Comorbidities are common in COPD and have been associated with reduced health status, increased health care utilization, all-cause hospitalization, and mortality. There is a scarcity of data on the relationship between comorbidities and functional capacity.
Objectiveto evaluate the impact of comorbidities on functional capacity of COPD patients.
Methodsa cross-sectional study was conducted at two teaching hospitals in Fortaleza, Brazil. The functional capacity was assessed by spirometry and the 6-min walking test (6MWT). The health status was assessed by the St. George's respiratory questionnaire (SGRQ) and the COPD assessment test (CAT). The sample was stratified as having “none”, “one” and “two or three” comorbidities groups. One-way ANOVA was used to compare means of the three groups and a multiple linear regression was run to predict the impact of comorbidities on 6MWT.
ResultsComorbidities (hypertension, coronary disease and diabetes) were found in 54% of the studied patients. The mean age of the 79 patients was 67±8 years and 55% were male. CAT scores increased from “no comorbidity” (17.9±7.7) to “one comorbidity” (22.8±6.8) and “two or three comorbidities” groups (24.2±10.2). A post hoc test showed a significant difference in the “no comorbidity” compared to the “two or three comorbidities” groups (p=0.01). The distance walked by the patients decreased from “no comorbidity” (386.1±83.2m) to “one comorbidity” (350±98m) and “two or three comorbidities” groups (312.6±91m). A post hoc test showed significant difference in the “no comorbidity” compared to “two or three comorbidities” groups (p=0.007). Numbers of comorbidities were independently associated with the 6MWT adjusting for age, severity of COPD and CAT scores.
Conclusionin the studied sample, the presence of comorbidities contributed to impair exercise capacity in patients with COPD.
Chronic obstructive pulmonary disease (COPD) is an important cause of impaired health-related quality of life, disability and death, with expressive social and economic repercussions.1 It is a complex disease with pulmonary and systemic symptoms, frequently associated with comorbidities2 that contribute to reduced health status and increased healthcare utilization, all-cause hospital admission, and mortality.3,4 The prevalence of the different types of comorbidity varies somewhat across studies, depending on the patient population, the definition of diseases and methods of patient evaluation.5
Hypertension, coronary disease and diabetes are frequent conditions associated with COPD and an increased risk of death.6,7 The presence of these comorbidities appears to have a deleterious effect on several outcomes in COPD.5
Endothelial dysfunction and increased arterial stiffness begin early in the course of COPD8–10 and probably represent the onset of atherosclerotic disease. Data from one study, including 20,269 subjects, identified a 40% prevalence of hypertension among 76 patients with COPD.7 Results from an observational study suggests that poorer health status, as indicated by a high COPD assessment test (CAT) score, may indicate the presence of certain comorbidities.11
There is a growing body of evidence from some studies evaluating the impact of comorbidities on 6-min walking test (6MWT). Most of these studies have included patients with anxiety and depression.12–15 Only one observational and longitudinal study has included 2164 patients with COPD associated with diabetes and cardiovascular disease.16
A better understanding of the impact of comorbidities, particularly diabetes, hypertension and cardiovascular disease, among patients with COPD is required. In the current study, we have evaluated the impact of comorbidities, diabetes, hypertension and cardiovascular disease, on functional performance in patients with COPD, after controlling for the effects of potential confounders including age, severity of COPD and health status.
MethodsPatients and study designA cross-sectional study was conducted at two teaching hospitals in Fortaleza, Brazil, from January to December 2012. The research protocol was approved by local Research Ethics Committee (no. 880/12), and a written informed consent was obtained in all 96 cases. Patients were recruited during their initial assessment prior to enrollment in a 97 pulmonary rehabilitation program in the ambulatories of both hospitals. The inclusion criteria were, to be smoker or ex-smoker with a smoking history of at least 10 packs-years, aged 40–80 years, a previous diagnosis of COPD on stages II–IV (post-bronchodilator FEV1/FVC<0.7 and FEV1<80% of predicted). All patients were clinically stable and without exacerbations for at least one month prior to recruitment.
Patients with a primary diagnosis of asthma or other chronic respiratory diseases, with severe cognitive deficiency preventing them from understanding the questionnaire and patients with restricted mobility, were excluded.
Assessment of patient's parametersSocio-demographic data were obtained through a structured questionnaire. Functional capacity was assessed by spirometry and 6MWT. The time allowed for patients to rest between the two tests was 1h.
