | After 12h | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| RR (breaths per minute) | 25 | 20 | 26 | 22 | 16 | 18 | 21 | 22 | 20 | ||
| Heart rate (bpm) | 87 | 72 | 80 | 74 | 60 | 65 | 68 | 64 | 65 | ||
| Mean Arterial Pressure (mmHg) | 97 | 113 | 107 | 108 | 97 | 103 | 88 | 87 | 96 | ||
RICU, Respiratory Intensive Care Unit; GGO, ground-glass opacities; s.c., sub cutaneous; NIV, non invasive mechanical ventilation; HFNC, High Flow Nasal Cannula; PP, prone position; LD, lateral decubitus.
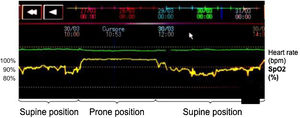
A 74 year-old woman was admitted on March 19th, after 10 days of fever. On the 24th she was transferred to our Respiratory Intensive Care Unit (RICU) due to worsening of her respiratory conditions. On arrival, she was haemodynamically stable, her respiratory rate was 18/min in a reservoir oxygen mask at 15 l/min; ABG testing showed a severe impairment of gas exchange (PaO2/FiO2 87; PaO2 69 mmHg, PaCO2 33 mmHg, pH 7.49, HCO3- 27,8 mmol/L). We initiated non-invasive ventilation (NIV) with helmet interface (PSV: PS 22 cmH2O, PEEP 10 cmH2O, FiO2 80%), without improvement of gas exchange (PaO2/FiO2 80). A high resolution CT-scan (HRCT) showed bilateral consolidations with ground-glass opacities (GGO), mainly in the posterior dependent zones. Based on this radiological picture we pronated the patient whilst administering oxygen-therapy with reservoir mask. An almost immediate increase of SpO2 was observed (Fig. 1). At 2 h the PaO2/FiO2 had increased to 203 mmHg and this trend was maintained after 12 h of prone positioning (Table 1). She improved slowly with a schedule of pronation of two sessions lasting 6 h throughout the day and overnight and was discharged home on April 29th.
The second case was a 71-year-old man, admitted to the Emergency Department (ED) with fever and progressively worsening dry cough for one week. On admission, ABG showed ARF (PaO2/FiO2 261, PaO2 55 mmHg, PaCO2 31 mmHg, pH 7.45, HCO3-24 mmol/l). Clinical conditions and gas exchange rapidly worsened (ABG 48 h after admission: PaO2/FiO2 186, PaO2 65 mmHg, PaCO2 33 mmHg, pH 7.43, HCO3- 25,6 mmol/L) and on day 6 since admission he was referred to our RICU, where HFNC therapy was set (Flow 50 L/min, FiO2 50%). The HRCT scan showed parenchymal involvement of the left lung, with relative sparing of the right one. A spontaneous breathing trial was performed placing the patient on the right lateral decubitus during HFNC therapy. Respiratory rate rapidly decreased (from 22 to 16 breaths/min) and ABG showed a significant improvement of oxygenation (P/F ratio of 202 and 211 after 2 and 12 h respectively) (Table 1). Therefore, we scheduled at least two sessions lasting 6 h of lateral position throughout the day and overnight. He was transferred to the ward 8 days after ICU admission and discharged at home after 28 days.
The last patient was admitted to the ED after 6 days of fever, asthenia and dyspnoea. On admission, ABG was normal, but lung ultrasound documented signs suggestive of interstitial-alveolar pneumonia and a HRCT confirmed bilateral GGO associated with initial peripheral consolidations. The patient’s condition deteriorated and she was transferred to our RICU, where HFNC therapy was started (Flow 45 L/min, FiO2 60%). A novel CT scan showed a relative sparing of the left lung, therefore she was placed in left lateral decubitus. Changes in oxygenation as well as in respiratory pattern are summarized in Table 1. Two sessions lasting 6 h of lateral position throughout the day and overnight determined a stable improvement of gas exchange and prevented mechanical ventilation. She was discharged home after 21 days from hospital admission.
Our findings indicate that this strategy is feasible and a useful option in the management of acute respiratory failure due to this disease. In fact, patient recumbency in accordance with imaging to adjust V/Q was associated with a significant improvement of oxygenation and breathing pattern, with good tolerance. In addition, we found no significant hemodynamic adverse effects. The physiologic rationale for prone positioning and lateral decubitus in non-intubated patients is strong: firstly, redistribution of V/Q ratio due to the gravity-induced increase of blood flow to spared regions of the lung, which becom better ventilated14; secondly, lung recruitment of previously dependent regions occurs as “oedema” flows away from anti gravitational alveoli.14 Similarly, positioning patients with unilateral pleuro-parenchimal disease with the normal lung down, especially in the absence of pleural pain, can affect gas exchange.15,16 Thirdly, the increase in oxygenation should also ameliorate hypoxemic vasoconstriction, reducing pulmonary vascular resistance and improving right ventricular function.17 In addition, in the prone position we may obtain a relief from the weight of the mediastinum and a decrease in overdistension of the healthy areas, thanks to the distribution of trans-pulmonary pressure. In fact, recruitment of the dorsal lung, which has a higher degree of perfusion in either position, reduces shunt.18,19 A retrospective study including 15 patients showed a beneficial effect of prone position during NIV in patients with severe ARF due to pneumonia.2 Recently, Ding3 reported a reduction in intubation rate in patients with moderate to severe ARDS when treated with combined prone positioning and NIV or HFNC.
Recent studies8–13 showed that prone positioning may improve gas exchange in COVID-19 patients during oxygen therapy and non invasive support ( HFNC or NIV). However, no information about the radiological pattern has been provided. In contrast, our cases showed that the distribution of parenchymal lesions could be a valid criterion to select patient for spontaneously breathing trial in prone positioning and lateral decubitus. Chest x-ray could be useful to support diagnosis, especially during Sars-cov 2 pandemic: sensitivity values range from 57% to 89%.20 However, Chest-x-ray can not detect spared lung areas: exclusive dorsal lung areas involvement can not be detected without latero-lateral projection, not usually performed in critical setting, requiring orthostatic posture. As observed by Marini,4 COVID-19 pneumonia appears to include an important vascular insult that potentially mandates a different approach from that usually applied for ARDS. Our patients, despite very poor oxygenation and extensive parenchymal lesions, recovered without needing either NIV or intubation, and such a result would not, probably, have been possible in a “traditional” ARDS. All healthcare workers exposed used personal protective equipment (PPE).21 Interestingly, in all 3 cases reported we observed that PaCO2 did not change, indicating that the change in PaO2 was not a consequence of a change in alveolar ventilation, supporting the theory of a beneficial effect on V/Q ratio. However, we do not recommend delaying intubation or attempting this approach in a setting without intensive monitoring, which is necessary to quickly upgrade ventilatory support in non-responders.
To conclude, we have demonstrated that preferential decubitus on the least affected areas of the lung, either in prone or lateral position, in awake and spontaneously breathing, non-intubated patients with ARF due to COVID-19 pneumonia is feasible, well tolerated and is associated with a significant benefit on oxygenation. Further studies are warranted to confirm our results.
Declaration of interestsThe authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.