Pulmonary metastases are complications of multiple malignancies due to haematogenic or lymphatic spread. Most patients who develop pulmonary metastases cannot be cured; however, despite the absence of randomized controlled trials on the subject, in selected cases metastasectomy can be a therapeutic option. Apart from surgery, other treatment options include pharmacologic treatment according to the primary malignancy or various ablative techniques, such as stereotactic radiosurgery and image-guided thermal ablation.1 Data on feasibility and potential complications of ablative techniques is lacking, despite their potential severity, as presented in this case.
The authors present a case of a 64 year-old female patient, with metastatic parathyroid carcinoma, who underwent thermal ablation of pulmonary metastasis due to hypercalcemia refractory to medical treatment with denosumab. She had previously been submitted to two lung metastasis thermal ablations, leading to improved calcium levels’ control, while the oncological disease remained stable. She had no other relevant past medical history.
Eight days after this new procedure, the patient was admitted to the emergency room (ER) due to retrosternal pain and dyspnoea of one day of duration. She also complained of swallowing problems in the cervical region.
At the ER presentation, vital signs were normal: blood pressure 120/80 mmHg, respiratory rate of 18 breaths/min, heart rate of 90 beats/min, and an oxygen saturation of 93% on room air. On pulmonary auscultation, there were crackles on the right hemithorax and lung sounds were lowered on the all hemithorax, and inaudible on the right lower third. Inspection revealed a swollen neck with subcutaneous emphysema on the cervical, right chest and arm areas.
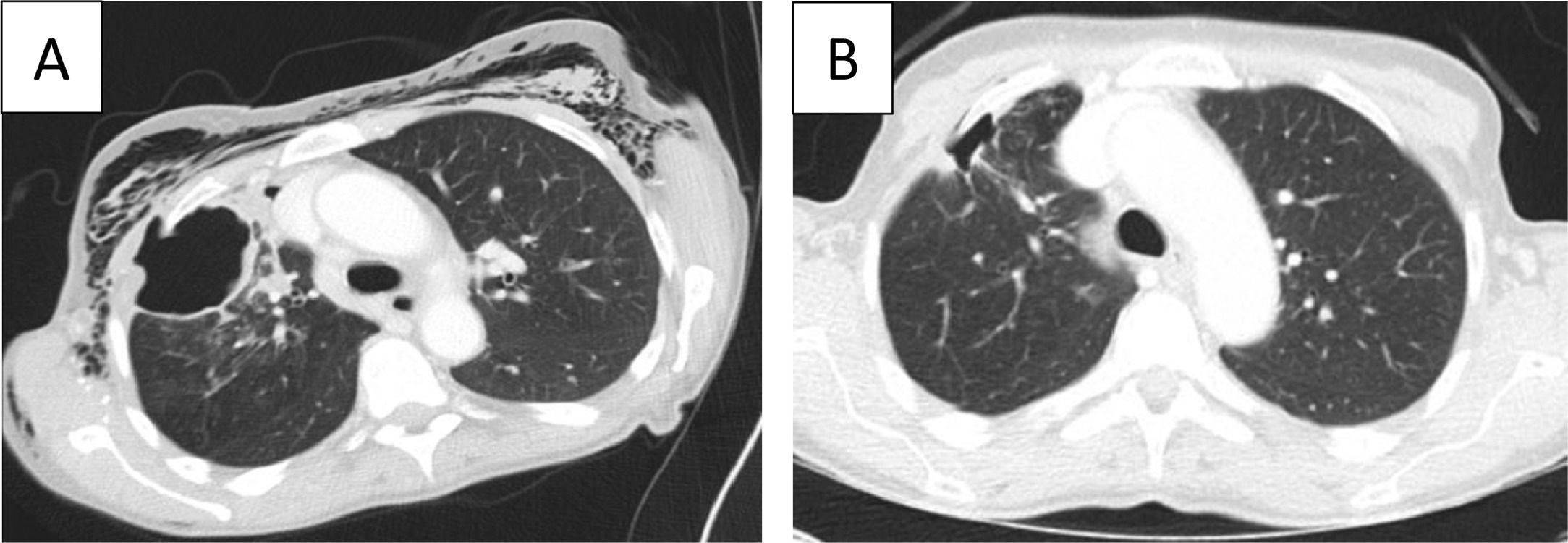
Laboratory analysis at the ER: Arterial blood gas analysis (FiO2 50%): pH of 7.35, PaCO2 of 29,1 mm Hg, PaO2 of 72 mm Hg, and bicarbonate of 15,9 mEq/L. Ionized serum calcium levels were 1,37 mmol/L. Hemogram, urea, creatinine, and thyroid function test results were within normal limits. Chest CT revealed two pulmonary cavities on the right upper and middle lobes, a fistulous trajectory to the thoracic wall and broncho-pleural fistula. There was also pneumomediastinum and signs of right lower lobe consolidation and pleural effusion (Fig. 1).
