Endobronchial hamartoma (EH) represents nearly 10% of all lung hamartomas, the most common benign lung tumour.1 Although benign, hamartoma has been linked with lung cancer and very occasionally can evolve to a malignant lesion.1,2 They are rare, slow growing, usually single tumours, often symptomatic, unlike intraparenchymal hamartomas.2,3 Obstructive pneumonia and hemoptysis are the most frequent symptoms. However, wheezing, dyspnea and cough might be the only signs present, mimicking other conditions like asthma.2,4 Clinical suspicion should be raised when symptoms persist, and patients offered a chest computed tomography and bronchoscopy. As EH is often symptomatic, treatment is frequently indicated.3
The authors intend to retrospectively analyse all cases of EH diagnosed from 2011 until mid-2021, in a tertiary hospital in Porto, Portugal. This study was approved by the hospital ethics committee (number 226/2021) on 21st September 2021. The ethics committee considered the exemption from Informed Consent to be acceptable.
During the study period, EH was diagnosed in 14 patients. Eleven patients (78.6%) were male, with a median age of 61.50 years (IQR 57.75–72.0), 71.4% were current or former smokers.
Eight patients presented respiratory symptoms that prompted endoscopic evaluation: recurrent respiratory infections (n = 4), nonresolving pneumonia (n = 2) and hemoptysis (n = 2). In the remaining six patients, EH diagnosis was incidental.
It was an incidental radiological finding in two patients who underwent thoracic/abdominal computed tomography for other reasons (chest trauma and acute cholecystitis) that revealed an endobronchial lesion. The additional four cases were incidental endoscopic findings: two patients with concurrent lung cancer (EH and neoplasm were in different lobes), one patient who underwent bronchoscopy to exclude lung metastases (rectal adenocarcinoma), and one patient with suspected airway compression by Kommerell's diverticulum.
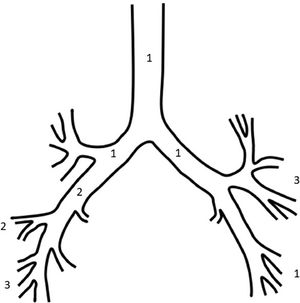
Concerning EH location in the tracheobronchial tree, it was more frequently found in the right bronchial tree (n = 8) – Fig. 1. The lesion was often described as having smooth and regular surface, without signs of deep invasion, and sometimes with polypoid features – Fig. 2A–C.
An example of an endobronchial hamartoma totally occluding the intermediate bronchus (Fig. 2. A, B); and later, after treatment by rigid bronchoscopy - mechanical debridement and laser (Fig. 2. C). Endobronchial hamartoma biopsy showing endobronchial epithelium, adipose tissue and hyaline cartilage [H&E; x10] (Fig. 1.D).
Histological aspects provided more accurate classification of hamartomas, describing six cases of chondroid hamartoma and only one case of lipoid hamartoma, in seven cases no predominant cellular component was described (Fig. 2D).
Excluding two patients with concurrent lung cancer, eight of the 12 patients (66.7%) presented significant bronchial obstruction: main bronchus obstruction (n = 1), lobar bronchus obstruction (n = 5) and segmental bronchus obstruction (n = 2).
Ten patients needed endoscopic treatment to restore acceptable bronchial patency. Mechanical debridement plus laser photoresection were used in six cases, and only mechanical debridement was necessary in the remaining four cases. In two patients, mechanical debridement was performed through flexible bronchoscopy due to segmental lesions. All other eight patients underwent rigid bronchoscopy. Total EH resection was accomplished in half of the patients (n = 5).
One rigid bronchoscopy, performed due to total middle lobar bronchus obstruction, was complicated by pneumomediastinum and pneumothorax with no need for drainage. In this case, bronchial perforation could not be excluded, though it was not recognized during bronchoscopy. No other complications were registered.
One patient needed a second endoscopic procedure. Another patient with partial resection after mechanical debridement and laser, who maintained recurrent respiratory infections, underwent lobectomy with clinical resolution and no complications.
For the 13 patients not needing surgery, follow-up until now or until death (median time of 3.50 years (IQR 0.88-5.50)) showed no EH recurrence and no need for further endoscopic treatment.
EH management must be individualised depending on features and location of the hamartoma, symptoms, fitness and preference of the patient.3,4
Bronchoscopy plays an essential part in EH diagnosis, providing its precise location in the airway and biopsy.4
Still, bronchoscopy role in EH treatment is not less relevant, having replaced surgery as the first choice for management of EH given diagnosis confirmation and healthy lung parenchyma.5
EH resection is usually performed by rigid bronchoscopy, since it assures airway patency and ventilation, the use of different tools and techniques and easier control of bleeding or other complications, if necessary. Laser, electrocautery, argon plasma coagulation and cryoablation, combined with mechanical debridement, have been used in EH resection with effective results.2
In particular cases, flexible bronchoscopy may be preferred, as in more distal lesions, if the patient is not suitable for rigid bronchoscopy or it is not available.2 However, the rate of recurrence associated with flexible bronchoscopy resection is superior to rigid bronchoscopy.5
Compared to surgery, endoscopic resection is a less invasive procedure, presents better mortality and allows sparing of healthy lung. The most frequent complication of bronchoscopy treatment is pneumothorax, still overall morbidity is low.5
EH presents a low recurrence rate, superior after endoscopic treatment compared to surgical treatment. Long term endoscopic surveillance guided by clinical and radiological features is advised.5
Altogether, the benefits of endoscopic resection seem to outweigh those of surgical treatment. Surgery is usually reserved for cases with long-standing bronchial obstruction with irreversible parenchymal damage, non-resolving symptoms or when malignancy cannot be excluded.2
In conclusion, endoscopic resection is the first choice in EH treatment since excellent results can be achieved in centres of expertise.
Recurrence and malignancy development, though infrequent, may occur and so, follow-up should be ensured.2





![An example of an endobronchial hamartoma totally occluding the intermediate bronchus (Fig. 2. A, B); and later, after treatment by rigid bronchoscopy - mechanical debridement and laser (Fig. 2. C). Endobronchial hamartoma biopsy showing endobronchial epithelium, adipose tissue and hyaline cartilage [H&E; x10] (Fig. 1.D). An example of an endobronchial hamartoma totally occluding the intermediate bronchus (Fig. 2. A, B); and later, after treatment by rigid bronchoscopy - mechanical debridement and laser (Fig. 2. C). Endobronchial hamartoma biopsy showing endobronchial epithelium, adipose tissue and hyaline cartilage [H&E; x10] (Fig. 1.D).](https://static.elsevier.es/multimedia/25310437/0000002900000001/v1_202301030817/S2531043722001490/v1_202301030817/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9znTMwFdb/TnkS0koegILxs=)