Spirometry was conducted using an electronic spirometer in accordance with the guidelines of the American Thoracic Society/European Respiratory Society (ATS/ERS).17
Functional exercise capacity was assessed by 6MWT. It was performed twice in a 30m corridor. The patients were instructed to walk from end to end, covering as much ground as they could during the allotted time, as recommended by ATS guidelines.18
Health-related quality of life was assessed by St. George's respiratory questionnaire (SGRQ). The SGRQ consists of 53 items, which can be aggregated into an overall score and three domain scores describing symptoms, activity and impact.19 Current health was assessed by the COPD assessment test (CAT). This questionnaire consists of eight items that describe cough, phlegm, chest tightness, breathlessness going up hills/stairs, activity limitations at home, confidence leaving home, sleep and energy. Each item is scored from 0 to 5, thereby making the range of the total score from 0 to 40. Higher scores represent worse health.20 Both, SGRQ and CAT were previously translated and validated for the Portuguese language.21–23 The Brazilian version of SGRQ and CAT showed good psychometric properties. CAT showed an excellent inter-rater and intra-rater reliability (intraclass correlation coefficient [ICC]=0.96; 95% CI: 0.93–0.97; p<0.001; and ICC=0.98; 95% CI: 0.96–0.98; p<0.001, respectively).23 SGRQ showed an intraclass correlation ratio for the total score of α=0.79.21 Both questionnaires were administered in the mode of face-to-face interview, by the same interviewer and prior to the start of the rehabilitation program.
The diagnosis of the three studied comorbidities was based on data from medical records or upon clinical examination of patients. Subjects were classified as having diabetes if they reported a physician diagnosis of diabetes at baseline, or had impaired fasting or post-glucose load glucose levels (≥140mgdL−1) upon examination.
Subjects were classified as having coronary disease if they reported a previous physician diagnosis of myocardial infarction, angina or transient ischemic attacks, or when this information was registered in their medical records.
Subjects were classified as having hypertension if they reported a physician diagnosis of hypertension, were taking drugs for hypertension or had evidence of hypertension during a clinical examination (diastolic blood pressure ≥90mmHg or a systolic blood pressure ≥140mmHg, on three measurements). Each subject was classified as having none, one, two or three comorbidities.
Statistical analysesFor continuous variables, data are presented as means±standard deviation (SD) and for categorical variables, as percentage. Normality distribution for continuous variables was assessed by means of the Kolmogorov–Smirnov test. One-way ANOVA with the Bonferroni correction was used to compare the means of the three groups. For comparison of proportions, the χ2 test for linear trends was used. A multiple linear regression was run to predict the impact of comorbidities on 6MWT adjusting for age, severity of COPD and CAT scores. The p values less than 0.05 were considered significant. All statistical analyses were performed with SPSS for Windows version 10.0 (SPSS Inc., Chicago, IL).
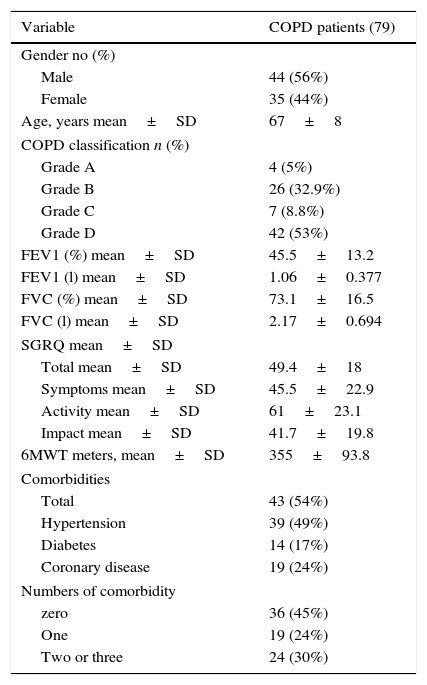
ResultsDemographic, clinical, respiratory function and functional exercise capacity of the 79 subjects studied are shown in Table 1. According the new GOLD classification (GOLD 2014),24 4 (5%) patients were in grade A, 26 (32.9%) in grade B, 7 (8.8%) in grade C and 42 (53%) in grade D.
Demographic, clinical and functional characteristics of 79 COPD patients.