Due to the patient stability and exuberant radiologic findings, the patient was admitted for surveillance. A diagnosis of pleuro-parenchymal fistula and pneumomediastinum after thermal lung metastasis ablation was made.
The patient started large-spectrum antibiotics and chest drainage of the right lower pleural effusion was performed. After 3 weeks of antibiotics (Piperacillin-Tazobactam) and clinical improvement, a bronchoscopy was performed that confirmed a broncho-pleural fistula. Microbiologic cultures from the pleural fluid, sputum and bronchial lavage were negative. No respiratory failure was documented. The chest tube was removed after 3 days.
After 26 days, the patient was discharged with oral antibiotic treatment with Amoxicillin-Clavunate 875/125 mg until completion of 6 weeks treatment. No surgical intervention was necessary. Due to patient´s preference, limited respiratory function, technical impairments or age / comorbidities, surgery was not an option.
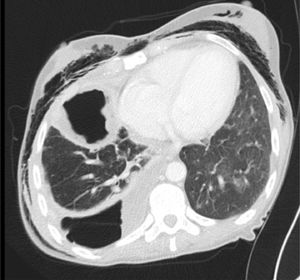
Follow-up CT at 2 months revealed marked improvement (Fig. 2) and the patient was able to return to daily activities with no residual symptoms.
Evolution of Chest CT findings. A- CT at admission with a right upper lobe (RUL) cavitary lesion with a chest wall fistula. Extensive subcutaneous emphysema. B- CT after 2 months, revealing improvement of the lung cavitation and fistula on the RUL and no subcutaneous emphysema. The metastatic lesion submitted to thermal ablation is not present.
Thermal ablation techniques include radiofrequency, microwave and cryotherapy, with the first being the most commonly used. A recent review estimated that the overall survival at 5 years after the procedure ranged from 32% to 65%, due to different criteria in terms of number of metastasis, location and ECOG status of patients.2 Chemotherapy-free survival is an important factor to take into account, with good results for thermal ablation in lung metastasis from colorectal cancer.3
The main complication reported is pneumothorax in up to 72% of procedures, leading to drainage in 13–47% of cases.4 One of the strategies to reduce complications is a better recognition of the indications: absence of extra-pulmonary metastasis and <3 pulmonary metastasis appears to be related to better patient outcomes.3–5 Other reports suggest that thermal ablation is an alternative particularly in patients with less than 5 metastasis and maximum size of 30 mm.4
Outcomes vary according to the primary tumor site.2,3 A review in colo-rectal metastasis revealed a good local control and prolonged time to systemic chemetherapy.4 Reports show that repeated ablation can improve local control.5,6
In this patient, endocrinology, oncology and radiology multidisciplinary assessment decided to perform thermal ablation due to persistent hypercalcemia despite denosumab, with two previous successful procedures managing to reduce serum calcium levels. The central location and size of the metastasis can explain the complication. Despite its exuberant presentation, a watchful strategy with antibiotics was preferred due to the risks associated with thoracic surgery or immediate bronchoscopy interventions. There was a progressive reduction of the cavity size and resolution of the pneumomediastinum and subcutaneous emphysema.
In conclusion, this case represents a potential fatal complication of thermal lung ablation and how a close follow-up, management and multidisciplinary discussion could prevent further complication. A careful selection of patients for thermal lung ablation is warranted.