Bronchial foreign bodies are a rare condition in adults. In previous studies, only 6% of all airway foreign bodies occur in patients over 14 years of age.1
According to different series, 60–65% of the foreign bodies are located in the right main bronchus, 25–30% in the left main bronchus and 9–12% in the subglottis trachea. There is a similar distribution in pediatric patients. Within the adult population, the presence of foreign bodies in the airway has been reported more frequently in elderly patients, patients with mental health problems, and patients with swallowing problems.2
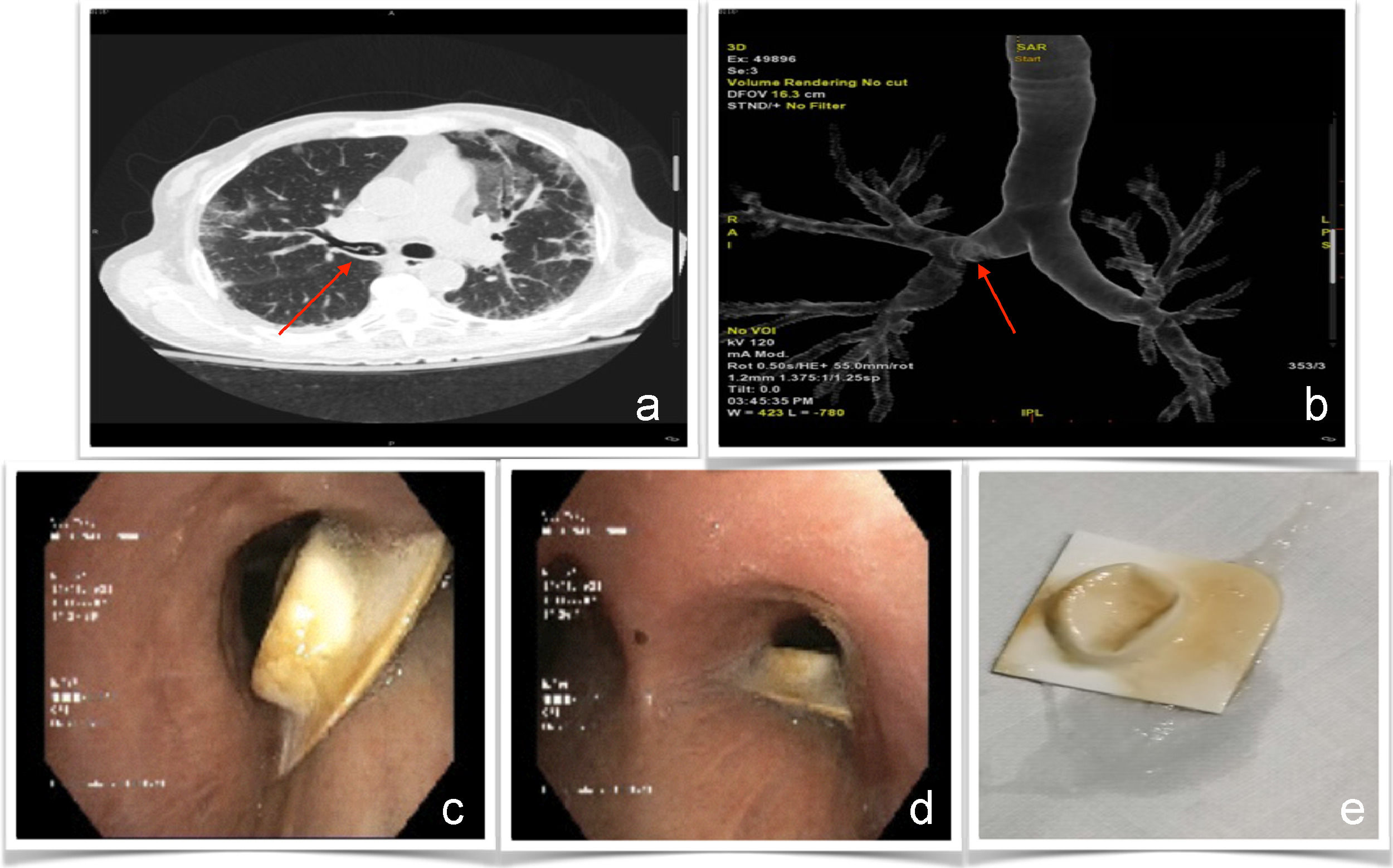
We present a 67-year-old patient who underwent a liver transplant in 2016. A computerized tomography (CT) scan (Lightspeed Pro 32 General Electric Healthcare, Chicago, USA) of the chest was made to study bilateral pulmonary infiltrates. In addition to areas with a crazy-paving pattern, a suspicious image of a foreign body was observed in the right main bronchus. For a better assessment, a 3D reconstruction was carried out. (Fig. 1a and b).
Image a. Visualization of the foreign body in thoracic CT (indicated by the arrow). Image b. Reconstruction of the bronchial tree with foreign body at the level of the right main bronchus (indicated by the arrow). Image c. Impacted foreign body in the right main bronchus with image from the main carina. Image d. Visualization of foreign body impacted at the entrance of the right main bronchus. Image e. Foreign body once removed by biopsy forceps.
Subsequently, bronchofibroscopy (Olympus BF H-190, Tokyo, Japan) was performed. A foreign body in the right main bronchus was observed, without alteration of the adjacent bronchial mucosa (Fig. 1c and Fig. 1d) and removed with biopsy forceps. Once outside, it was confirmed that the foreign body was a blister pack of a tablet (Fig. 1e).
The images are rare and surprising, first of all because this was an adult patient without swallowing or mental disorders. Secondly, despite the irritant and noxious nature of the material and the long time in the airway, no alteration in the bronchial mucosa was observed and the patient was asymptomatic. Finally, reviewing previous literature, this is the first case in which the presence of a pharmaceutical blister is described as a bronchial foreign body.
We want to particularly acknowledge Joy Selene Osorio for help in the translation of this article.
All authors have seen and approved the manuscript, contributed significantly to the work and declare that they have no conflicting interests that are relevant to this article. There are not organizations that have funded this research.