| Variable | COPD patients (79) |
|---|---|
| Gender no (%) | |
| Male | 44 (56%) |
| Female | 35 (44%) |
| Age, years mean±SD | 67±8 |
| COPD classification n (%) | |
| Grade A | 4 (5%) |
| Grade B | 26 (32.9%) |
| Grade C | 7 (8.8%) |
| Grade D | 42 (53%) |
| FEV1 (%) mean±SD | 45.5±13.2 |
| FEV1 (l) mean±SD | 1.06±0.377 |
| FVC (%) mean±SD | 73.1±16.5 |
| FVC (l) mean±SD | 2.17±0.694 |
| SGRQ mean±SD | |
| Total mean±SD | 49.4±18 |
| Symptoms mean±SD | 45.5±22.9 |
| Activity mean±SD | 61±23.1 |
| Impact mean±SD | 41.7±19.8 |
| 6MWT meters, mean±SD | 355±93.8 |
| Comorbidities | |
| Total | 43 (54%) |
| Hypertension | 39 (49%) |
| Diabetes | 14 (17%) |
| Coronary disease | 19 (24%) |
| Numbers of comorbidity | |
| zero | 36 (45%) |
| One | 19 (24%) |
| Two or three | 24 (30%) |
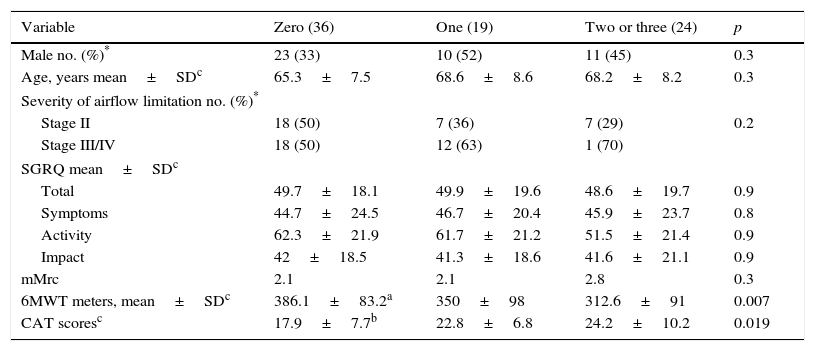
The mean age of the patients was 67±8 years and 44 (55%) were male. Fifty four percent of patients had at least one of three studied comorbidities. The sample was stratified as having “none”, “one” and “two or three” comorbidities groups. There was a significant difference between groups as determined by one-way ANOVA (Table 2). CAT scores increased from the “none” comorbidity group (17.9±7.7) to “one” comorbidity group (22.8±6.8) and “two or three” comorbidities group (24.2±10.2). A Bonferroni post hoc test revealed a significant difference in the “none” comorbidity group compared to the “two or three” comorbidities group (p=0.01).
Parameters of the 79 patients according to the number of comorbidity.
| Variable | Zero (36) | One (19) | Two or three (24) | p |
|---|---|---|---|---|
| Male no. (%)* | 23 (33) | 10 (52) | 11 (45) | 0.3 |
| Age, years mean±SDc | 65.3±7.5 | 68.6±8.6 | 68.2±8.2 | 0.3 |
| Severity of airflow limitation no. (%)* | ||||
| Stage II | 18 (50) | 7 (36) | 7 (29) | 0.2 |
| Stage III/IV | 18 (50) | 12 (63) | 1 (70) | |
| SGRQ mean±SDc | ||||
| Total | 49.7±18.1 | 49.9±19.6 | 48.6±19.7 | 0.9 |
| Symptoms | 44.7±24.5 | 46.7±20.4 | 45.9±23.7 | 0.8 |
| Activity | 62.3±21.9 | 61.7±21.2 | 51.5±21.4 | 0.9 |
| Impact | 42±18.5 | 41.3±18.6 | 41.6±21.1 | 0.9 |
| mMrc | 2.1 | 2.1 | 2.8 | 0.3 |
| 6MWT meters, mean±SDc | 386.1±83.2a | 350±98 | 312.6±91 | 0.007 |
| CAT scoresc | 17.9±7.7b | 22.8±6.8 | 24.2±10.2 | 0.019 |
SGRQ: St. George's respiratory questionnaire, mMRC: modified medical research council dyspnea scale, 6MWT: 6-min walking test, CAT: COPD assessment test.
The presence of comorbidities was associated with an increased CAT score for the items that assess the functional capacity. The score of activities items increased from 2.56±1.4 for “none” comorbidity group to 3.32±1.2 for “one” comorbidity group and 3.38±1.5 for “two or three” comorbidities group (p=0.04). For confidence and energy items the scores for groups “none”, “one” and “two or three” comorbidities were respectively 2.03±1.1; 2.63±1.2 and 3.04±1.5 (p=0.01) and 2.78±1.2; 3.58±1.1 and 3.67±1.4 (p=0.02).
The distance walked by the patients decreased from the “none” comorbidity group (386.1±83.2m) to the “one” comorbidity group (350±98m) and “two or three” comorbidities group (312.6±91m). A Bonferroni post hoc test showed significant difference in the “none” comorbidity group compared to “two or three” comorbidities group (p=0.007).
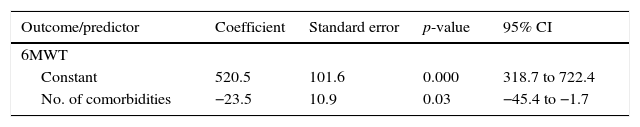
Each one of the three specific comorbidities had a similar impact on both exercise functional capacity as in CAT score. For cardiovascular disease, hypertension or diabetes the distance walked by the patients was respectively, 315±95.4m, 330±98.2m and 313.8±80.7m (p<0.05). The CAT scores were respectively, 23.7±10.5; 23.4±9.2 and 22.6±9.7 (p<0.05). Multiple linear regression analyses was built in order to investigate the influence of comorbidities on the 6MWT adjusting for age, severity of COPD and CAT scores A multiple linear regression model was built in order to investigate the influence of comorbidities in the 6MWT, after adjustment for age, severity of COPD and CAT score. The number of comorbidities was inversely associated with the distance walked during the 6MWT (Table 3).
Results of the stepwise multiple regression analyses of 79 patients with 6MWT as dependent variable.
| Outcome/predictor | Coefficient | Standard error | p-value | 95% CI |
|---|---|---|---|---|
| 6MWT | ||||
| Constant | 520.5 | 101.6 | 0.000 | 318.7 to 722.4 |
| No. of comorbidities | −23.5 | 10.9 | 0.03 | −45.4 to −1.7 |
Adjusted R2=0.117.
6MWT: 6-min walking test.
In this cross-sectional study, we found that 54% of patients with COPD, before starting the pulmonary rehabilitation program, had at least one of the three searched comorbidities. In a previous study, Crisafulli et al. reported very similar results (51%).25
The exercise capacity is currently considered an important parameter in the prediction of the risk of death from any cause and from respiratory causes among patients with COPD.26 This study showed that the presence of one or more comorbidities is associated with reduced exercise capacity in COPD patients. Our findings corroborated a recent study showing that heart trouble, hypertension and diabetes are associated with increased breathlessness and reduced 6-min walking distance.16 The assessment of exercise capacity by means of the 6MWT is frequently used in pulmonary and cardiac diseases. This is a simple, low cost and reproducible method to assess exercise capacity and it correlates closely with the daily activities of patients.27
Several comorbidities are associated with COPD. Among the frequently considered as relevant are included cardiovascular diseases, hypertension, lung cancer, diabetes cerebrovascular disease, muscle weakness, osteoporosis, anxiety and depression.28
Results of a large population-based study support the association between COPD and an increased incidence of cardiovascular disease.29
Due to the great number and high complexity of diseases associated with COPD we could not comprehensively address all comorbidities. Instead we focused on diabetes and cardiovascular disease since they are common and are associated with an increased frequency of relevant outcomes, including mortality and hospitalizations, in patients with COPD.7
The association between respiratory and cardiovascular diseases is a subject of research that has received a great deal of attention in recent years.30–33 Increased systemic inflammation in COPD patients with cardiac comorbidities supports the hypothesis of systemic inflammation as a potential mechanistic link between COPD and these comorbidities.28
The univariate analysis indicated that COPD subjects with one or more comorbidities had a significant higher CAT score than those without comorbidities. This is in agreement with the study of Miyazaki et al.11
Burger et al.27 in a cross-sectional study including 326 COPD patients, observed that anxiety and depression, but not cardiovascular disease and diabetes, are associated with low health-related quality of life assessed by SGRQ. In our study there was a lack of association of comorbidities with the SGRQ. The possible explanation is that Saint George is a specific questionnaire for respiratory diseases and does not directly evaluate “activity”, “confidence” and “energy”, items assessed in CAT and which showed strong correlation with functional exercise capacity.
The severity of airflow limitation was not generally associated with comorbidities. This result is in agreement with a longitudinal study including 2164 patients, performed by Miller et al.16, that failed to show association between comorbidities and severity of airflow limitation.
Some limitations of this study should be mentioned. This is a cross-sectional study with a convenience sample of patients with moderate to severe COPD. Subjects were recruited from two teaching hospitals and this may differ from COPD patients treated elsewhere. Due to the small sample size, a comparison of sub-groups GOLD stages II, III and IV, was not possible. The participants of this study were treated as considered best by their clinicians, so it was not possible to evaluate the influence of comorbidity treatment on the 6MWT.
Some strengths deserve be mentioned. This study used an objective and reproducible method for the assessment of functional exercise capacity (walked distance in the 6MWT) and well-defined criteria for comorbidities. In addition, our patients were homogenously distributed as to the severity of airflow limitation.
In summary, the presence of comorbidities contributed to impair functional exercise capacity in the patients studied. This finding reinforces the recommendation for a rigorous search for comorbidities in patients with COPD and functional exercise capacity impairment.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.